文章信息
- 罗耀兵, 叶丰宁, 肖龙敏, 刘勇
- LUO Yaobing, YE Fengning, XIAO Longmin, LIU Yong
- 床旁超声FAST联合血清CRP、PCT、IL-6检测对急性胸腹创伤患者结局的预测价值
- Value of FAST combined with serum CRP, PCT, and IL-6 detection in predicting the clinical outcome of patients with acute chest and abdominal trauma
- 中国医科大学学报, 2024, 53(2): 172-177
- Journal of China Medical University, 2024, 53(2): 172-177
-
文章历史
- 收稿日期:2023-02-28
- 网络出版时间:2024-01-10 15:57:25
2. 恩施土家族苗族自治州民族医院超声影像科, 湖北 恩施 445000;
3. 恩施土家族苗族自治州民族医院胸外科, 湖北 恩施 445000
2. Department of Ultrasound Ima-ging, Enshi Tujia and Miao Autonomous Prefecture Ethnic Hospital, Enshi 445000, China;
3. Department of Thoracic Surgery, Enshi Tujia and Miao Autonomous Prefecture Ethnic Hospital, Enshi 445000, China
急性胸腹创伤为临床常见急诊创伤类型之一,大多危及内脏,且伤情变化复杂,严重时可引发休克、窒息等[1-2]。既往临床上多采用由急诊医生主导的床旁超声创伤重点超声评估法(focused assessment with sonography for trauma,FAST)为患者提供快速检查,以便及时采取急救措施来挽救患者的生命[3-5]。近年来,研究[6]显示FAST测定的下腔静脉-塌陷指数(collapsible index of inferior vena cava,IVC-CI)可评估患者的血流动力学,并与早期伤情严重程度密切相关。已有研究[7]显示,创伤造成死亡的患者中,60%在创伤现场与急救过程中死亡,40%在住院期间死亡。既往关于急诊医生主导的床旁超声FAST对急性创伤患者的研究多集中于急救过程中,对患者住院期间临床结局的预测鲜有报道。严重创伤患者通常会出现持续性炎症免疫抑制及代谢综合征,极易并发脓毒症、脓毒性休克及多器官衰竭,增加患者死亡风险[8]。创伤所造成的住院期间死亡主要因感染或器官功能障碍引起,目前已有多项生物学标志物[C反应蛋白(C-reactive protein,CRP)、降钙素原(procalcitonin,PCT)及白细胞介素-6(interleukin-6,IL-6)等]广泛应用于严重创伤患者病情的评估及指导治疗。本研究探讨急诊医生主导的床旁超声FAST联合血清CRP、PCT、IL-6检测对急性胸腹创伤患者结局的预测价值,旨在为临床诊疗提供参考。
1 材料与方法 1.1 研究对象及分组选取2019年2月至2022年2月我院急诊科收治的96例急性胸腹部创伤患者作为研究对象。纳入标准:(1)符合胸腹部创伤诊断标准[9],且受伤至入院时间 < 24 h;(2)患者或其家属知情同意并签署知情承诺书。排除标准:(1)非胸腹创伤或不含胸腹创伤的多发伤;(2)严重创伤导致入院当天死亡;(3)治疗 < 48 h死亡或出院;(4)入院后未持续治疗,自动出院;(5)合并心、肝、肾等重要脏器功能障碍。本研究获得医院伦理委员会批准[批号:2019伦审第(WY20)号]。根据患者临床结局(治疗48 h后生存状态)分为死亡组(n = 14)和生存组(n = 82)。
1.2 治疗策略接诊后迅速给予心电监护、吸氧,建立静脉输液通道,接诊医生立即检查患者受损具体部位,若患者昏迷无法配合检查时进行全面检查,包括头、胸、腹部CT等;同时还需根据急性胸腹创伤患者病情进行血常规及生物化学等各项指标检测,具体创伤急救措施根据患者病情综合判断。
1.3 检测方法 1.3.1 急诊医生主导的床旁超声FAST检测入院后即刻由急诊医生主导床旁超声FAST检查,患者平卧于操作台,采用超声诊断仪行FAST检查,探查胸腹腔,包括脾肾间隙及左右肋间、肋下,于右侧肋下纵向探测肝后下腔静脉(inferior vena cava,IVC),距右心房入口2 cm处测量下腔静脉管直径,超声图像于吸气末与呼气末同步冻结,测量下腔静脉最大直径(maximum diameter of inferior vena cava,IVCe)、下腔静脉最小直径(minimum diameter of inferior vena cava,IVCi),IVC-CI=(IVCe-IVCi)/IVCe×100%。
