文章信息
- 侯珊珊, 吴毅凌, 罗炜, 尹欣, 孙中兴, 赵琦, 赵根明, 姜永根, 王娜, 姜庆五.
- Hou Shanshan, Wu Yiling, Luo Wei, Yin Xin, Sun Zhongxing, Zhao Qi, Zhao Genming, Jiang Yonggen, Wang Na, Jiang Qingwu
- 社区中老年人静坐行为与第1秒用力呼气容积下降的关联研究
- Association between sedentary behavior and force expiratory volume in 1 second reduction in middle-aged and elderly adults in communities
- 中华流行病学杂志, 2023, 44(7): 1092-1098
- Chinese Journal of Epidemiology, 2023, 44(7): 1092-1098
- http://dx.doi.org/10.3760/cma.j.cn112338-20221111-00963
-
文章历史
收稿日期: 2022-11-11
2. 上海市松江区疾病预防控制中心, 上海 201620
2. Songjiang District Center for Disease Control and Prevention, Shanghai 201620, China
慢性呼吸系统疾病(CRD),包括慢性阻塞性肺疾病(COPD)、支气管哮喘等,是中老年人群常见的慢性非传染性疾病。我国≥40岁人群COPD患病率为13.6%[1],总患病人数近1亿[2];哮喘患者超3 000万,给家庭和社会带来沉重负担[3]。肺功能检查作为COPD等多种呼吸系统疾病的必要检查之一,对于早期检出肺、气道病变,开展预防有重要公共卫生价值。第1秒用力呼气容积(FEV1)作为气流受限程度的指标,在COPD的分级[4]和支气管哮喘的诊断[5]中被广泛应用。FEV1[FEV1占预计值百分比(FEV1%Pred) < 80%][6]下降被认为与COPD早期发展密切相关[7],队列研究表明,基线FEV1下降者患COPD的风险是正常者的3倍以上(26% vs. 7%)。
静坐行为是在清醒状态下,长时间保持坐或靠的姿势[8]。流行病学研究显示,静坐行为与糖尿病、心血管疾病等不良健康结局以及全死因死亡相关[9-10],更是COPD死亡的独立预测因素[11]。但静坐行为与社区人群,尤其≥40岁CRD重点人群肺功能的关联尚缺乏系统研究。本研究旨在了解上海郊区自然人群队列中≥40岁社区居民的静坐行为和FEV1状况,进而探讨静坐行为与FEV1下降的关联,为社区中老年人群的CRD预防提供参考依据。
对象与方法1. 研究对象:上海郊区自然人群队列于2016年在上海市松江区对69 116名20~74岁居民开展基线调查[12]。2021年7-9月,本研究在此基础上随机选取3 381名研究对象参与调查。纳入标准:①年龄≥40岁(截至2021年6月30日);②队列基线信息完整;③无肺功能检查和支气管扩张检查的禁忌症[13-14];④知情同意。剔除肺功能检查质量不合格者[13](129名)及问卷数据缺失者(68名)后,共纳入3 121名研究对象。本研究通过复旦大学公共卫生学院医学研究伦理委员会批准(批准文号:IRB#2021-03-0883)。
