| 调神法针刺调节失眠患者丘脑功能连接的fMRI研究 |
2. 北京中医药大学, 北京 100029
2. Beijing University of Traditional Chinese Medicine, Beijing 100029, China
失眠是指睡眠机会和睡眠环境适当的条件下,仍对睡眠时间和/或质量不满足,并产生疲劳、情绪障碍、记忆减退等日间功能受损的一种主观体验[1]。其中,疲劳被视为失眠最常见和持久的日间症状[2],且其严重程度与失眠程度密切相关,严重影响患者的社会功能[3]。fMRI可直观显示针刺对大脑功能活动的影响,为揭示针刺治疗的潜在中枢机制提供可能。调神法针刺可有效改善失眠患者的睡眠质量并缓解日间疲劳[4]。丘脑与睡眠-觉醒、疲劳调节密切相关[2],但丘脑在针刺治疗失眠中的作用机制尚待深入探讨。本研究以丘脑为ROI,采用静息态功能连接方法,从fMRI角度探讨失眠患者与健康受试者丘脑FC差异,以及失眠患者调神法针刺前后FC的变化,以期为揭示针刺治疗失眠的中枢机制提供影像学依据。
1 资料与方法 1.1 一般资料招募2018年12月至2020年12月首都医科大学附属北京中医医院收治的失眠患者60例(失眠组),按1∶1比例随机分为调神法针刺组和非穴浅刺组各30例。纳入标准:符合《精神障碍诊断与统计手册(第5版)》[5]中失眠的诊断标准;年龄18~60岁;匹兹堡睡眠质量指数(Pittsburgh sleep qualify index,PSQI)评分>8分;过度觉醒量表(hyper arousal scale,HAS)评分>32分;汉密尔顿抑郁量表(Hamilton depression scale,HAMD)评分 < 7分;汉密尔顿焦虑量表(Hamilton anxiety scale,HAMA)评分 < 14分;近1个月未服用助眠药物;可配合完成MRI扫描;右利手。排除标准:合并抑郁症、焦虑症、精神分裂症等严重精神疾病;患有心、肝、肾、血液、消化系统等严重原发性疾病;孕期及哺乳期妇女;MRI扫描中发现明确病变或头部解剖结构严重不对称者。
同期招募30例健康受试者(健康组)。纳入标准:无对睡眠数量及质量不满的主诉;年龄18~60岁;PSQI评分 < 8分;HAS评分 < 32分;HAMD评分 < 7分;HAMA评分 < 14分;无心、肝、肾、血液、消化系统等疾病及精神疾病;可配合完成MRI扫描;右利手。
收集3组性别、年龄、学历等人口学资料及PSQI、HAS、HAMA、HAMD、疲劳量表-14(fatigue scale-14,FS-14)评分。
本研究经医院医学伦理委员会审批(审批号:2018BL-002-02),并于中国临床试验注册中心注册(注册号:Chi CTR1800015282),所有受试者均签署知情同意书。
1.2 针刺方法① 调神法针刺组:予调神法针刺。取穴:百会、神庭、四神聪,双侧本神、神门、内关、三阴交。百会、神庭、四神聪、本神平刺10~20 mm,余穴直刺10~30 mm,配合捻转提插平补平泻手法,以局部酸胀感为度,留针30 min。②非穴浅刺组:予非效穴浅刺。选取文献检索证实的7个对治疗失眠无效的穴位旁开的非穴点(均取双侧):臂臑、手三里、曲池、外关、风市、伏兔、梁丘旁开1寸。所有非穴点直刺1~2 mm,不行任何手法,留针30 min。
2组均隔日针刺1次,3次/周,连续4周。所有患者的针刺操作均由1位具有15年以上临床经验的针灸医师完成。
1.3 MRI检查采用Siemens 3.0 T Magnetom Trio MRI扫描仪。受试者仰卧,海绵塞固定头部,保持睁眼状态,避免入睡。采用磁化预备梯度回波序列对脑结构像T1WI-3D进行扫描,扫描参数:TR 2 300 ms,TE 2.32 ms,视野240 mm×240 mm,翻转角8°,层厚0.9 mm,矩阵256×256,切片数量192层,体素大小0.9 mm×0.9 mm×0.9 mm;使用轴位EPI序列获得fMRI图像,扫描参数:TR 3 000 ms,TE 30 ms,视野220 mm×220 mm,翻转角90°,层厚3.0 mm,体素大小3.5 mm×3.5 mm×3.5 mm,切片数量32层,带宽1 774 Hz。共采集240个全脑图像。
