文章信息
- 张晓岚, 刘霄霄, 耿龙
- 以硬斑病样皮损为表现的线状皮肤型红斑狼疮1例报道并文献复习
- Linear cutaneous lupus erythematosus with morphea lesions as the manifestation: a case report and literature review
- 中国医科大学学报, 2024, 53(11): 1043-1046
- Journal of China Medical University, 2024, 53(11): 1043-1046
-
文章历史
- 收稿日期:2023-10-26
- 网络出版时间:2024-11-21 11:10:05
2. 中国医科大学附属第一医院皮肤科, 沈阳 110001
线状皮肤型红斑狼疮(liner cutaneous lupus erythematosus,LCLE)是红斑狼疮中一种极为罕见的亚型,主要发生于儿童和青年人,无明显的性别差异[1]。皮损通常沿Blaschko线分布,主要见于面部及四肢。临床表现通常为非对称性分布的线状红斑或丘疹,预后相对较好[2]。目前,国内外的相关病例报道很少。本文报道了中国医科大学附属第一医院收治的1例以硬斑病样皮损为表现的LCLE病例,并复习相关文献,探讨该病的发病机制及诊断与治疗方法,以期为LCLE的诊疗提供参考依据。
1 临床资料患者,男,5岁,以“枕部及后颈部线状白斑伴脱发1年”为主诉来中国医科大学附属第一医院皮肤科门诊就诊。患者1年前于枕部出现白斑,呈线状分布,伴有皮损处毛发脱失,无痛痒感,皮损逐渐蔓延至后颈部。于当地医院就诊,考虑为“硬斑病”,给予自制外用药物治疗,病情未见好转,故来我院就诊。患者病来无发热,无关节肿痛,无乏力等其他伴随症状。既往健康,足月儿,生长发育正常。家族中无遗传疾病。
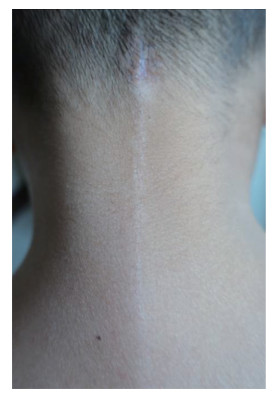
体格检查:发育正常,营养状况良好,系统查体未见异常。皮肤科查体:枕部及后颈部可见长度约10 cm线状白斑,白斑表面可见灶状萎缩,无鳞屑附着,枕部白斑处毛发缺失(图 1)。
|
| 图 1 患者枕部及后颈部皮损 |
实验室检查:血尿常规未见异常。抗核抗体(antinuclear antibody,ANA),抗史密斯(anti-Smith,Sm)抗体、抗干燥综合征A(anti-Sjӧgren syndrome A,SSA/Ro)抗体,抗干燥综合征B(anti-Sjӧgren syndrome B,SSB/La)抗体,抗双链DNA(anti-double-stranded DNA,ds-DNA)抗体,抗核糖核蛋白(anti-ribonucleoprotein,RNP)抗体,抗组氨酰-tRNA合成酶(anti-histidyl-tRNA synthetase,Jo-1)抗体,以及抗硬皮病70(anti-scleroderma 70,SCL-70)抗体检测均为阴性。
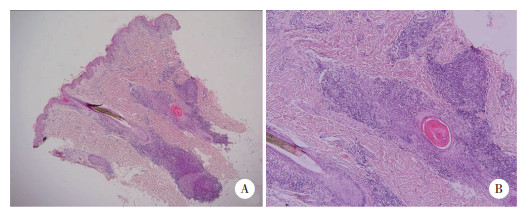
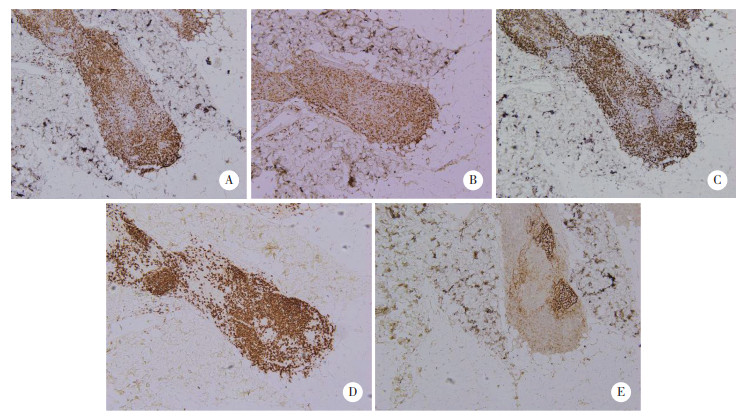
皮肤组织病理:表皮轻度萎缩,基底层灶状液化变性,真皮内血管及毛囊周围致密淋巴细胞浸润,呈结节状分布(图 2)。免疫组织化学检查:真皮内淋巴细胞主要表现为CD3、CD4、CD8阳性表达,毛囊周围见CD20和CD21阳性细胞呈结节状分布。EB病毒编码RNA(Epstein-Barr virus encoded RNA,EBER)阴性(图 3)。直接免疫荧光检查:IgA、IgM、IgG、C3在真皮、表皮内均为阴性表达。
|
| A,皮损处组织病理表现为表皮轻度萎缩,基底层灶状液化变性,真皮内血管及毛囊周围致密淋巴细胞浸润(×40);B,毛囊及血管周围可见结节状分布的淋巴细胞浸润(×100). 图 2 皮损处组织病理图像 HE染色 |
|
| 真皮内淋巴细胞主要表现为CD3(A)、CD4(B)、CD8(C)阳性表达,毛囊周围见CD20(D)和CD21(E)阳性细胞呈结节状分布. 图 3 皮损处免疫组织化学图像 ×100 |
结合临床表现,实验室检查及病理结果,诊断为LCLE。鉴别诊断见表 1。明确诊断后给予患者糠酸莫米松乳膏适量(2次/d)外用于皮损处,3周后皮损较前明显缩小,而后改为0.03%他克莫司乳膏适量(2次/d)外用于皮损处。目前患者仍在随访中。本研究获得锦州医科大学附属第一医院医学研究伦理委员会批准,患者及其家属知情同意。
2 讨论
LCLE是红斑狼疮中的一种罕见的变异型。1978年由UMBERT等[6]第一次作为皮肤型红斑狼疮的线性变异型提出,1998年ABE等[7]将其正式命名为LCLE。早期报道的案例通常多为沿Blaschko线分布的盘状红斑狼疮,不引起系统受累[8-9],而后逐渐发现狼疮性脂膜炎、大疱性红斑狼疮、亚急性红斑狼疮等皮损也可沿线状排列[10-12]。故2000年ABE等[13]将其统称为LCLE。该病多发生在儿童和青少年,男女发病比例约为1∶1.3[14]。该病的发病机制目前尚不明确。JIN等[15]曾提出LCLE发病模式与角质形成细胞出现遗传镶嵌/表观遗传修饰以及角质形成细胞凋亡学说等有关。其中,角质形成细胞凋亡学说是促进LCLE发病的一种重要因素。遗传变异的角质形成细胞缺乏调控细胞凋亡所需的蛋白,从而导致主要组织相容性复合体(major histocompatibility complex,MHC)表达异常和细胞因子异常释放,进而导致LCLE发生[16]。感染、药物、紫外线照射、创伤因素也会通过诱导Blaschko线上的角质形成细胞表达相关抗原,引起皮肤型红斑狼疮的发病[17-19]。