2. 研究方法:①问卷调查:调查员现场使用电子问卷进行面对面调查;在队列基线时使用国际体力活动调查问卷(IPAQ)中文版短问卷采集研究对象一周各种体力活动水平和静坐行为的频率及每日累计时间[15]。②体格检查:使用统一的身高体重仪,采集体重及净足身高,并计算BMI(kg/m²)。③肺功能检查:使用优呼吸肺功能检测仪(PF680,浙江亿联康医疗科技有限公司),及配套优呼吸肺功能检测综合管理系统(系统)进行。系统根据性别、年龄、身高和体重数据生成FEV1预计值。肺功能检查操作规范、读数、检查质量判定依据《肺功能检查指南(第二部分)——肺计量检查》进行[13],取各次吹气中最大FEV1值,计算其与FEV1预计值之比值,即为FEV1%Pred;FEV1与最大用力肺活量(FVC)之比为FEV1/FVC。
对FEV1/FVC < 70%者进行支气管舒张试验:医师遵循《肺功能检查指南(第四部分)——支气管舒张试验》建议评估受试者基础情况后[14],给予吸入沙丁胺醇,静坐15~20 min后,再次进行肺功能检测。
3. 相关指标定义:①静坐行为:清醒状态下以坐姿或卧姿进行的行为[8]。通过IPAQ短问卷采集问题“你通常每天多少时间坐着或靠着?(包括工作、居家、乘坐交通工具、业余休闲时,但不包括睡觉时间)”获得。以每日静坐时间上四分位数为截断值分为 > 5 h及≤5 h组。②完全静坐行为:将一周内无报告任何中或重度体力活动水平的研究对象定义为完全静坐组,其余为非完全静坐行为组[15]。③FEV1下降:将FEV1%Pred < 80%定义为下降组,≥80%定义为正常组[6]。④体力活动水平、锻炼强度的计算与分级:根据IPAQ建议,计算调查对象每周体力活动水平[代谢当量(MET)-min/周],并综合考虑每周体力活动天数,将调查对象分为高、中、低组[16];并依据对中老年人的运动建议[17],将体力活动水平≥600 MET-min/周定义为达标组,< 600 MET-min/周为未达标组。⑤患COPD或支气管哮喘:由经验丰富的临床医生结合症状、肺功能检查结果,排除其他鉴别诊断后判定[4-5]。⑥患呼吸系统疾病家族史:自报直系亲属曾患支气管哮喘、慢性支气管炎、肺气肿及COPD。⑦共患其他慢性病:自报患有心脑血管疾病、恶性肿瘤、糖尿病与代谢性疾病。
4. 质量控制:严格按照《肺功能检查指南(第二部分)——肺量计检查》[13]及《常规肺功能检查基层指南(2018年)》[6]要求进行仪器校准、肺功能检查和结果判定,所有技术人员经过全面系统的培训。
5. 统计学分析:依据IPAQ建议对资料进行异常值剔除和数据截断[16]。每日静坐时间、BMI、FEV1%Pred等偏态定量资料用M(Q1,Q3)表示,多组间比较使用Kruskal-Wallis检验,使用方差分析检验组间差异;使用χ²检验比较基本特征的组间差异。鉴于FEV1受性别及年龄的影响较大[18],在综合考虑各层样本量后,将研究人群分为4个亚组,即 < 60岁男性、≥60岁男性、< 60岁女性、≥60岁女性。在总人群及每个亚组中,使用广义加性模型进行多因素回归分析:以FEV1是否下降作为因变量;以完全静坐行为(是vs.否)、每日静坐时间(连续变量)、静坐时间分组(> 5 h/d vs.≤5 h/d)作为自变量分别纳入方程;协变量包括年龄、BMI及其他CRD相关因素。其中年龄和BMI与因变量呈非线性相关,使用光滑样条函数处理后作为连续变量纳入。使用R 4.1.3软件进行数据清理和分析。双侧检验,检验水准α=0.05。
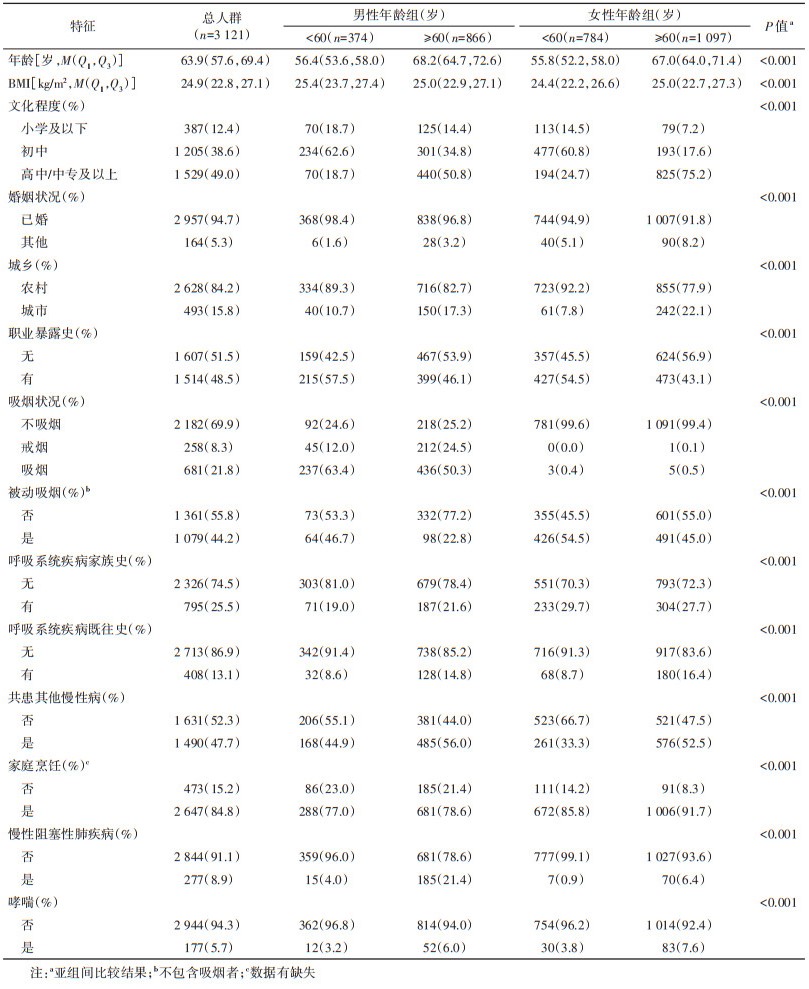
结果1. 基本特征:3 121名研究对象年龄M(Q1,Q3)为63.9(57.6,69.4)岁,BMI、文化程度、婚姻状况、职业暴露史、吸烟状况、呼吸系统疾病既往史、呼吸系统疾病家族史、家庭烹饪等变量在不同亚组间的分布差异均有统计学意义(P < 0.05)。见表 1。