1.4 数据处理基于Matlab 2018b(The MathWorks,Inc.)平台的DPABI( http://rfmri.org/dpabi )软件包分析数据。
预处理步骤:①将DICOM图像格式转换为NIFTI格式;②剔除前10个时间点;③头动校正和时间层校正;④空间标准化和高斯平滑,将fMRI图像通过EPI模板配准至蒙特利尔神经病学研究所空间,采用6 mm的半峰全宽高斯平滑核行空间平滑;⑤去线性漂移和滤波;⑥回归协变量,去除头动、脑白质、脑脊液等信号的协变量。
以双侧丘脑为种子点,根据自动解剖标记3(automated anatomical labelling 3,ALL3)图谱[6]定义左侧丘脑[-12, -18, 8],右侧丘脑[12, -18, 8],取半径为5 mm的球体区域为VOI,将VOI的时间序列与全脑所有体素的时间序列行相关性分析,并将相关系数行Fisher z变换。
1.5 统计学处理使用SPSS 26.0软件进行数据分析。计数资料组间比较行χ2检验;计量资料符合正态分布以x±s表示,不符合正态分布以M(QL,QU)表示。组内比较符合正态分布行配对样本t检验,非正态分布行Wilcoxon秩和检验;组间比较符合正态分布行两独立样本t检验,非正态分布行Mann-Whitney U检验。采用Pearson相关性分析观察调神法针刺前后FC差值与PSQI、HAS、FS-14评分差值的相关性,多重比较采用Bonferroni校正。以P < 0.05为差异有统计学意义。
2 结果 2.1 各组临床资料比较调神法针刺组因个人原因脱落4例,因影像学质量控制剔除1例,非穴浅刺组因治疗效果不佳脱落6例,最终完成临床干预及fMRI扫描49例。
失眠组和健康组性别、年龄、学历差异均无统计学意义(均P>0.05);2组针刺前PSQI、HAS、HAMA、HAMD、FS-14评分差异均有统计学意义(均P < 0.001)(表 1)。调神法针刺组和非穴浅刺组性别、年龄、学历,以及针刺前HAMA、HAMD、PSQI、HAS、FS-14评分差异均无统计学意义(均P>0.05)(表 2,3)。
| 表 1 失眠组和健康组临床资料比较 |
 |
| 表 2 调神法针刺组和非穴浅刺组临床资料比较 |
 |
| 表 3 调神法针刺组和非穴浅刺组针刺前后临床量表评分比较 |
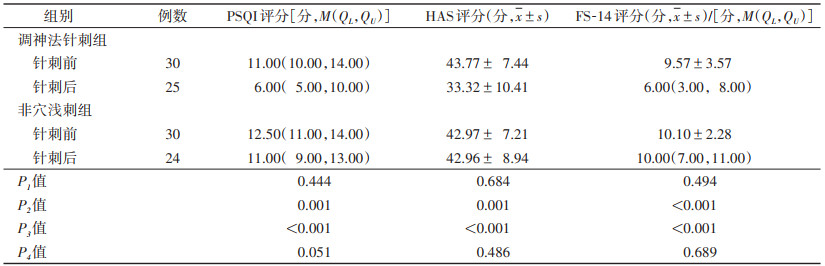 |
针刺后2组间PSQI、HAS、FS-14评分差异均有统计学意义(均P < 0.05);调神法针刺组针刺前后差异均有统计学意义(P < 0.001);非穴浅刺组针刺前后差异均无统计学意义(均P>0.05)(表 3)。
2.2 各组FC比较与健康组相比,失眠组针刺前左丘脑与右楔叶、右中央后回、右颞中回的FC均增强(均P < 0.05,FEW校正);右丘脑与右颞上回、右额中回、右扣带回、左枕中回、左额下回、左顶下回、左海马旁回的FC均增强(均P < 0.05,FEW校正)(图 1)。
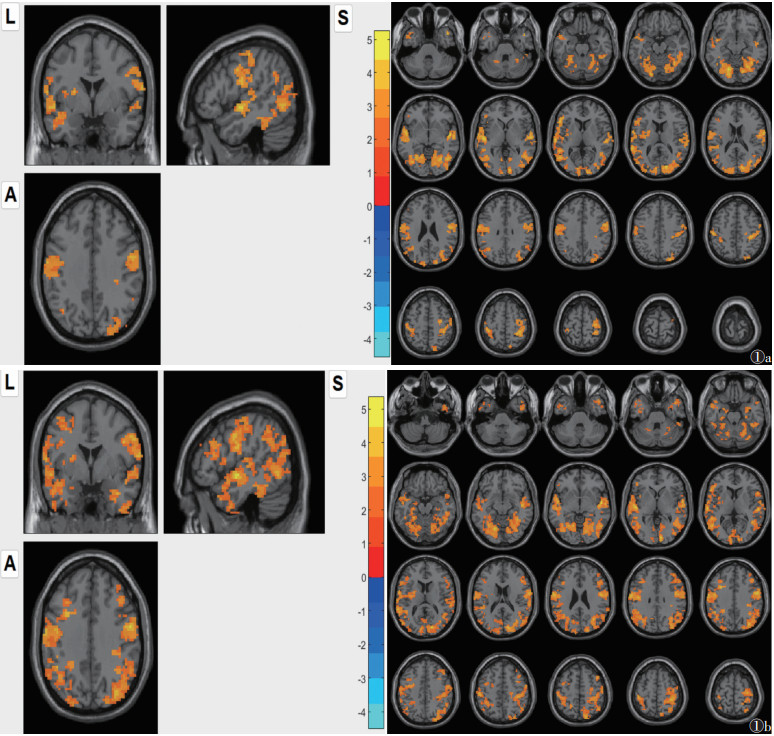 |
| 注:图 1a示左侧丘脑为种子点,图 1b示右侧丘脑为种子点。橙色区域代表失眠组较健康组FC增强的脑区(P < 0.05,FEW校正)。左侧图像为显示脑区FC改变的轴位和矢状位图;右侧图像为全面显示脑区FC改变的轴位图。L为左侧,S为矢状位,A为轴位 图 1 失眠组针刺前后与健康组丘脑功能连接(FC)比较 |
组内比较,调神法针刺组针刺前后左丘脑与左顶上回,右丘脑与左顶下回、左旁中央小叶、左额中回、右顶上回、右中央后回、双侧中扣带回的FC均减弱(均P < 0.05,FEW校正)(图 2)。针刺后调神法针刺组与非穴浅刺组比较,右丘脑与左额中回、左海马、右后扣带回的FC均减弱(均P < 0.05,FEW校正)(图 3)。
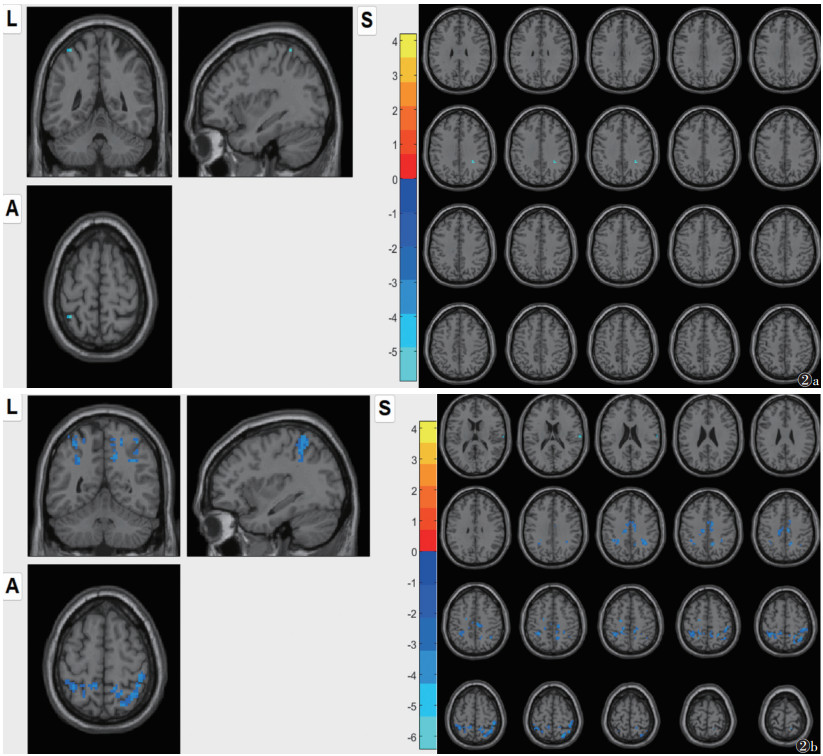 |
