| 门静脉瘤的MSCT诊断价值 |
门静脉瘤较罕见,约占全身静脉瘤的3%[1],自1956年报道第1例以来尚不足200例[2],文献[3]报道较少,且未有明确的诊断及治疗方法[4]。炫速双源CT是一种安全、无创、有效的影像检查技术,广泛应用于肝胆系统及其血管疾病的诊断。现回顾性分析我院2016年1月至2017年12月收集的14例门静脉瘤患者的临床及影像资料,旨在探讨炫速双源CT对门静脉瘤的诊断价值,提高对门静脉瘤的认识。
1 资料与方法 1.1 一般资料14例中男8例,女6例;年龄35~74岁,平均57.7岁。临床表现:肝硬化合并肝癌3例,肝硬化2例,肝硬化合并胆道系统结石1例,胆道系统结石合并门静脉海绵样变性3例,胆道系统结石1例,乳腺癌、宫颈癌各1例,无明显不适1例,体检患者1例,其中合并门静脉高压9例。诊断标准[5-7]:门静脉管径大于邻近段正常的门静脉,呈囊状或梭形瘤样扩张。根据发生部位分为肝内型、肝外型。
1.2 仪器与方法14例均行炫速双源CT检查,扫描范围:膈顶至肾下极或耻骨联合下缘。扫描参数:120 kV,300 mA,层厚、层距均为5 mm,螺距0.6。采用高压注射器经肘静脉注入非离子型对比剂碘海醇(350 mgl/mL)70~80 mL,流率3.0~4.5 mL/s,后以相同流率注射生理盐水40 mL,分别于25~30、70~75 s行动脉期、门静脉期扫描。对门静脉期图像行薄层重建,重建层厚0.75 mm,间隔0.75 mm,传至syngo.via工作站,行MPR、MIP、VR。观察并记录肝胆系统情况,以及门静脉瘤的发生部位、形态、大小、CT表现、有无合并症等。
2 结果14例均为单发,其中肝外型10例(图 1,2),肝内型4例;脾静脉与肠系膜上静脉交汇处9例(图 2),门静脉主干1例(图 1),门静脉左支2例,门静脉左右支分叉处2例;11例呈囊状扩张(图 1,2),3例呈梭形扩张。CT平扫表现为与大动脉相近的稍低密度影,增强扫描均表现为与门静脉强化相一致的囊状或梭形瘤样扩张,瘤径均大于邻近段正常门静脉;其中2例合并钙化,2例合并门静脉海绵样变性,1例合并门静脉右支栓子形成(图 1),1例合并腹主动脉瘤。
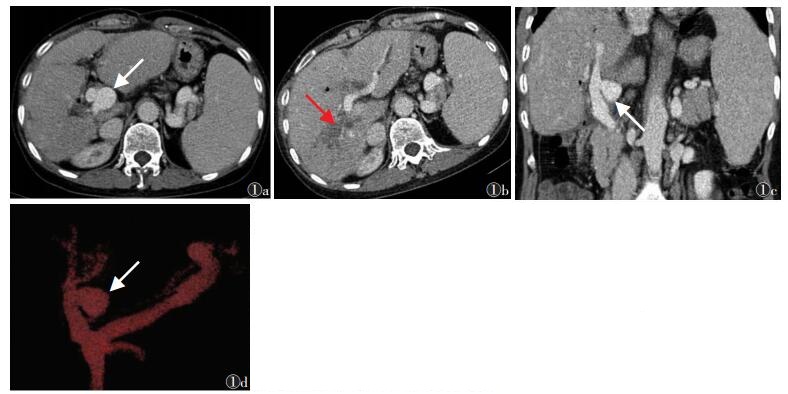 |
| 图 1 女,57岁,肝内胆管结石术后 图 1a,1b为不同层面CT横轴位图像,图 1c,1d为MPR冠状位及VR图像。门静脉主干左侧囊状瘤样扩张(箭头),大于邻近段正常门静脉,与门静脉同步强化;门静脉右支栓子形成(红箭);肝硬化,脾大,胆道系统轻度扩张、少量积气 |
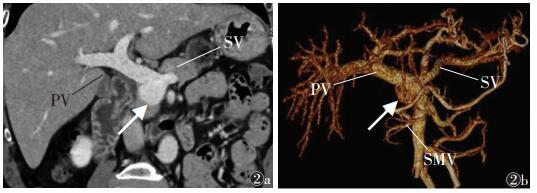 |
| 图 2 男,50岁,体检患者 图 2a,2b分别为CT冠状位及VR图像,示肠系膜上静脉与脾静脉交汇处门静脉囊状扩张(箭头),大于邻近段正常门静脉,与门静脉同步强化(PV:门静脉主干;SV,脾静脉;SMV:肠系膜上静脉) |
3 讨论
门静脉瘤,又称门静脉瘤样扩张,表现为门静脉主干或分支局部囊状或梭形扩张,大于邻近段门静脉。组织病理学表现为门静脉壁的内中膜变薄、破坏[8-10]。门静脉瘤患者大多无临床症状,但当瘤体较大压迫邻近组织结构或引起并发症(血栓、门静脉高压、破裂等)时,可出现腹背部疼痛、胃肠道出血、发热、黄疸、体质量减轻等症状[10-12]。本组大多因肝硬化、胆道系统结石就诊,偶然发现门静脉瘤,无与门静脉瘤相关的临床症状,与文献报道相符,分析其原因可能是门静脉瘤较小,未压迫邻近组织器官,或肝硬化、胆道系统结石症状掩盖了门静脉瘤引起的症状。
门静脉瘤可分为先天性、获得性。先天性门静脉瘤较少见,其形成原因可能是门静脉局部血管壁先天性肌发育不良或胚胎期原始右脐肠静脉未闭或憩室残留并增大,可在子宫内经超声诊断[5];肝脏组织正常且未合并门静脉高压的门静脉瘤,随访过程中,如未发生改变,也强烈提示为先天性[6]。获得性门静脉瘤更常见,引发因素有肝硬化、门静脉高压、胰腺炎、创伤、恶性门静脉栓子、肝移植等[5, 11, 13],其中最危险因素为肝硬化、门静脉高压。本组中,肝硬化合并门静脉高压或单纯门静脉高压患者,可能是长期门静脉高压引起血流动力学改变,导致管壁内膜变薄、中膜代偿性增生肥大,继而纤维组织增生,最终管壁变薄,门静脉瘤样扩张[9];胆道系统结石,可能是长期门静脉周围的炎性刺激,导致门静脉管壁损伤、变薄,最终引起门静脉瘤样扩张,故获得性门静脉瘤与胆道系统结石关系密切。而乳腺癌、宫颈癌、体检患者,无上述危险因素存在及血流动力学改变,故笔者推测其为先天性。
