2. Department of Ophthalmology, the First Hospital of Jilin University, Changchun 130021, China;
3. Department of Radiology, the First Hospital of Jilin University, Changchun 130021, China
Yunqian Li, Professor, Deputy Director of Neurosurgery of the First Hospital of Jilin University, is a chief physician and a supervisor of Postdoctoral Fellows. He obtained a PhD degree from Jilin University in 2012. He was also a Postdoctoral Fellow, studying brain tumors, at the Department of Bethune Medical School of Jilin University in 2006–2007. He is a member of the standing committee of the Chinese Medical Doctor Association of Jilin Province Professional Committee of Neurosurgery, youth member of the Neurological Surgery Branch of the Chinese Medical Association, deputy director of the Chinese Council for the Promotion of the Health Care International Exchange of Neurosurgery Section, and won the Chinese Neurosurgeons' Zhong-Cheng Wang "young physician award" in 2016. Engaged in neurosurgery work for nearly 20 years, he is skilled in the diagnosis and treatment of all kinds of brain and spinal cord tumors. He has published more than 70 papers, and has hosted and participated in more than 10 national and provincial scientific research projects.
Intrasellar cavernous hemangioma is difficult to diagnosis. It is a rare vascular lesion of the sellar region. Moreover, the clinical features of its mass effect can resemble a pituitary adenoma. Herein, we present a patient with a contrast-enhancing lesion in the sella turcica and part of the lesion in the right cavernous sinus. Surgery was performed under the assumption that it was a nonfunctional pituitary macroadenoma and the histopathological diagnosis was cavernous hemangioma.
2 Case reportA 64-year-old postmenopausal woman presented with intermittent headache attacks over 10 years and slowly progressive decreased vision of both eyes for about 1 year. Neurological examination revealed a bitemporal visual field deviation and both pupils had a normal light reflex. She had no history of decreased libido, weight gain, fatigue, cold intolerance, or symptoms of hypocortisolemia. Her prolactin level was 746.12 mUI/L (normal range 70.81-566.5 mUI/L) but without lactation, and thyroid-stimulating hormone levels and follicle-stimulating hormone, luteinizing hormone, testosterone, and growth hormone levels were all normal.
The patient had no previous history of cerebrovascular accidents or major systemic disease. Her serum biochemistry were all unremarkable. Brain magnetic resonance imaging (MRI) showed an enlarged pituitary fossa and an irregular solid tumor (33 mm × 22 mm × 22 mm) in the sella turcica and parasellar region. The pituitary stalk was not visible and the optic chiasm was elevated. The tumor invaded the right cavernous sinus and compressed and encased the cavernous portion of the internal carotid artery. The right temporal lobe was also compressed.
The lesion appeared iso-intense to gray matter on T1-weighted images (Figures 1a and 1d) and hyperintense on T2-weighted images (T2WI) (Figures 1b and 1e) and enhanced homogenously after gadolinium injection (Figures 1c and 1f). This imaging appearance was consistent with a pituitary macroadenoma. On T1-weighted MRI, the lesion was iso-intense or hypointense to grey matter and enhanced homogeneously after contrast administration. Suspecting a nonfunctioning pituitary macroadenoma, a transseptal transsphenoidal approach was used to remove the sellar tumor.
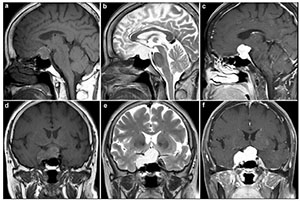
|
| Figure 1 Preoperative MRI revealed a large tumor in the sella turcica. a. The tumor has marked iso-intensity on a T1-weighted image in a sagittal view. b. The tumor has marked hyperintensity on a T2-weighted image in a sagittal view. c. The tumor is brightly enhanced in a sagittal view. d. The tumor has marked iso-intensity on a T1-weighted image in a coronal view. e. The tumor shows marked hyperintensity on a T2-weighted image in a coronal view. f. The tumor is brightly enhanced in a coronal view. |
A tough lesion with a dark-red surface and a firm and highly vascular structure of the tumor contrasted with most pituitary adenomas. There was profuse bleeding during the surgical procedure. Pathological examination revealed that the lesion consisted of multiple vessels, filled with red cells, with a large lumen and thin walls, and some of the vessels were filled with organized thrombi (Figures 2a and 2b). Follow-up CT showed the lesion to be smaller (Figures 2c and 2d). Postoperatively, her visual acuity became better. Stereotactic radiosurgery was recommended, but the patient refused it.
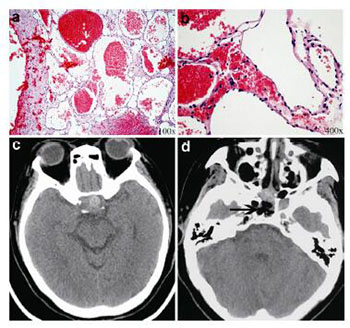
|
| Figure 2 Post-operative histological and imaging examinations (a, b). On histologic examination, the mass is composed of dilated vessels occasionally containing thrombi (a, hematoxylin and eosin [H & E] stain, ×100; b, H & E stain, ×400). (c, d) Post-operative CT imaging. |
Cavernous hemangioma is defined as malformations of the microcirculation, which are different from neoplasms. It originates from any intracranial region, accounts for 5%-13% of vascular malformations, and occurs in approximately 0.5%-1% of the population[1]. When it occurs in the cerebral hemispheres, seizures and bleeding caused by cavernous hemangioma are typical, while in the sella, seizures are rare but a mass effect is often notable.