2. 各亚组完全静坐行为和每日静坐时间分布:FEV1下降者占所有研究对象的14.8%,其中≥60岁男性的FEV1下降占比(26.0%)显著高于其他亚组(P < 0.05)。完全静坐行为者占所有研究对象的24.8%。男性各亚组高于女性,≥60岁组完全静坐行为者占比低于 < 60岁组,但差异均无统计学意义(P > 0.05)。各组完全静坐行为占比和锻炼强度差异无统计学意义(P > 0.05),但≥60岁女性静坐时间 > 5 h/d组占比显著高于 < 60岁男性(23.1% vs. 13.4%)。见表 2。
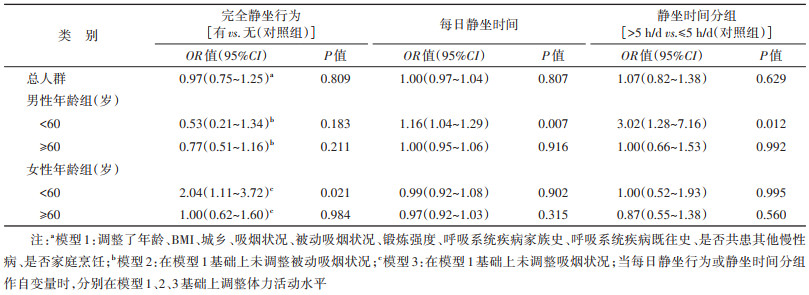
3. 完全静坐行为及每日静坐时间与FEV1下降关联的多因素分析:在 < 60岁女性中,完全静坐行为组FEV1下降是非完全静坐行为组的2.04(95%CI:1.11~3.72)倍。但这一关联在其他年龄、性别亚组的人群中并不显著(P > 0.05)。< 60岁男性中,FEV1下降比例随每日静坐时间增加而上升(OR=1.16,95%CI:1.04~1.29);静坐时间 > 5 h/d者与FEV1下降的关联是≤5 h/d组的3.02(95%CI:1.28~7.16)倍。而在 < 60岁女性中,FEV1下降与每日静坐时间增加之间无统计学关联(P > 0.05)。≥60岁男性及女性亚组FEV1下降与完全静坐行为、每日静坐时间增加之间无统计学关联(P > 0.05)。见表 3。
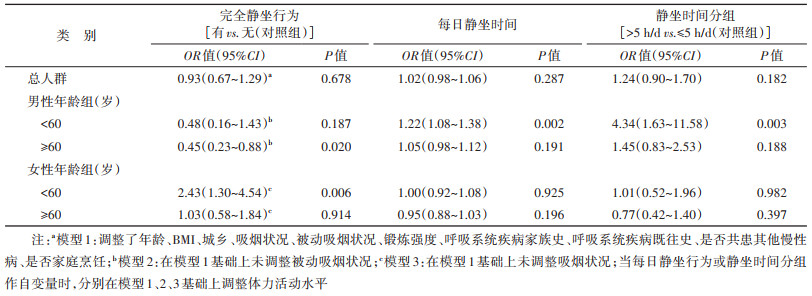
4. 敏感性分析:剔除COPD及支气管哮喘患者后,< 60岁女性和男性的FEV1下降分别与完全静坐行为、每日静坐时间增加显著相关(P < 0.05),与多因素分析结论相同。见表 4。在≥60岁男性组被剔除的316名患者中有100名FEV1下降且无完全静坐行为,使该组FEV1下降人群中完全静坐行为者的比例由20.9%下降至13.3%,可能是该组敏感性分析中,完全静坐行为与FEV1下降呈负相关(OR=0.45,95%CI:0.23~0.88)的原因。
本研究基于上海郊区自然人群队列,探讨≥40岁社区居民静坐行为特征,及其与肺功能之间的关联。结果表明 < 60岁人群中,女性的完全静坐行为和男性的每日静坐时间增加均与FEV1下降显著相关,且该效应独立于体力活动。
肺功能检查是多种CRD诊断和分级的必要依据[4-5],FEV1%Pred是气流受限的敏感指标,对阻塞性通气障碍、COPD严重程度分级等有指示意义[4, 7]。低FEV1%Pred与多种血清学改变、COPD的恶病质之间存在机制关系链[19-20],低FEV1者有更高风险发展为COPD,应尽早采取干预措施,预防或延缓FEV1的下降[7]。目前少有聚焦于疾病早期乃至非CRD人群的低FEV1%Pred影响因素研究。本研究中有14.8%的我国上海市松江区≥40岁社区人群FEV1下降,与日本相关研究结果(15.8%)相近[21]。FEV1与吸烟、衰老和性别等密切相关,但相关危险因素对不同人群的FEV1影响差异较大,如15~29岁人群中,吸烟量≥20包年者FEV1下降可能是 < 20包年者的81.8倍,而60~82岁人群中,此因素的OR值仅为2.9[22],本研究同样提示,不同年龄、性别亚组FEV1下降比例差异颇大,有必要开展亚组分析。
静坐行为的发生率不断上升,本研究中24.8%的研究对象存在完全静坐行为。其他大型队列研究也显示,83.3%的队列成员每日静坐时间 > 2.0 h[23],另有研究通过加速度计测量出成年人每日静坐时间可达7.7 h[24]。静坐行为带来一系列健康问题,与心血管疾病、糖尿病和全死因死亡显著相关[9-11],影响CRD的健康结局,如死亡和生命质量等[25-26],本研究中 < 60岁人群的FEV1下降与静坐行为相关,在 < 60岁女性中与完全静坐行为,即中、高强度体力活动水平的缺失显著相关;在40~59岁男性人群中与每日静坐时间的增加显著关联。且这些关联独立于体力活动,与其他国内外研究一致[27-28]。