Doust等[14]通过超声研究正常人与肝硬化患者的门静脉直径,发现正常人门静脉直径≤15 mm,肝硬化患者≤19 mm。因此,有学者[6]认为肝内、肝外门静脉局部扩张大于15、20 mm可诊断为门静脉瘤,但也有学者[5-7]认为门静脉管径明显大于邻近段正常的门静脉,呈囊状或梭形瘤样扩张,即可诊断门静脉瘤;笔者将后者作为本组的诊断标准。门静脉瘤可为多种形状,最常见为梭形,其次为囊状[4, 15],本组11例呈囊状,3例呈梭形,与文献报道不符,可能是例数较少。门静脉瘤依据发生部位分为肝内型、肝外型,肝外型多见,且主要发生于脾静脉与肠系膜上静脉交汇处,本组发生在脾静脉与肠系膜上静脉汇合处9例,与文献报道相符。门静脉瘤MSCT平扫表现为与大动脉相近的稍低密度影,增强扫描与门静脉同步强化,部分患者可见血栓、瘤壁钙化、门静脉海绵样变性及动脉瘤等并发症。
一般情况下,临床手术指征依据门静脉瘤大小及其引起的并发症与临床症状,最常见的是血栓、压迫邻近结构引起相应症状、瘤体即将破裂征象(持续性腹部疼痛)[4, 16]。但绝大多数患者完全无症状,行超声定期随访即可[17]。如随访中患者出现症状或瘤体增大、有破裂和血栓形成的风险,则需及时手术治疗。文献对需手术治疗的门静脉瘤体大小并无绝对标准,据Cho等[10]报道,门静脉瘤直径大于4.0 cm时需手术治疗。手术治疗方案会根据患者的危险因素(瘤体形态、位置改变),行门静脉瘤缝合、门静脉瘤切除术[17-19]。一般情况下,此类患者不能直接切除瘤体,而是采用脾脏切除术或门体分流术,以减少门静脉的血流量[18]。合并血栓形成患者,需及时治疗,以免病情加重,同时多数患者有肝硬化、门静脉高压、胆道系统结石,虽瘤体较小,但仍需密切随访观察,以免出现并发症。
总之,CT不仅能够直观、清晰、准确显示门静脉瘤及有无并发症,还能清晰显示肝脏、胆道系统是否存在相关危险因素,为临床进一步治疗提供有效信息。
| [1] |
Turner KC, Bohannon WT, Atkins MD. Portal vein aneurysm:a rare occurrence[J]. J Vasc Nurs, 2011, 29: 135-138. DOI:10.1016/j.jvn.2011.08.001 |
| [2] |
Ma R, Balakrishnan A, See TC, et al. Extra-hepatic portal vein aneurysm:A case report, overview of the literature and suggested management algorithm[J]. Int J Surg Case Rep, 2012, 3: 555-558. DOI:10.1016/j.ijscr.2012.07.009 |
| [3] |
Lall P, Potineni L, Dosluoglu HH. Complete spontaneous regression of an extrahepatic portal vein aneurysm[J]. J Vasc Surg, 2011, 53: 206-208. DOI:10.1016/j.jvs.2010.07.063 |
| [4] |
Flis V, Gadzijev E. Reconstruction of the main portal vein for a large saccular aneurysm[J]. HPB, 2003, 5: 188-190. DOI:10.1080/13651820310001351 |
| [5] |
纪昌学, 涂蓉, 俞安乐, 等. 64层螺旋CT血管成像对门静脉瘤的诊断价值初探[J]. 中国临床医学影像杂志, 2010, 21(9): 662-663. DOI:10.3969/j.issn.1008-1062.2010.09.019 |
| [6] |
Gallego C, Velasco M, Marcuello P, et al. Congenital and acquired anomalies of the portal venous system[J]. Radiographics, 2002, 22: 141-159. DOI:10.1148/radiographics.22.1.g02ja08141 |
| [7] |
吴晓, 金中高, 祝跃明. 肝外型门静脉瘤的CT诊断[J]. 肝胆胰外科杂志, 2009, 21(6): 487-488. DOI:10.3969/j.issn.1007-1954.2009.06.023 |