| 注:图 2a示左侧丘脑为种子点,图 2b示右侧丘脑为种子点。蓝色区域代表调神法针刺治疗后较治疗前FC降低的脑区(P < 0.05,FEW校正)。左侧图像为显示脑区FC改变的轴位和矢状位图;右侧图像为全面显示脑区FC改变的轴位图。L为左侧,S为矢状位,A为轴位 图 2 调神法针刺组针刺前后丘脑功能连接(FC)比较 |
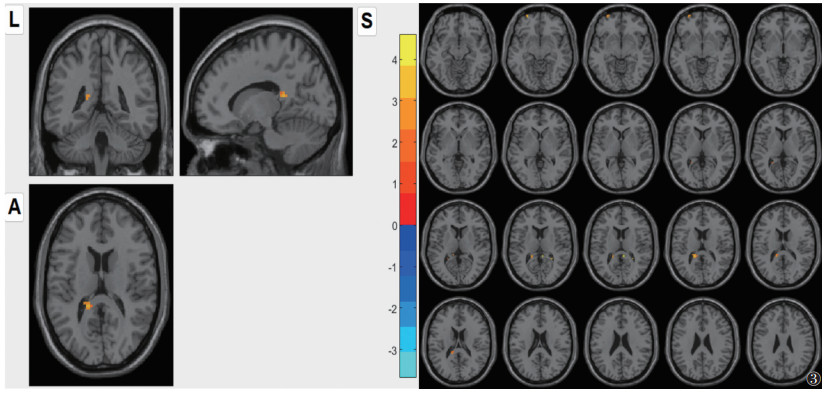 |
| 注:橙色区域代表针刺后非穴浅刺组较调神法针刺组功能连接(FC)升高的脑区(P < 0.05,FWE校正)。左侧图像为显示脑区FC改变的轴位和矢状位图;右侧图像为全面显示脑区FC改变的轴位图。L为左侧,S为矢状位,A为轴位 图 3 调神法针刺组与非穴浅刺组针刺后比较 |
2.3 调神法针刺组针刺前后FC差值与临床量表评分差值相关性分析
调神法针刺组右丘脑和左顶下回、右中扣带回、右顶上回减弱的FC值与FS-14评分均呈正相关(均P < 0.05);右丘脑和左旁中央小叶减弱的FC值与HAS评分呈正相关(P < 0.05)(图 4)。
 |
| 注:差值均为针刺后-针刺前,FS-14为疲劳量表-14,HAS为过度觉醒量表。Bonferroni校正后,P < 0.05为差异有统计学意义 图 4 调神法针刺组针刺前后功能连接(FC)差值与临床量表评分差值相关性散点图 |
3 讨论
丘脑调控大脑皮质兴奋状态,维持警觉性,调控睡眠-觉醒周期[7-9]。研究显示,失眠患者存在丘脑及其神经回路的FC、结构和代谢改变[2, 10-13],并与疲劳、觉醒密切相关[13]。丘脑的功能障碍也被视为失眠的神经机制之一[14]。
失眠患者由于睡眠结构和节律紊乱,在颞叶和楔叶表现出较高的自发性神经活动[15-16]。有研究发现失眠患者存在额叶和顶叶异常激活[17-18],以及丘脑和额中回、顶上小叶[19-20],中央后回与扣带回[21]的FC异常。此外,失眠严重程度还与海马旁回的异常血流活动有关[16],丘脑和海马旁回的FC增强与情绪失调及过度觉醒密切相关[20, 22]。本研究发现,失眠患者左丘脑与右楔叶、右中央后回、右颞中回,右丘脑与右颞上回、右额中回、右扣带回、左枕中回、左额中回、左顶下回、左海马旁回的FC增强。
顶下回属于中央执行控制网络,有研究显示失眠患者顶下回和前额叶的FC增强[23]。旁中央小叶属于感觉运动网络[24],失眠患者旁中央小叶和左中央后回、右中央前回的FC增强,且与失眠严重程度呈正相关[25]。顶上回位于默认网络,失眠患者丘脑和顶上回的FC降低与睡眠效率改善相关[26]。扣带回属于突显网络,与觉醒水平有关[27]。针刺调神是治疗失眠的第一要旨[28]。调神法针刺注重“脑神”与“心神”并调[28],选取百会、神庭、四神聪、本神调节脑神,联合心经、心包经腧穴神门和内关调节心神,三阴交调节经脉气血,养血安神。诸穴合用,以调神安眠。本研究显示,调神法针刺治疗后,丘脑与多个脑区的FC减低,且降低的右丘脑与左顶下回、右顶上回、右中扣带回的FC与FS-14评分差值呈正相关,右丘脑和左旁中央小叶减弱的FC与HAS评分差值呈正相关;这些脑区涉及多个脑网络,提示针刺治疗失眠可能通过调节丘脑的FC,整合大脑功能网络状态,从而改善过度觉醒和疲劳感知。
本研究存在一定局限性:丘脑功能复杂,且分为不同亚区,其调节睡眠-觉醒涉及多种神经回路的相互作用,后续研究可划分丘脑亚区进一步探讨;样本量较小,后续将增加样本量以提高研究的精确性;未采用多导睡眠监测等客观评价指标,影响了睡眠质量评价的准确性。
综上所述,丘脑在失眠发病机制中起重要作用,失眠患者存在异常的丘脑FC,而调神法针刺能调节丘脑FC,改善大脑过度觉醒,缓解日间疲劳,有效治疗失眠。fMRI可揭示调神法针刺治疗失眠的中枢机制。
| [1] |
中华医学会神经病学分会, 中华医学会神经病学分会睡眠障碍学组. 中国成人失眠诊断与治疗指南(2017版)[J]. 中华神经科杂志, 2018, 51(5): 324-335. DOI:10.3760/cma.j.issn.1006-7876.2018.05.002 |
| [2] |