LCLE发病较少,近年来国外报道约60例,国内报道约20例。复习相关文献[20]发现,LCLE的平均发病年龄约9岁,病程不等,约2个月~20余年。LCLE的好发部位分别为头颈部(57%)、四肢(46%)和躯干部(14%),也有少数患者会在多个部位出现皮损[21]。其皮损特点通常为沿Blaschko线分布的红色或紫红色的斑块,表面可附着白色鳞屑,通常不伴有系统受累[22]。少数患者也会出现皮肤钙质沉积或粟丘疹的改变[23]。实验室检查方面,文献[24-25]报道中多数患者ANA表达阴性或弱阳性。而本例患者发病部位为头皮及颈部,皮损表现为线状分布的白斑,表面萎缩,呈羊皮纸状外观,且伴随局部脱发,曾于当地医院误诊为硬斑病,是LCLE的一种较为罕见的临床表现,目前尚无类似报道。
LCLE的组织病理学改变包括角化过度,表皮萎缩,基底细胞液化变性,真皮内血管、毛囊等附属器周围有密集的淋巴细胞浸润[26]。部分深在性红斑狼疮病理可见脂肪小叶内的淋巴细胞浸润[27]。直接免疫荧光可表现为IgG、IgM、IgA或C3在真皮、表皮交接处和附属器周围呈颗粒状沉积。但免疫荧光结果阴性并不能排除该病[28]。因此,临床中通过皮肤病理和直接免疫荧光结果可与硬斑病、线状银屑病、线状扁平苔藓等鉴别。本例患者的皮损符合皮肤红斑狼疮病理改变,且免疫组织化学检查结果提示附属器周围以T淋巴细胞及B淋巴细胞混合性浸润为主,结合患者的临床表现,诊断为LCLE。
局限性LCLE的治疗以外用强效激素及防晒为主[29],也可外用钙调免疫抑制剂作为维持治疗[30]。对于多发性LCLE则需要系统治疗,羟氯喹为首选药物[31]。对于羟氯喹反应差的患者,可选择氨苯砜或者甲氨蝶呤口服配合中强效激素软膏外用进行治疗[32-33]。本例患者皮损局限,且无其他系统症状,因此首选糠酸莫米松乳膏外用3周,治疗后皮损较前明显好转,而后改为0.03%他克莫司乳膏外用于皮损处维持治疗。
| [1] |
REAGIN H, NGUYEN DA, LEWIN MR, et al. Linear cutaneous lupus erythematosus following blaschko's lines on the scalp: additional cases and review of the literature[J]. HCA Healthc J Med, 2022, 3(2): 51-62. DOI:10.36518/2689-0216.1308 |
| [2] |
MILOSAVLJEVIC K, FIBEGER E, VIRATA AR. A case of linear cutaneous lupus erythematosus in a 55-year-old woman[J]. Am J Case Rep, 2020, 21: e921495. DOI:10.12659/AJCR.921495 |
| [3] |
PEÑA-ROMERO AG, GARCÍA-ROMERO MT. Diagnosis and management of linear scleroderma in children[J]. Curr Opin Pediatr, 2019, 31(4): 482-490. DOI:10.1097/MOP.0000000000000785 |
| [4] |
ONOUFRIADIS A, NIAZI U, DIMITRAKOPOULOU K, et al. Transcriptomic analysis of blaschko-linear psoriasis reveals shared and distinct features with psoriasis vulgaris[J]. J Invest Dermatol, 2022, 142(2): 489-493. DOI:10.1016/j.jid.2021.07.007 |
| [5] |
MERIO L, TOUNKARA TM, BATTESTI G, et al. Blaschko-linear lichen planus of the face: a retrospective study of 6 cases and a literature review[J]. Ann Dermatol Venereol, 2022, 149(2): 112-118. DOI:10.1016/j.annder.2021.08.003 |
| [6] |
UMBERT P, WINKELMANN RK. Concurrent localized scleroderma and discoid lupus erythematosus.Cutaneous 'mixed' or 'overlap' syndrome[J]. Arch Dermatol, 1978, 114(10): 1473-478. DOI:10.1001/archderm.1978.01640220022005 |
| [7] |
ABE M, ISHIKAWA O, MIYACHI Y. Linear cutaneous lupus erythematosus following the lines of Blaschko[J]. Br J Dermatol, 1998, 139(2): 307-310. DOI:10.1046/j.1365-2133.1998.02373.x |
| [8] |
VERMA SB, WOLLINA U. Chronic disseminated discoid lupus erythematosus with linear lesions following Blaschko's lines on forearm and hand[J]. J Dtsch Dermatol Ges, 2012, 10(2): 129-130. DOI:10.1111/j.1610-0387.2011.07795.x |
| [9] |