基于本研究发现,建议≥40岁人群在定期肺功能检查及戒烟、加强锻炼等的基础上[4],使居民避免完全静坐行为、减少静坐时间。鉴于气道阻塞本身会加速FEV1下降[19]、肺功能受损非完全可逆,干预应尽早进行。但目前各国CRD的临床诊疗指南仅9%提出了减少静坐行为的建议[29],应加强相关研究,提供更多科学证据。
本研究基于社区人群,对3 121名≥40岁中老年人逐一开展肺功能检测,样本量较大,并采用标准化问卷对静坐行为进行定义和分析,结果可信。本研究存在局限性。第一,采用自我报告评价静坐时间和体力活动水平。研究表明IPAQ会低估受访者的体力活动水平,但对每日静坐时间与加速度计测量结果无显著差异[30],因此本研究结果可信,后续可采用多种方式测量静坐行为。第二,未能对静坐行为进行多次动态评价,但鉴于中老年人运动及静坐行为习惯较为稳定,可能产生的影响相对有限。第三,未对每日静坐时间的构成进一步分析,如因工作、娱乐等导致的静坐与活动能力不足导致的静坐对健康的影响是否存在差别等。第四,本研究基于单次肺功能检测,后续可在前瞻性研究中结合肺功能改变进一步论证。
综上所述,本研究通过分析不同的性别、年龄亚组中FEV1下降与完全静坐行为、每日静坐时间增加的关联,提示在肺功能健康的防治中,女性应注重适当增加中、高强度体力活动水平,以避免完全静坐行为;男性亦可通过增加运动等减少每日静坐时间,且静坐行为的干预应尽早进行。
利益冲突 所有作者声明无利益冲突
作者贡献声明 侯珊珊:酝酿和设计实验、实施研究、数据采集和分析、论文撰写;吴毅凌、罗炜:酝酿和设计实验、实施研究、数据采集、经费支持;尹欣:酝酿和设计实验、实施研究、数据采集;孙中兴、赵琦、赵根明、姜永根、姜庆五:酝酿和设计实验;王娜:酝酿和设计实验、技术支持和指导、经费支持
| [1] |
Fang LW, Gao P, Bao HL, et al. Chronic obstructive pulmonary disease in China: a nationwide prevalence study[J]. Lancet Respir Med, 2018, 6(6): 421-430. DOI:10.1016/S2213-2600(18)30103-6 |
| [2] |
Wang C, Xu JY, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health study): a national cross-sectional study[J]. Lancet, 2018, 391(10131): 1706-1717. DOI:10.1016/S0140-6736(18)30841-9 |
| [3] |
胡善联, 饶克勤, 高军, 等. 中国居民常见疾病的经济负担[C]//中华预防医学会第二届学术年会暨全球华人公共卫生协会第二届年会论文集. 香河: 中华预防医学会, 2006. Hu SL, Rao KQ, Gao J, et al. The economic burden of common diseases among Chinese residents[C]//The 2nd annual academic conference of the Chinese Society of Preventive Medicine and the 2nd annual conference of the global Chinese public health association. Xianghe: Chinese Preventive Medicine Association, 2006. |
| [4] |