Its pathological features are described as berry-like collections of vascular spaces that are lined by thin walls devoid of smooth muscle, and there is no intervening glial tissue between the vascular spaces. Thus, the vascular tissue in cavernous hemangioma is anelastic and easily thromboplastic. Electron microscopy shows that the tight junctions of endothelial cells appear to have abnormal gaps. That may be the reason for blood leakage.
Extra-cerebral cavernous hemangioma is mostly located in the middle cranial fossa, including the parasellar, the intrasellar, and the clivus region. However, an intrasellar cavernous hemangioma is rare, and a parasellar is even more so. The difference between them is the main location of the tumor mass.
Our literature review identified 8 cases of intrasellar cavernous hemangioma (Table 1)[1-5]. All of them were confirmed by pathology, and the mass was completely located in the sella turcica in only 2 of 8 cases, while others extended into the suprasellar cistern and cavernous sinus and encompassed the internal carotid. This may be another difficult factor for total resection.
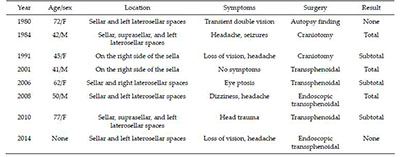
|
Remarkably, the first case was diagnosed by autopsy findings, and after 2000, all patients were operated on via the transsphenoidal approach. In the case reported by Chuang et al., cavernous hemangioma was not detected by cerebral angiography[4]. Hori et al. reported that stereotactic radiosurgery was effective for treating cavernous hemangioma[5].
In our case, the major part of the lesion was located in the sellar fossa with right and upward extension. The clinical features presented as bitemporal hemianopia due to optic chiasm elevation, and mildly increased prolactin levels due to a pituitary stalk effect.
MRI is more specific and sensitive than cerebral angiography and computed tomography in the diagnosis of cavernous hemangioma. On angiography, most cavernous hemangioma cannot be detected. On MRI, cavernous hemangioma has the following characteristics: well-defined borders, brightly hyperintense on T2WI images, and two pattern enhancement with a rapid homogeneous enhancement and a progressive enhancement. The contrast agent fills the peripheral part of the lesion in the early stage of dynamic contrast-enhanced scanning and then slowly fills the entire lesion[2]. In addition, most pituitary adenomas are hypointense to iso-intense to the normal gland and cerebral cortex on T1-weighted MRI scans and of variable intensity on T2-weighted sequences. On MRI, they are similar. That is why cavernous hemangioma in the sella turcica is difficult to diagnose pre-operatively.
With complete resection, cavernous hemangioma can be curable. In particular, the total mass of cavernous hemangioma located in the sellar fossa could be removed completely with the development of an endoscopic transsphenoidal approach[6]. In these operations, obstructing the blood supply to cavernous hemangioma is vital to reduce the risk of bleeding and allow for total removal of the lesion.
Numerous methods of reducing tumor size and vascularity have been suggested to minimize blood loss during resection of these highly vascular tumors. However, radiosurgery is preferred because of its good outcomes with lower morbidity and a lower risk of hemorrhage after treatment of cavernous hemangioma[7]. Considering the high risk of bleeding in surgery and the good response to radiosurgery of cavernous hemangioma, we only performed debulking in our patient.
4 ConclusionTranssphenoidal approach surgery should be applied for decompression of the optic nerve and biopsy, and stereotactic radiosurgery is effective and preferred for cavernous hemangioma treatment.
Conflict of interests
All contributing authors have no conflict of interests.
| [1] | Cobbs CS, Wilson CB. Intrasellar cavernous hemangioma. Case report. J. Neur., 2001, 94(3): 520–522. |
| [2] | Lee DM, Yu SH, Yoon HH, Lee KL, Eom YS, Lee K, Kim BJ, Kim YS, Park IeB, Kim KW, Lee S. Genetic analysis of multiple endocrine neoplasia Type 1(MEN1) leads to misdiagnosis of an extremely rare presentation of intrasellar cavernous hemangioma as MEN1. End. Met., 2014, 29(2): 146–153. |
| [3] | Ma LC, Li WY, Chen WQ, Wu YK. Intrasellar cavernous hemangioma. Neur. Ind., 2014, 62(1): 95–96. DOI:10.4103/0028-3886.128352 |
| [4] | Chuang CC, Jung SM, Yang JT, Chang CN, Pai PC. Intrasellar cavernous hemangioma. J. Clini. Neur., 2006, 13(6): 672–675. DOI:10.1016/j.jocn.2005.08.017 |
| [5] | Hori S, Hayashi N, Nomoto K, Sato H, Hayashi T, Nagai S, Nishikata M, Endo S. Cavernous sinus cavernous hemangioma largely extending into the sella turcica and mimicking pituitary adenoma. Neurol Med Chir (Tokyo), 2010, 50(4): 330–332. DOI:10.2176/nmc.50.330 |
| [6] | Fraser JF, Mass AY, Brown S, Anand VK, Schwartz TH. Transnasal endoscopic resection of a cavernous sinus hemangioma:Technical note and review of the literature. Skull Base, 2008, 18(5): 309–315. DOI:10.1055/s-0028-1086059 |
| [7] | Wang Y, Li P, Zhang XJ, Xu YY, Wang W. Gamma knife surgery for cavernous sinus hemanginoma:A report of 32 cases. World Neurosurg, 2016, 94: 18–25. DOI:10.1016/j.wneu.2016.06.094 |