1.3.2 血清CRP、PCT、IL-6检测入院即刻(0 h),24、48 h于空腹状态下抽取肘静脉血(5 mL),高速离心10 min,分离血清、血浆,-80 ℃贮存。采用酶联免疫吸附试剂盒[艾博抗(上海)贸易有限公司]测定CRP、PCT、IL-6水平,采用酶标仪测定450 nm波长下吸光度值,计算样品中CRP、PCT、IL-6的水平,操作严格遵循试剂盒及仪器说明书进行。
1.3.3 CRAMS评分[10]采用国际常用CRAMS评分,包括循环、呼吸、腹部创伤、运动及语言等项目,合计0~10分,得分越低,表示患者伤情越严重。
1.4 统计学分析利用SPSS 21.0软件处理数据,计量资料采用x±s表示,2组间比较采用t检验,多组间比较采用重复测量方差分析;计数资料以率(%)表示,组间比较采用χ2检验。采用logistic回归分析影响急性胸腹创伤患者结局的危险因素。绘制受试者操作特征(receiver operating characteristic,ROC)曲线评估IVC-CI及血清CRP、PCT、IL-6水平对患者结局的预测价值,以Delong检验绘制临床决策曲线(decision curve analysis,DCA)分析临床净获益。P < 0.05为差异有统计学意义。
2 结果 2.1 2组一般临床指标、CRAMS评分及IVC-CI比较结果显示,2组性别、年龄、体质量、创伤类型、吸烟史、饮酒史及既往胸腹部手术史比较差异均无统计学意义(均P > 0.05);而死亡组CRAMS评分、IVC-CI均高于生存组(均P < 0.05)。见表 1。
| Group | n | Male/female | Age(year) | Weight(kg) | Trauma type [n(%)] | ||
| Traffic accident | Fall from height | Blunt force injury | |||||
| Death group | 14 | 8/6 | 40.75±4.49 | 63.25±6.14 | 10(71.43) | 3(21.43) | 1(7.14) |
| Survival group | 82 | 44/38 | 39.29±5.18 | 62.64±6.19 | 59(71.95) | 15(18.29) | 8(9.76) |
| t/χ2 | 0.059 | 0.992 | 0.341 | 0.150 | |||
| P | 0.809 | 0.324 | 0.734 | 0.928 | |||
| Group | Smoking [n(%)] | Drinking [n(%)] | Previous history of chest and abdominal surgery [n(%)] | CRAMS score | IVC-CI | ||
| Death group | 4(28.57) | 5(35.71) | 4(28.57) | 3.80±1.12 | 0.42±0.05 | ||
| Survival group | 23(28.05) | 25(30.49) | 17(20.73) | 2.65±0.84 | 0.34±0.04 | ||
| t/χ2 | 0.079 | 0.006 | 0.094 | 4.499 | 6.662 | ||
| P | 0.778 | 0.938 | 0.760 | < 0.001 | < 0.001 | ||
2.2 2组血清CRP、PCT、IL-6水平比较
结果显示,入院0、24、48 h死亡组血清CRP、PCT、IL-6水平均高于生存组(均P < 0.001)。死亡组患者血清CRP、PCT、IL-6水平从入院0 h至48 h时逐渐增高,各时间点比较差异有统计学意义(均P < 0.001);生存组患者血清CRP、PCT、IL-6水平从入院0 h至24 h升至最高,入院48 h时下降,各时间点比较差异均有统计学意义(均P < 0.001),见表 2。
| Item | n | 0 h | 24 h | 48 h |
| CRP(mg/L) | ||||
| Death group | 14 | 78.54±12.491) | 124.94±35.691),2) | 152.79±34.111),2),3) |
| Survival group | 82 | 68.96±15.87 | 108.49±30.122) | 80.85±10.232) |
| PCT(μg/L) | ||||