中华医学会呼吸病学分会慢性阻塞性肺疾病学组, 中国医师协会呼吸医师分会慢性阻塞性肺疾病工作委员会. 慢性阻塞性肺疾病诊治指南(2021年修订版)[J]. 中华结核和呼吸杂志, 2021, 44(3): 170-205. DOI:10.3760/cma.j.cn112147-20210109-00031 Chronic Obstructive Pulmonary Disease Group of Chinese Thoracic Society, Chronic Obstructive Pulmonary Disease Committee of Chinese Association of Chest Physician. Guidelines for the diagnosis and management of chronic obstructive pulmonary disease (revised version 2021)[J]. Chin J Tuberc Respir Dis, 2021, 44(3): 170-205. DOI:10.3760/cma.j.cn112147-20210109-00031 |
| [5] |
中华医学会呼吸病学分会哮喘学组. 支气管哮喘防治指南(2020年版)[J]. 中华结核和呼吸杂志, 2020, 43(12): 1023-1048. DOI:10.3760/cma.j.cn112147-20200618-00721 Asthma Group of Chinese Society. Guidelines for bronchial asthma prevent and management (2020 edition) Asthma group of Chinese Throacic society[J]. Chin J Tuberc Respir Dis, 2020, 43(12): 1023-1048. DOI:10.3760/cma.j.cn112147-20200618-00721 |
| [6] |
中华医学会, 中华医学会杂志社, 中华医学会全科医学分会, 等. 常规肺功能检查基层指南(2018年)[J]. 中华全科医师杂志, 2019, 18(6): 511-518. DOI:10.3760/cma.j.issn.1671-7368.2019.06.003 Chinese Medical Association, Chinese Medical Journals Publishing House, Chinese Society of General Practice, et al. Guideline for pulmonary function testing in primary care (2018)[J]. Chin J Gen Pract, 2019, 18(6): 511-518. DOI:10.3760/cma.j.issn.1671-7368.2019.06.003 |
| [7] |
Jakeways N, McKeever T, Lewis SA, et al. Relationship between FEV1 reduction and respiratory symptoms in the general population[J]. Eur Respir J, 2003, 21(4): 658-663. DOI:10.1183/09031936.03.00069603 |
| [8] |
Hernández-Vicente A, Vicente-Rodríguez G, Gómez- Cabello A, et al. Physical Exercise[M]. Oxford: Academic Press, 2020.
