2. Department of Neurosurgery, Beijing Tsinghua Changgung Hospital, Medical Center, Tsinghua University, Beijing 102218, China
Neurocutaneous melanosis (NCM), first described by Rokitansky in 1861, is a congenital, nonheritable phakomatosis, which was generally thought to result from neuroectodermal dysplasia in which the neural crest cells erroneously migrate to the skin and pia mater[1-3]. In 1991, Kadonaga and Frieden reviewed the features of NCM and proposed the currently accepted modified criteria[4] (Table 1). When neur-ological signs are present in children, death occurs within 3 years after a rapid deteriorating course[5]. To date, there are only 15 reported cases of NCM confirmed by histopathology in adult patients[6-20]. In this report, we present a case of a woman diagnosed with NCM with intraspinal malignant melanoma. The detailed clinical description and systematic analyses in conjunction with the related literature review are provided as well.
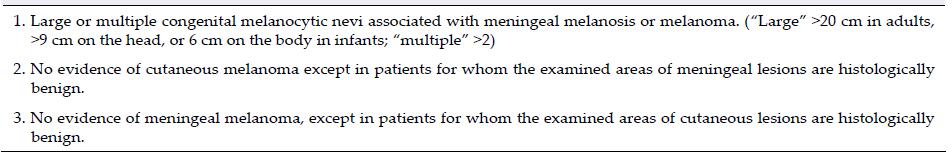
|
A 41-year-old woman presented in our hospital with a 5-month history of progressive low back and left lower extremity pain. On presentation, her visual analog scale (VAS) score was 8 points. The patient's physical and neurological examination results were normal. Laboratory findings were within normal levels. Her medical history consisted of a giant congenital blue nevus occupying the back at birth (Figure 1a).

|
| Figure 1 (a) A giant congenital blue nevus in the patient's back. (b) The spinal cord and cauda equina surrounded by dark black soft tissues. |
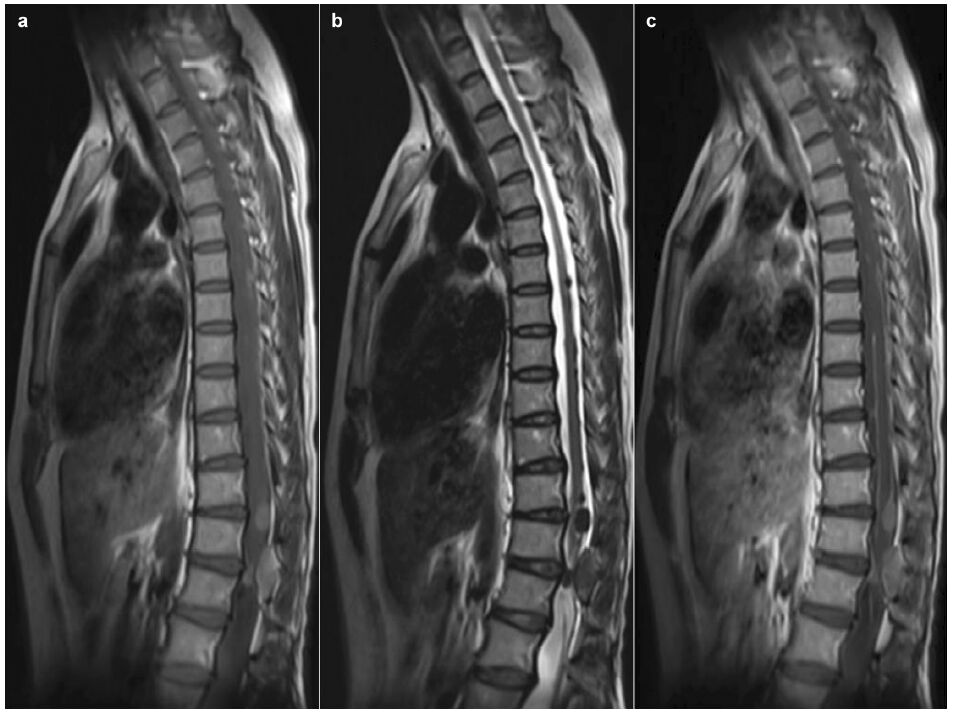
Magnetic resonance imaging (MRI) revealed com-pression and distortion of the spinal cord caused by intraspinal multi-nodules at the level of T6 through L1, which were hyperintense on the T1-weighted MR image (T1WI) and hypointense on the T2-weighted image (T2WI). The MR images obtained after gadolinium-diethylenetriamine pentaacetic acid (Gd- DTPA) injection clearly showed homogenous enhan-cement of the lesions on T1-weighted images (Figure 2). The cervical spine and intracranial lesions were not observed on the series of MR images. Based on the neuroimaging results, intraspinal neurofibroma was suspected. Skin biopsy on the back revealed congenital nevi of the common melanocytic type.