| Death group | 14 | 1.64±0.211) | 2.88±0.561),2) | 3.91±0.691),2),3) |
| Survival group | 82 | 1.22±0.27 | 2.35±0.492) | 2.04±0.522),3) |
| IL-6(pg/mL) | ||||
| Death group | 14 | 79.14±11.731) | 127.54±19.821),2) | 162.74±27.821),2),3) |
| Survival group | 82 | 70.22±12.09 | 105.19±15.262) | 85.69±15.122),3) |
| 1)P < 0.001 vs. survival group;2)P < 0.001 vs. 0 h in the same group;3)P < 0.001 vs. 24 h in the same group. | ||||
2.3 影响急性胸腹创伤患者结局危险因素的logistic回归分析
以急性胸腹创伤患者临床结局为因变量(生存=0,死亡=1),以单因素分析有统计学意义(P < 0.05)指标(CRAMS评分、IVC-CI及血清CRP、PCT、IL-6)为自变量进行logistic回归分析。结果显示,CRAMS评分、IVC-CI及血清CRP、PCT、IL-6是影响急性胸腹创伤患者结局的危险因素(均P < 0.001)。见表 3。
| Variable | β | SE | Waldχ2 | OR | 95%CI | P |
| CRAMS score | 2.693 | 0.674 | 15.969 | 14.782 | 6.851-31.894 | < 0.001 |
| IVC-CI | 2.726 | 0.683 | 15.932 | 15.274 | 6.263-37.252 | < 0.001 |
| CRP | 2.517 | 0.695 | 13.115 | 12.390 | 5.393-28.464 | < 0.001 |
| PCT | 2.680 | 0.702 | 14.579 | 14.591 | 6.012-35.411 | < 0.001 |
| IL-6 | 2.592 | 0.698 | 13.789 | 13.355 | 5.899-30.237 | < 0.001 |
2.4 IVC-CI及血清CRP、PCT、IL-6对患者结局的预测价值
以死亡为阳性,生存为阴性,IVC-CI及入院48 h血清CRP、PCT、IL-6水平绘制ROC曲线,获得IVC-CI及入院48 h血清CRP、PCT、IL-6各指标单独及联合的ROC曲线曲线下面积(area under the curve,AUC)、95%CI、截断值、灵敏度及特异度,见表 4,图 1。
| Index | AUC | 95%CI | Cut-off value | Sensitivity(%) | Specificity(%) |
| IVC-CI | 0.803 | 0.709-0.877 | 0.38 | 82.86 | 54.88 |
| CRP | 0.815 | 0.723-0.887 | 160.28 mg/L | 71.43 | 80.24 |
| PCT | 0.830 | 0.739-0.899 | 3.72 μg/L | 78.57 | 82.93 |
| IL-6 | 0.703 | 0.601-0.792 | 147.87 pg/ml | 71.43 | 69.51 |
| Combination | 0.930 | 0.860-0.972 | - | 87.96 | 90.41 |
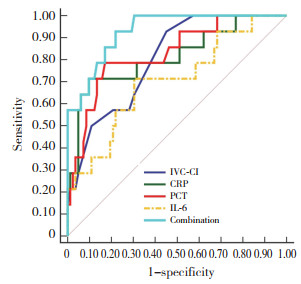
|
| 图 1 IVC-CI,血清CRP、PCT、IL-6单独及联合检测的ROC曲线 Fig.1 ROC curves for the IVC-CI and serum CRP, PCT, and IL-6 detection individually and in combination |
2.5 IVC-CI,血清CRP、PCT、IL-6单独及联合检测预测价值比较
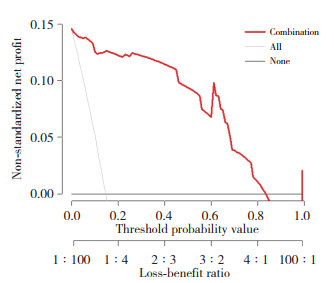
结果显示,IVC-CI联合入院48 h血清CRP、PCT、IL-6预测急性胸腹创伤患者结局的AUC值大于各单独指标,差异有统计学意义(均P < 0.05),见表 5。绘制IVC-CI联合入院48 h血清CRP、PCT、IL-6预测急性胸腹创伤患者结局DCA曲线的结果显示,IVC-CI联合入院48 h血清CRP、PCT、IL-6预测方案具有临床净获益,见图 2。