|
| [9] |
Petersen CB, Bauman A, Grønbæk M, et al. Total sitting time and risk of myocardial infarction, coronary heart disease and all-cause mortality in a prospective cohort of Danish adults[J]. Int J Behav Nutr Phys Act, 2014, 11(1): 13. DOI:10.1186/1479-5868-11-13 |
| [10] |
Chau JY, Grunseit AC, Chey T, et al. Daily sitting time and all-cause mortality: a meta-analysis[J]. PLoS One, 2013, 8(11): e80000. DOI:10.1371/journal.pone.0080000 |
| [11] |
Furlanetto KC, Donária L, Schneider LP, et al. Sedentary behavior is an independent predictor of mortality in subjects with COPD[J]. Respir Care, 2017, 62(5): 579-587. DOI:10.4187/respcare.05306 |
| [12] |
赵琦, 刘星, 姜永根, 等. 上海郊区自然人群队列和生物样本库建设[J]. 中华流行病学杂志, 2023, 44(1): 28-33. DOI:10.3760/cma.j.cn112338-20221018-00888 Zhao Q, Liu X, Jiang YG, et al. Establishment of Shanghai suburban adult cohort and biobank[J]. Chin J Epidemiol, 2023, 44(1): 28-33. DOI:10.3760/cma.j.cn112338-20221018-00888 |
| [13] |
中华医学会呼吸病学分会肺功能专业组. 肺功能检查指南(第二部分)——肺量计检查[J]. 中华结核和呼吸杂志, 2014, 37(7): 481-486. DOI:10.3760/cma.j.issn.1001-0939.2014.07.001 Pulmonary Function Professional Group, Chinese Thoracic Society, Chinese Medical Association. Guidelines for pulmonary function tests (Part Ⅱ)-spirometry[J]. Chin J Tuberc Respir Dis, 2014, 37(7): 481-486. DOI:10.3760/cma.j.issn.1001-0939.2014.07.001 |
| [14] |
中华医学会呼吸病学分会肺功能专业组. 肺功能检查指南(第四部分)——支气管舒张试验[J]. 中华结核和呼吸杂志, 2014, 37(9): 655-658. DOI:10.3760/cma.j.issn.1001-0939.2014.09.007 Pulmonary Function Professional Group, Chinese Thoracic Society, Chinese Medical Association. Guidelines for pulmonary function tests (Part Ⅳ)-Bronchodilator test[J]. Chin J Tuberc Respir Dis, 2014, 37(9): 655-658. DOI:10.3760/cma.j.issn.1001-0939.2014.09.007 |
| [15] |
叶真, 胡如英, 沈玉华, 等. 静坐行为和时间与代谢综合征相关性研究[J]. 中华内分泌代谢杂志, 2013, 29(9): 756-760. DOI:10.3760/cma.j.issn.1000-6699.2013.09.005 Zhen Y, Hu RY, Shen YH. et al. Association of sedentary behavior and time with risk of metabolic syndrome[J]. Chin J Endocrinol Metab, 2013, 29(9): 756-760. DOI:10.3760/cma.j.issn.1000-6699.2013.09.005 |
| [16] |
樊萌语, 吕筠, 何平平. 国际体力活动问卷中体力活动水平的计算方法[J]. 中华流行病学杂志, 2014, 35(8): 961-964. DOI:10.3760/cma.j.issn.0254-6450.2014.08.019 Fan MY, Lyu J, He PP. Chinese guidelines for data processing and analysis concerning the international physical activity questionnaire[J]. Chin J Epidemiol, 2014, 35(8): 961-964. DOI:10.3760/cma.j.issn.0254-6450.2014.08.019 |
| [17] |
《中国人群身体活动指南》编写委员会. 中国人群身体活动指南(2021)[J]. 中华流行病学杂志, 2022, 43(1): 5-6. DOI:10.3760/cma.j.cn112338-20211119-00903 Composing and Editorial Board of Physical Activity Guidelines for Chinese. Physical activity guidelines for Chinese (2021)[J]. Chin J Epidemiol, 2022, 43(1): 5-6. DOI:10.3760/cma.j.cn112338-20211119-00903 |
| [18] |
赵蓉雅, 朱蕾, 李丽, 等. 1988年上海地区成人肺功能正常预计值公式的适用性检验[J]. 中华结核和呼吸杂志, 2011, 34(8): 586-589. DOI:10.3760/cma.j.issn.1001-0939.2011.08.012 Zhao RY, Zhu L, Li L, et al. The applicability of the 1988 version of the prediction equations for adult normal lung function in Shanghai[J]. Chin J Tuberc Respir Dis, 2011, 34(8): 586-589. DOI:10.3760/cma.j.issn.1001-0939.2011.08.012 |