DALDON PEC, LAGE RN. Linear chronic discoid lupus erythematosus following the lines of Blaschko[J]. An Bras Dermatol, 2011, 86(3): 553-556. DOI:10.1590/s0365-05962011000300020 |
| [10] |
TAMADA Y, ARISAWA S, IKEYA T, et al. Linear lupus erythematosus profundus in a young man[J]. Br J Dermatol, 1999, 140(1): 177-178. DOI:10.1046/j.1365-2133.1999.02636.x |
| [11] |
VASSILEVA S. Bullous systemic lupus erythematosus[J]. Clin Dermatol, 2004, 22(2): 129-138. DOI:10.1016/j.clindermatol.2003.12.020 |
| [12] |
RÖCKMANN H, FELLER G, SCHADENDORF D, et al. Subacute cutaneous lupus erythematosus on the lines of Blaschko[J]. Eur J Dermatol, 2006, 16(3): 302-306. |
| [13] |
ABE M, OHNISHI K, ISHIKAWA O. Guess what? Linear cutaneous lupus erythematous (LCLE): relationship with Blaschko's lines[J]. Eur J Dermatol, 2000, 10(3): 229-231. |
| [14] |
SINDHUSEN S, CHANPRAPAPH K, RUTNIN S. Adult-onset linear discoid lupus erythematosus on the forehead mimicking en coup de sabre: a case report[J]. J Med Case Rep, 2019, 13(1): 350. DOI:10.1186/s13256-019-2249-7 |
| [15] |
JIN H, ZHANG GY, ZHOU Y, et al. Old lines tell new tales: blaschko linear lupus erythematosis[J]. Autoimmun Rev, 2016, 15(4): 291-306. DOI:10.1016/j.autrev.2015.11.014 |
| [16] |
SEITZ CS, BRÖCKER EB, TRAUTMANN A. Linear variant of chronic cutaneous lupus erythematosus: a clue for the pathogenesis of chronic cutaneous lupus erythematosus?[J]. Lupus, 2008, 17(12): 1136-1139. DOI:10.1177/0961203308092425 |
| [17] |
SHAPIRO M, SOSIS AC, JUNKINS-HOPKINS JM, et al. Lupus erythematosus induced by medications, ultraviolet radiation, and other exogenous agents: a review, with special focus on the development of subacute cutaneous lupus erythematosus in a genetically predisposed individual[J]. Int J Dermatol, 2004, 43(2): 87-94. DOI:10.1111/j.1365-4632.2004.02013.x |
| [18] |
AIYAMA A, MURO Y, SUGIURA K, et al. Extraordinarily long linear cutaneous lupus erythematosus along the lines of Blaschko[J]. Dermatol Online J, 2013, 19(7): 18960. DOI:10.5070/D3197018960 |
| [19] |
ZANDMAN-GODDARD G, SOLOMON M, ROSMAN Z, et al. Environment and lupus-related diseases[J]. Lupus, 2012, 21(3): 241-250. DOI:10.1177/0961203311426568 |
| [20] |
CAMPOS-MUÑOZ L, FUEYO-CASADO A, CONDE-TABOADA A, et al. Clinical Images: progressive linear blaschkoid lupus erythematosus[J]. Arthritis Rheumatol, 2017, 69(11): 2250. DOI:10.1002/art.40172 |
| [21] |
MARINHO AK, RAMOS TB, BARBOSA DM, et al. Linear cutaneous lupus erythematosus following the lines of Blaschko - case report[J]. An Bras Dermatol, 2016, 91(4): 510-513. DOI:10.1590/abd1806-4841.20163800 |