GUO Y, CHEN Y, SHAO Y, et al. Thalamic network under wakefulness after sleep onset and its coupling with daytime fatigue in insomnia disorder: an EEG-fMRI study[J]. J Affect Disord, 2023, 334: 92-99. DOI:10.1016/j.jad.2023.04.100 |
| [3] |
罗燕鸿, 庄芸月, 宋天贺, 等. 失眠障碍和社会功能的关系: 疲劳和抑郁情绪的链式中介作用[J]. 神经疾病与精神卫生, 2023, 23(8): 557-562. DOI:10.3969/j.issn.1009-6574.2023.08.005 |
| [4] |
霍一珊, 陈昭伊, 尹雪娇, 等. 调神法针刺治疗原发性失眠: 随机对照预试验[J]. 中国针灸, 2023, 43(9): 1008-1013. |
| [5] |
American Psychiatric Association. Diagnostic and statistical manual of mental disorders fifth edition[M]. Arlington VA: American Psychiatric Association, 2013.
|
| [6] |
ROLLS E T, HUANG C C, LIN C P, et al. Automated anatomical labelling atlas 3[J]. Neuroimage, 2020, 206: 116189. DOI:10.1016/j.neuroimage.2019.116189 |
| [7] |
FALAHPOUR M, CHANG C, WONG C W, et al. Template-based prediction of vigilance fluctuations in resting-state fMRI[J]. Neuroimage, 2018, 174: 317-327. DOI:10.1016/j.neuroimage.2018.03.012 |
| [8] |
ZOU G, LI Y, LIU J, et al. Altered thalamic connectivity in insomnia disorder during wakefulness and sleep[J]. Hum Brain Mapp, 2021, 42(1): 259-270. DOI:10.1002/hbm.25221 |
| [9] |
HALE J R, WHITE T P, MAYHEW S D, et al. Altered thalamocortical and intra-thalamic functional connectivity during light sleep compared with wake[J]. Neuroimage, 2016, 125: 657-667. DOI:10.1016/j.neuroimage.2015.10.041 |
| [10] |
LIU C, KONG X Z, LIU X, et al. Long-term total sleep deprivation reduces thalamic gray matter volume in healthy men[J]. Neuroreport, 2014, 25(5): 320-323. DOI:10.1097/WNR.0000000000000091 |
| [11] |
KOO D L, SHIN J H, LIM J S, et al. Changes in subcortical shape and cognitive function in patients with chronic insomnia[J]. Sleep Med, 2017, 35: 23-26. DOI:10.1016/j.sleep.2017.04.002 |
| [12] |