|
| Figure 2 Sagittal magnetic resonance (MR) images. Multi-nodules of T6 through L1, hyperintense on the T1 weighted image (a), hypointense on the T2 weighted image (b), and homogenous enhancement of the lesions and linear enhancement of the spinal pia materon T1-weighted images (c). |
A T11-L1 laminectomy with neurophysiological monitoring was performed via a posterior approach. The spinal cord and caudaequina were surrounded by dark black soft tissues with irregular and indistinct margins that could be sucked in (Figure 1b). Two dark black nodules were solid and tightly adherent to the dorsal surface of the spinal cord, and were almost totally resected.
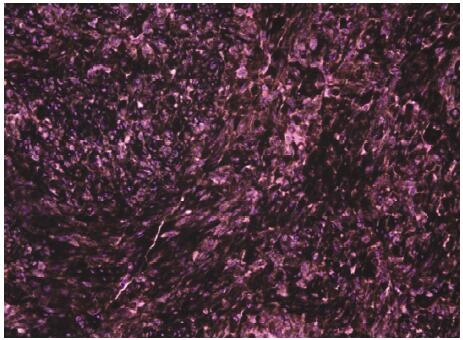
In the histopathological examination, there were malignant tumors containing variable amount of melanin with areas of necrosis and foci of paren-chymal infiltration. Nuclear pleomorphism with occasional mitotic figures was observed (Figure 3). Immunohistochemical determination showed that the nodules were positive for HMB-45, S-100, and Melan A, while negative for epithelial membrane antigen (EMA). Final diagnosis was confirmed as NCM with intraspinal malignant melanoma.
|
| Figure 3 Hematoxylin and Eosin (H&E) staining, ×400. Variable amounts of melanin with areas of necrosis and foci of parenchymal infiltration and nuclear pleomorphism with occasional mitotic figures are observed. |
Adjuvant chemotherapy was followed. The post- operative course was uneventful and her symptoms significantly improved (VAS: 3 points). However, she developed symptoms of intracranial hypertension and deteriorated rapidly after 11 months of operation, and died 1 month later. An autopsy was not permitted.
3 DiscussionNCM is a rare disorder characterized by lesions with poor prognosis. Neurologic manifestations of NCM appear generally in the first 2 years after birth, or later in the second decade of life. Within 3 years of the initial symptoms, death occurs in more than 50% of patients[1]. Fifteen reported cases of NCM confirmed by histopathology in adult patients plus the present case in our experience have been summarized to characterize this clinical entity[6-20]. Analyses showed that the average age was 33.8 years (range 19-65 years), and 11 patients (68.8%) were between 20 and 40 years. A slight male predominance (M:F/11:5) was found. However, there was no gender preference in children[2].
The major clinical manifestations were symptoms related to increased intracranial pressure or hydro-cephalus, such as headache, vomiting, and diplopia (56.2%), epilepsy (25%) and weakness (18.8%). In one case, the initial presentation was with excessive sweat-ing of the palms and soles, followed by numbness of the extremities[7]. Patients with bladder or bowel dysfunction, or developmental delay have not been pre-viously reported. Our case presented progressive low back and left lower extremity pain without increased intracranial pressure or epilepsy as the symptom. We thought that the symptom was caused by spinal cord compression and infiltration of malignant melanocytes. The onset of symptoms varied widely. The incubation period ranged from 1 week to 10 years, while the average period was 25 months, which was shorter than in patients with the symptom of seizures (average period: 61 months).