| [19] |
Mokari-Yamchi A, Jabbari M, Sharifi A, et al. Low FEV1 is associated with increased risk of Cachexia in COPD patients[J]. Int J Chron Obstruct Pulmon Dis, 2019, 14: 2433-2440. DOI:10.2147/COPD.S221466 |
| [20] |
Adair D, Lugogo N, Yosef M, et al. High IL6 asthma is associated with lower FEV1 and greater likelihood of metabolic dysfunction[J]. Am J Respir Crit Care Med, 2020, 201: A2740. |
| [21] |
Masuko H, Sakamoto T, Kaneko Y, et al. Lower FEV1 in non-COPD, nonasthmatic subjects: association with smoking, annual decline in FEV1, total IgE levels, and TSLP genotypes[J]. Int J Chron Obstruct Pulmon Dis, 2011, 6: 181-189. DOI:10.2147/COPD.S16383 |
| [22] |
Breyer-Kohansal R, Faner R, Breyer MK, et al. Factors associated with low lung function in different age bins in the general population[J]. Am J Respir Crit Care Med, 2020, 202(2): 292-296. DOI:10.1164/rccm.202001-0172LE |
| [23] |
樊萌语, 吕筠, 郭彧, 等. 中国慢性病前瞻性研究: 10个项目地区成人体力活动和休闲静坐时间特征差异的分析[J]. 中华流行病学杂志, 2015, 36(8): 779-785. DOI:10.3760/cma.j.issn.0254-6450.2015.08.002 Fan MY, Lyu J, Guo Y, et al. Regional differences on patterns of physical activity and leisure sedentary time: findings from the China Kadoorie Biobank study, including a million people from 10 regions[J]. Chin J Epidemiol, 2015, 36(8): 779-785. DOI:10.3760/cma.j.issn.0254-6450.2015.08.002 |
| [24] |
Owen N, Healy GN, Matthews CE, et al. Too much sitting: the population health science of sedentary behavior[J]. Exer Sport Sci Rev, 2010, 38(3): 105-113. DOI:10.1097/JES.0b013e3181e373a2 |
| [25] |
Mckeough Z, Cheng SN, Alison J, et al. Associations of sedentary behaviour and physical activity phenotypes with health outcomes in COPD: a cohort study[J]. Eur Respir J, 2018, 52(Suppl 62): OA1981. DOI:10.1183/13993003.congress-2018.OA1981 |
| [26] |
Atkins CP, Baxter M, Jones AP, et al. Measuring sedentary behaviours in patients with idiopathic pulmonary fibrosis using wrist-worn accelerometers[J]. Thorax, 2016, 71(Suppl 3): A238-A239. DOI:10.1136/thoraxjnl-2016-209333.420 |
| [27] |
Watz H, Waschki B, Boehme C, et al. Extrapulmonary effects of chronic obstructive pulmonary disease on physical activity: a cross-sectional study[J]. Am J Respir Crit Care Med, 2008, 177(7): 743-751. DOI:10.1164/rccm.200707-1011OC |
| [28] |
Lei YL, Zou K, Xin JG, et al. Sedentary behavior is associated with chronic obstructive pulmonary disease: A generalized propensity score-weighted analysis[J]. Medicine, 2021, 100(18): e25336. DOI:10.1097/MD.0000000000025336 |
| [29] |
Lewthwaite H, Effing TW, Olds T, et al. Physical activity, sedentary behaviour and sleep in COPD guidelines: A systematic review[J]. Chron Respir Dis, 2017, 14(3): 231-244. DOI:10.1177/1479972316687224 |
| [30] |
屈宁宁, 李可基. 国际体力活动问卷中文版的信度和效度研究[J]. 中华流行病学杂志, 2004, 25(3): 265-268. DOI:10.3760/j.issn:0254-6450.2004.03.021 Qu NN, Li KJ. Study on the reliability and validity of international physical activity questionnaire (Chinese Vision, IPAQ)[J]. Chin J Epidemiol, 2004, 25(3): 265-268. DOI:10.3760/j.issn:0254-6450.2004.03.021 |
 2023, Vol. 44
2023, Vol. 44