DELUCA J, GENOVA H M, CAPILI E J, et al. Functional neuroimaging of fatigue[J]. Phys Med Rehabil Clin N Am, 2009, 20(2): 325-337. DOI:10.1016/j.pmr.2008.12.007 |
| [13] |
ANGIONI D, VIRECOULON GIUDICI K, MONTOYA MARTINEZ M, et al. Neuroimaging markers of chronic fatigue in older people: a narrative review[J]. Aging Clin Exp Res, 2021, 33(6): 1487-1492. DOI:10.1007/s40520-020-01666-1 |
| [14] |
LI M, WANG R, ZHAO M, et al. Abnormalities of thalamus volume and resting state functional connectivity in primary insomnia patients[J]. Brain Imaging Behav, 2019, 13(5): 1193-1201. DOI:10.1007/s11682-018-9932-y |
| [15] |
LI C, MA X, DONG M, et al. Abnormal spontaneous regional brain activity in primary insomnia: a resting-state functional magnetic resonance imaging study[J]. Neuropsychiatr Dis Treat, 2016, 12: 1371-1378. |
| [16] |
XU M, WANG Q, LI B, et al. Cerebellum and hippocampus abnormalities in patients with insomnia comorbid depression: a study on cerebral blood perfusion and functional connectivity[J]. Front Neurosci, 2023, 17: 1202514. DOI:10.3389/fnins.2023.1202514 |
| [17] |
ZANG S, CHEN Y, CHEN H, et al. Effects of acupuncture on the brain in primary insomnia: a coordinate-based meta-analysis of fMRI studies[J]. Front Neurol, 2023, 14: 1180393. DOI:10.3389/fneur.2023.1180393 |
| [18] |
LI Y, WANG E, ZHANG H, et al. Functional connectivity changes between parietal and prefrontal cortices in primary insomnia patients: evidence from resting-state fMRI[J]. Eur J Med Res, 2014, 19(1): 32. DOI:10.1186/2047-783X-19-32 |
| [19] |
PERRIER J, BRUIJEL J, NAVEAU M, et al. Functional connectivity correlates of attentional networks in insomnia disorder: a pilot study[J]. J Sleep Res, 2023, 32(3): e13796. DOI:10.1111/jsr.13796 |
| [20] |