| [8] |
秦军. 门静脉瘤的CT和MRI诊断[J]. 中国CT和MRI杂志, 2014, 59(6): 61-63. DOI:10.3969/j.issn.1672-5131.2014.06.18 |
| [9] |
杨琳媛, 马峰, 丁军. 门静脉瘤的临床及影像学表现附病例报道[J]. 中国实验诊断学, 2013, 17(11): 2093-2094. |
| [10] |
Cho SW, Marsh JW, Fontes PA, et al. Extrahepatic portal vein aneurysm-report of six patients and review of the literature[J]. J Gastrointest Surg, 2008, 12: 145-152. DOI:10.1007/s11605-007-0313-x |
| [11] |
Labgaa I, Lachenal Y, Allemann P, et al. Giant extra-hepatic thrombosed portal vein aneurysm:a case report and review of the literature[J]. World Journal of Emergency Surgery, 2014, 9: 35. DOI:10.1186/1749-7922-9-35 |
| [12] |
Giannoukas AD, Sfyroeas GS. Current management of visceral venous aneurysms[J]. Phlebolymphology, 2010, 17: 130-136. |
| [13] |
Molinares B, Alvarez S, García V, et al. Extrahepatic portal vein aneurysm after liver transplantation in a child:case report[J]. Pediatric Transplantation, 2013, 17: 33-36. DOI:10.1111/j.1399-3046.2012.01782.x |
| [14] |
Doust BD, Pearce JD. Gray-scale ultrasonic properties of the normal and inflamed pancreas[J]. Radiology, 1976, 120: 653-657. DOI:10.1148/120.3.653 |
| [15] |
Blasbalg R, Yamada RM, Tiferes DA. Extrahepatic portal vein aneurysms[J]. AJR Am J Roentgenol, 2000, 174: 877. |
| [16] |
Giannoukas AD, Sfyroeas GS. Current management of visceral venous aneurysms[J]. Phlebolymphology, 2010, 17: 130-136. |
| [17] |
Gallagher DM, Leiman S, Hux CH. In utero diagnosis of a portal vein aneurysm[J]. J Clin Ultrasound, 1993, 21: 147-151. DOI:10.1002/(ISSN)1097-0096 |
| [18] |
Fujikawa T, Tanaka A, Yoshimoto Y. Enlarged extrahepatic portal vein aneurysm in a noncirrhotic patient:a therapeutic dilemma[J]. Bmj Case Reports, 2011, 2011: ⅱ. |
| [19] |
Jin B, Sun Y, Li YQ, et al. Extrahepatic portal vein aneurysm:two case reports of surgical intervention[J]. World J Gastroen-terol, 2005, 14: 2206-2209. |
 2018, Vol. 16
2018, Vol. 16