| [22] |
LEE SK, BAEK J, ROH JY, et al. Clinical characteristics of pediatric cutaneous lupus erythematosus: experience from a tertiary referral center in Korea[J]. Lupus, 2019, 28(7): 888-892. DOI:10.1177/0961203319851568 |
| [23] |
MA H, LIAO MS, QIU S, et al. Linear cutaneous lupus erythematosus with calcinosis cutis and milia[J]. Pediatr Dermatol, 2015, 32(1): e33-e35. DOI:10.1111/pde.12496 |
| [24] |
GAITANIS G, NOMIKOS K, CHANIOTAKIS I, et al. Linear cutaneous lupus erythematosus: a subset of childhood cutaneous lupus erythematosus[J]. Lupus, 2009, 18(8): 759-761. DOI:10.1177/0961203308100509 |
| [25] |
CAMPOS-MUÑOZ L, FUEYO-CASADO A, CONDE-TABOADA A, et al. Clinical Images: progressive linear blaschkoid lupus erythematosus[J]. Arthritis Rheumatol, 2017, 69(11): 2250. DOI:10.1002/art.40172 |
| [26] |
MOWLA MR, BARUA DP, ZAMAN S, et al. Clinicopathological characteristics of cutaneous lupus erythematosus patients in Bangladesh[J]. Postepy Dermatol Alergol, 2022, 39(4): 782-787. DOI:10.5114/ada.2021.110254 |
| [27] |
RANGEL LK, VILLA-RUIZ C, LO K, et al. Clinical characteristics of lupus erythematosus panniculitis/profundus: a retrospective review of 61 patients[J]. JAMA Dermatol, 2020, 156(11): 1264-1266. DOI:10.1001/jamadermatol.2020.2797 |
| [28] |
BITAR C, MENGE TD, CHAN MP. Cutaneous manifestations of lupus erythematosus: a practical clinicopathological review for pathologists[J]. Histopathology, 2022, 80(1): 233-250. DOI:10.1111/his.14440 |
| [29] |
LU QJ, LONG H, CHOW S, et al. Guideline for the diagnosis, treatment and long-term management of cutaneous lupus erythematosus[J]. J Autoimmun, 2021, 123: 102707. DOI:10.1016/j.jaut.2021.102707 |
| [30] |
KER KJ, TESKE NM, FENG R, et al. Natural history of disease activity and damage in patients with cutaneous lupus erythematosus[J]. J Am Acad Dermatol, 2018, 79(6): 1053-1060.e3. DOI:10.1016/j.jaad.2018.06.040 |
| [31] |
SHI H, GUDJONSSON JE, KAHLENBERG JM. Treatment of cutaneous lupus erythematosus: current approaches and future strategies[J]. Curr Opin Rheumatol, 2020, 32(3): 208-214. DOI:10.1097/BOR.0000000000000704 |
| [32] |
BLAKE SC, DANIEL BS. Cutaneous lupus erythematosus: a review of the literature[J]. Int J Womens Dermatol, 2019, 5(5): 320-329. DOI:10.1016/j.ijwd.2019.07.004 |
| [33] |
KUHN A, OCHSENDORF F, BONSMANN G. Treatment of cutaneous lupus erythematosus[J]. Lupus, 2010, 19(9): 1125-1136. DOI:10.1177/0961203310370345 |
 2024, Vol. 53
2024, Vol. 53