KIM N, WON E, CHO S E, et al. Thalamocortical functional connectivity in patients with insomnia using resting-state fMRI[J]. J Psychiatry Neurosci, 2021, 46(6): E639-E646. DOI:10.1503/jpn.210066 |
| [21] |
HU Z, LI W, YE Y, et al. Alterations of functional connectivity in young people with depression mediate the relationship between sleep quality and cognitive function[J]. J Affect Disord, 2023, 340: 160-166. DOI:10.1016/j.jad.2023.08.026 |
| [22] |
BLOOD A J, ZATORRE R J, BERMUDEZ P, et al. Emotional responses to pleasant and unpleasant music correlate with activity in paralimbic brain regions[J]. Nat Neurosci, 1999, 2(4): 382-387. DOI:10.1038/7299 |
| [23] |
谭志, 骆俊佳, 罗树存, 等. 低频振幅联合功能连接对原发性失眠的研究[J]. 中国CT和MRI杂志, 2022, 20(2): 1-4. DOI:10.3969/j.issn.1672-5131.2022.02.001 |
| [24] |
JUNG M E, COLLETTA M, COALSON R, et al. Differences in interregional brain connectivity in children with unilateral hearing loss[J]. Laryngoscope, 2017, 127(11): 2636-2645. DOI:10.1002/lary.26587 |
| [25] |
BAI Y, TAN J, LIU X, et al. Resting-state functional connectivity of the sensory/somatomotor network associated with sleep quality: evidence from 202 young male samples[J]. Brain Imaging Behav, 2022, 16(4): 1832-1841. DOI:10.1007/s11682-022-00654-5 |
| [26] |
LEE Y G, KIM S, KIM N, et al. Changes in subcortical resting-state functional connectivity in patients with psychophysiological insomnia after cognitive-behavioral therapy: changes in resting-state FC after CBT for insomnia patients[J]. Neuroimage Clin, 2017, 17: 115-123. |
| [27] |
MENON V. Large-scale brain networks and psychopathology: a unifying triple network model[J]. Trends Cogn Sci, 2011, 15(10): 483-506. DOI:10.1016/j.tics.2011.08.003 |
| [28] |
郭静, 王麟鹏. "心神"与"脑神"在针刺治疗失眠中的重要意义[J]. 中国针灸, 2007, 27(S1): 71-72. |
 2025, Vol. 23
2025, Vol. 23