| Item | Difference in area | SE | Z | 95%CI | P |
| Combination vs. CRP | 0.115 | 0.082 | 1.398 | 0.046-0.276 | 0.047 |
| Combination vs. PCT | 0.101 | 0.055 | 1.835 | 0.007-0.208 | 0.049 |
| Combination vs. IL-6 | 0.227 | 0.081 | 2.793 | 0.081-0.387 | 0.005 |
| Combination vs. IVC-CI | 0.128 | 0.067 | 1.905 | 0.003-0.259 | 0.045 |
|
| 图 2 IVC-CI联合血清CRP、PCT、IL-6预测方案的DCA曲线 Fig.2 DCA curve of the prediction regimen based on the IVC-CI combined with serum CRP, PCT, and IL-6 detection |
3 讨论
研究[11]显示,急性胸腹创伤致死率约高达30%,患者早期即存在内脏损伤继而出现严重休克,这增加了患者死亡的风险。急性胸腹创伤往往为多发伤,且各处伤情不同,相互之间难以鉴别,诊断难度相对较大,极易出现漏诊现象。已有研究[12-13]指出,急诊医生主导的床旁超声FAST检测急性胸腹部创伤患者肝脾破裂、肾损伤等准确率可媲美CT检测,而且检测快速高效,可短时间内确定损伤类型,可为后续治疗提供依据,也为患者争取了宝贵的抢救时间。
严重创伤后组织损伤及失血均可导致炎症反应快速激活,释放损伤相关分子模式,该模式通过细胞表面受体直接激活单核细胞及中性粒细胞等免疫细胞,从而促炎症介质大量释放,产生炎症级联反应,这种全身性的失控式炎症反应称为全身炎症反应综合征。全身炎症反应综合征的发生是引起患者死亡的主要原因[14-15]。此外,创伤后感染同样也是严重创伤患者死亡的主要因素[16]。本研究结果显示,入院0 h、24 h及48 h死亡组血清CRP、PCT、IL-6水平均高于生存组(均P < 0.05);而且死亡组患者血清CRP、PCT、IL-6在入院0~48 h内持续升高,生存组患者血清CRP、PCT、IL-6入院24 h升至最高水平随后下降,提示入院0~48 h血清CRP、PCT、IL-6水平持续升高与急性胸腹创伤患者死亡有关。CRP属于急性时相蛋白,正常人体血液中含量极低,当机体受到外界刺激或感染时,肝细胞大量分泌、释放CRP至血液中,故创伤早期血液中CRP水平明显升高[17]。有研究[18]指出,创伤后感染患者血清CRP水平明显高于无感染患者,提示创伤后血清水平升高与感染密切相关。PCT属于多肽激素,是一种降钙素前肽,通常情况下在人体血液中较为稳定,含量极低。当机体发生感染时PCT在短时间内迅速升高。已有研究[19]发现PCT与创伤关系密切,且机体受伤后PCT可出现一定程度升高,升至峰值后可逐渐恢复正常,但若发生创伤性感染时血清PCT水平会持续升高。IL-6作为一种重要的炎症介质,可作用于微血管系统,促进内皮细胞收缩,增加血管通透性,引发白细胞浸润血管壁,造成毛细血管渗透及组织损伤。IL-6还可刺激肝细胞合成急性期反应蛋白,催化、放大炎症级联反应,致使组织细胞损伤。已有研究[20-21]证实,IL-6与创伤后感染、创伤后急性肝损伤等有关。IVC-CI可评估血流动力学,既往研究[22-23]指出,由急诊医生主导的超声FAST检测可反映创伤患者病情严重程度,其中IVC-CI与患者中心静脉压有关,可迅速反映病情进展。本研究结果显示,死亡组IVC-CI明显高于生存组,IVC-CI是影响患者结局的危险因素(P < 0.001),与既往研究结果一致。本研究结果显示,血清CRP、PCT、IL-6水平是影响急性胸腹部创伤患者结局的危险因素(均P < 0.001),提示急性胸腹创伤患者因伴有脏器功能损伤,应激反应较为剧烈,进而引发炎症级联反应,诱发创伤性感染,从而增加了患者住院期间死亡风险。
本研究结果显示,IVC-CI联合血清CRP、PCT、IL-6的AUC值大于各单独指标,可见联合方案可较好地预测急性胸腹创伤患者结局。另外,研究显示IVC-CI联合CRP、PCT、IL-6预测方案具有临床净获益,可为临床上患者治疗方案的调整提供参考依据。
综上所述,IVC-CI及血清CRP、PCT、IL-6水平与急性胸腹创伤患者临床结局相关;急诊医生主导的床旁超声FAST联合入院48 h血清CRP、PCT、IL-6检测可以预测急性胸腹部创伤患者的临床结局,且预测效能较好。本研究为单中心小样本研究,可能存在偏倚,今后有待临床多中心、多渠道取样,扩大样本量来进一步论证。