Once NCM is clinically suspected, MRI with gado-linium contrast is the best diagnostic choice. Generally, the most frequent MRI finding is linear or mass hyperintense signals on T1WI or hypointense signal on T2WI with homogenous enhancement. Six patients (37.5%) had hydrocephalus. In children, approximately two thirds developed hydrocephalus[21,22]. Three cases (18.8%) showed Dandy-Walker malformation, and 2 cases (12.5%) showed intracranial dermoid tumor. Locations of linear or mass lesions varied from the cerebral fissures and sulci to the cisterns. Our case is the only reported presentation of NCM with malignant melanomas located in the spinal cord in adults.
Unfortunately, although surgery was principally performed, radical removal was largely impossible due to massive infiltration and rapid relapses of masses. The main purpose of the operation was to relieve the neurological symptoms and ensure histological diagnosis. Neither chemotherapy nor radiation therapy has been shown to improve the outcome. Although this disease is rare in adults, the prognosis is considerably worse in adult patients. For the 12 cases for which detailed follow-up information was available, 9 patients (75%) died, with a survival time ranging from 1 day to 29 months post-operation. Death occurred within the first month of operation in 6 cases (46.2%). The median survival time was 3 months (statistical analyses conducted using SPSS 18.0 for Windows).
4 ConclusionsWe presented a case of a rare reported presentation of NCM with intraspinal malignant melanoma in an adult patient. Although rare, this clinical entity causes significant mortality and has poor prognosis.
Conflict of interests
All contributing authors have no conflict of interests.
| [1] | Di Rocco F, Sabatino G, Koutzoglou M, Battaglia D, Caldarelli M, Tamburrini G. Neurocutaneous melanosis. Childs Nerv Syst , 2004, 20 (1) : 23–28. DOI:10.1007/s00381-003-0835-9 |
| [2] | Pavlidou E, Hagel C, Papavasilliou A, Giouroukos S, Panteliadis C. Neurocutaneous melanosis: Report of three cases and up-to-date review. J Child Neurol , 2008, 23 (12) : 1382–1391. |
| [3] | Rokitansky J. Ein ausgezeichneter Fall von Pigment-Mal mit ausgebreiteter Pigmentierung der inneren Hirn-und Rückenmarkshäute. Allg Wien Med Z , 1861, 6 : 113–116. |
| [4] | Kadonaga JN, Frieden IJ. Neurocutaneous melanosis: Definition and review of the literature. J Am Acad Dermatol , 1991, 24 (5 Pt 1) : 747–755. |
| [5] | Waelchli R, Aylett SE, Atherton D, Thompson DJ, Chong WK, Kinsler VA. Classification of neurological abnormalities in children with congenital melanocytic naevus syndrome identifies magnetic resonance imaging as the best predictor of clinical outcome. Br J Dermatol , 2015, 173 (3) : 739–750. DOI:10.1111/bjd.13898 |
| [6] | Arunkumar MJ, Ranjan A, Jacob M, Rajshekhar V. Neurocutaneous melanosis: A case of primary intracranial melanoma with metastasis. Clin Oncol , 2001, 13 (1) : 52–54. |
| [7] | Faillace WJ, Okawara SH, McDonald JV. Neurocutaneous melanosis with extensive intracerebral and spinal cord involvement. Report of two cases. J Neurosurg , 1984, 61 (4) : 782–785. DOI:10.3171/jns.1984.61.4.0782 |
| [8] | Ge P F, Wang H F, Zhong Y P, Chen B, Ling F, Luo Y. Rare presentation in an adult patient with neurocutaneous melanosis. Int J Dermatol , 2010, 49 (11) : 1311–1313. DOI:10.1111/ijd.2010.49.issue-11 |