| [1] |
QUESADA D, MORSKY L, JONES A, et al. Pulmonary artery dissection post-blunt thoracoabdominal trauma[J]. Clin Pract Cases Emerg Med, 2020, 4(3): 466-467. DOI:10.5811/cpcem.2019.12.44649 |
| [2] |
MELISSANO G, MASCIA D, ATIQUE SG, et al. Treatment of acute thoracoabdominal aortic aneurysms[J]. J Cardiovasc Surg, 2017, 58(2): 228-237. DOI:10.23736/s0021-9509.16.09796-2 |
| [3] |
WANG PH, LIN HY, CHANG PY, et al. Focused assessment with sonography for trauma[J]. J Med Ultrasound, 2021, 29(3): 151-153. DOI:10.4103/jmu.jmu_128_21 |
| [4] |
MOLLY EW, THIESSEN MD, et al. Application of focused assessment with sonography for trauma in the intensive care unit[J]. Clin Chest Med, 2022, 43(3): 385-392. DOI:10.1016/j.ccm.2022.05.004 |
| [5] |
DEĞIRMENCI S, KARA H, KAYıŞ SA, et al. Role of ultrasound simulators in the training for focused assessment with sonography for trauma (FAST)[J]. Ulus Travma Acil Cerrahi Derg, 2021, 27(3): 303-309. DOI:10.14744/tjtes.2020.73626 |
| [6] |
王志华, 顾东明, 盛乐智, 等. 急诊创伤重点超声评估检查对腹部闭合性损伤患者诊断及休克预测价值[J]. 中国医学装备, 2018, 15(12): 89-92. DOI:10.3969/J.ISSN.1672-8270.2018.12.023 |
| [7] |
KONDO Y, OHBE H, YASUNAGA H, et al. Initial focused assessment with sonography in trauma versus initial CT for patients with haemodynamically stable torso trauma[J]. Emerg Med J, 2020, 37(1): 19-24. DOI:10.1136/emermed-2019-208537 |
| [8] |
李莲英, 刘凤娟, 丁密, 等. 胸部创伤患者早期血清调节性T淋巴细胞及Th1/Th2细胞因子变化与创伤后感染的关系[J]. 实用医学杂志, 2021, 37(15): 1967-1971. DOI:10.3969/j.issn.1006-5725.2021.15.012 |
| [9] |
康健, 郑富文, 王文娟, 等. 创伤超声重点评估在胸腹部创伤急救中的应用价值分析[J]. 中国急救复苏与灾害医学杂志, 2019, 14(10): 1004-1007. DOI:10.3969/j.issn.1673-6966.2019.10.028 |
| [10] |
王宾. 创伤急救评分联合创伤超声重点评估法在胸腹部多发伤患者救治中的应用价值[J]. 基层医学论坛, 2022, 26(4): 71-73. DOI:10.19435/j.1672-1721.2022.04.024 |
| [11] |
杨香森. 多层螺旋CT诊断急性胸腹部创伤的临床价值[J]. 深圳中西医结合杂志, 2020, 30(10): 67-68. DOI:10.16458/j.cnki.1007-0893.2020.10.033 |
| [12] |
周永江, 曹灵红, 江从兵, 等. 急诊床旁超声在胸腹部创伤急危重症患者的临床价值研究[J]. 实用医院临床杂志, 2022, 19(3): 125-127. DOI:10.3969/j.issn.1672-6170.2022.03.034 |
| [13] |
卢加发, 舒敏, 吴京兰, 等. 胸腹部创伤患者在院前行创伤超声重点评估的可行性[J]. 中华急诊医学杂志, 2020, 29(11): 1471-1475. DOI:10.3760/cma.j.issn.1671-0282.2020.11.016 |
| [14] |
CARDENAS JC. Thrombin generation following severe trauma: mechanisms, modulators, and implications for hemostasis and thrombosis[J]. Shock, 2021, 56(5): 682-690. DOI:10.1097/shk.0000000000001773 |
| [15] |
BALL CG. The Canadian-specific impact of COVID-19 on severe injuries from intentional violence, unintentional trauma and suicide-related causes[J]. Can J Surg, 2021, 64(2): E228-E229. DOI:10.1503/cjs.006321 |
| [16] |
COSTA ML, ACHTEN J, KNIGHT R, et al. Effect of incisional nega- tive pressure wound therapy vs standard wound dressing on deep surgical site infection after surgery for lower limb fractures associa- ted with major trauma[J]. JAMA, 2020, 323(6): 519. DOI:10.1001/jama.2020.0059 |
| [17] |
MERCURIO M, GALASSO O, FAMILIARI F, et al. Trend of perioperative CRP (C-reactive protein) levels in non-infected total knee arthroplasty[J]. Orthop Rev (Pavia), 2022, 14(4): 36589. DOI:10.52965/001c.36589 |
| [18] |
陈欣. D二聚体、C反应蛋白、血沉、血常规在创伤骨科患者围手术期治疗中的检测价值[J]. 血栓与止血学, 2022, 28(1): 116-117. DOI:10.3969/j.issn.1009-6213.2022.01.053 |
| [19] |
卢丹, 李红霞. 急诊外科腹部创伤患者术后切口感染病原学及血清细胞因子的诊断价值[J]. 中华医院感染学杂志, 2021, 31(24): 3752-3756. DOI:10.11816/cn.ni.2021-210274 |
| [20] |
吴俊学, 李毓灵, 陈路. IL-6、肿瘤坏死因子α及CRP对下肢创伤患者合并感染的预测价值分析[J]. 分子诊断与治疗杂志, 2020, 12(9): 1167-1170. DOI:10.3969/j.issn.1674-6929.2020.09.010 |
| [21] |
乔帅, 王晓磊, 刘俊清, 等. 内毒素、白细胞介素-6在重症胸腹损伤后急性肝损害发生中的作用[J]. 内蒙古医学杂志, 2020, 52(8): 902-903. DOI:10.16096/J.cnki.nmgyxzz.2020.52.08.003 |
| [22] |
PACE J, ARNTFIELD R. Focused assessment with sonography in trauma: a review of concepts and considerations for anesthesiology[J]. Can J Anesth, 2018, 65(4): 360-370. DOI:10.1007/s12630-017-1030-x |
| [23] |
ADI O, SUM KM, AHMAD AH, et al. Novel role of focused airway ultrasound in early airway assessment of suspected laryngeal trauma[J]. Ultrasound J, 2020, 12(1): 37. DOI:10.1186/s13089-020-00186-3 |
 2024, Vol. 53
2024, Vol. 53