| [9] | Kang SG, Yoo DS, Cho KS, Kim DS, Chang ED, Huh PW, Kim MC. Coexisting intracranial meningeal melanocytoma, dermoid tumor, and Dandy-Walker cyst in a patient with neurocutaneous melanosis. Case report. J Neurosurg , 2006, 104 (3) : 444–447. |
| [10] | Kiecker F, Hofmann MA, Audring H, Brenner A, Labitzke C, Sterry W, Trefzer U. Large primary meningeal melanoma in an adult patient with neurocutaneous melanosis. Clin Neurol Neurosurg , 2007, 109 (5) : 448–451. DOI:10.1016/j.clineuro.2007.02.004 |
| [11] | Kimura H, Itoyama Y, Fujioka S, Ushio Y. Neurocutaneous melanosis with intracranial malignant melanoma in an adult: A case report. No Shinkei Geka , 1997, 25 (9) : 819–822. |
| [12] | Kim YJ, Won YD, Kim KT, Chang ED, Huh PW. Parenchymal neurocutaneous melanosis in association with intraventricular dermoid and Dandy-Walker variant: A case report. Korean J Radiol , 2006, 7 (2) : 145–148. DOI:10.3348/kjr.2006.7.2.145 |
| [13] | Oliveira RS, Carvalho AP, Noro F, Melo AS, Monteiro R, Guimarães R, Landeiro JA. Neurocutaneous melanosis. Arq Neuropsiquiatr , 2013, 71 (2) : 130–131. DOI:10.1590/S0004-282X2013000200016 |
| [14] | Peretti-Viton P, Gorincour G, Feuillet L, Lambot K, Brunel H, Raybaud C, Pellissier J, Chérif AA. Neurocutaneous melanosis: Radiological-pathological correlation. Eur Radiol , 2002, 12 (6) : 1349–1353. DOI:10.1007/s00330-001-1195-z |
| [15] | Ramaswamy V, Delaney H, Haque S, Marghoob A, Khakoo Y. Spectrum of central nervous system abnormalities in neurocutaneous melanocytosis. Dev Med Child Neurol , 2012, 54 (6) : 563–568. DOI:10.1111/dmcn.2012.54.issue-6 |
| [16] | Shinno K, Nagahiro S, Uno M, Kannuki S, Nakaiso M, Sano N, Horiguchi H. Neurocutaneous melanosis associated with malignant leptomeningeal melanoma in an adult: Clinical significance of 5-S-cysteinyldopa in the cerebrospinal fluid-case report. Neurol Med Chir (Tokyo) , 2003, 43 (12) : 619–625. DOI:10.2176/nmc.43.619 |
| [17] | Vadoud-Seyedi R, Heenen M. Neurocutaneous melanosis. Dermatology , 1994, 188 (1) : 62–65. DOI:10.1159/000247089 |
| [18] | Walbert T, Sloan AE, Cohen ML, Koubeissi MZ. Symptomatic neurocutaneous melanosis and Dandy-Walker malformation in an adult. J Clin Oncol , 2009, 27 (17) : 2886–2887. DOI:10.1200/JCO.2008.21.5830 |
| [19] | Ye BS, Cho YJ, Jang SH, Lee BI, Heo K, Jung HH, Chang JW, Kim SH. Neurocutaneous melanosis presenting as chronic partial epilepsy. J Clin Neurol , 2008, 4 (3) : 134–137. DOI:10.3988/jcn.2008.4.3.134 |
| [20] | Zhang W, Miao JT, Li Q, Liu R, Li ZY. Neurocutaneous melanosis in an adult patient with diffuse leptomeningeal melanosis and a rapidly deteriorating course: Case report and review of the literature. Clin Neurol Neurosurg , 2008, 110 (6) : 609–613. DOI:10.1016/j.clineuro.2008.02.022 |
| [21] | Kadonaga JN, Barkovich AJ, Edwards MSB, Frieden IJ. Neurocutaneous melanosis in association with the Dandy Walker complex. Pediatr Dermatol , 1992, 9 (1) : 37–43. DOI:10.1111/j.1525-1470.1992.tb00323.x |
| [22] | Mena-Cedillos CA, Valencia-Herrera AM, Arroyo-Pineda AI, Salgado-Jiménez MA, Espinoza-Montero R, Martínez-Avalos AB, Perales-Arroyo A. Neurocutaneous melanosis in association with the Dandy-Walker complex, complicated by melanoma: Report of a case and literature review. Pediatr Dermatol , 2002, 19 (3) : 237–242. DOI:10.1046/j.1525-1470.2002.00073.x |



