文章信息
- 陈瑞珠, 张欢, 郑立春, 刘丽云, 欧阳向柳
- CHEN Ruizhu, ZHANG Huan, ZHENG Lichun, LIU Liyun, OUYANG Xiangliu
- 超声联合细针穿刺洗脱液甲状腺球蛋白测定在甲状腺乳头状癌颈部淋巴结转移诊断中的应用
- Ultrasound combined with FNA-Tg in the diagnosis of cervical lymph node metastasis in papillary thyroid carcinoma
- 中国医科大学学报, 2024, 53(11): 999-1004, 1011
- Journal of China Medical University, 2024, 53(11): 999-1004, 1011
-
文章历史
- 收稿日期:2023-09-19
- 网络出版时间:2024-11-21 11:03:18
2. 华北理工大学研究生学院, 河北 唐山 063000;
3. 唐山市工人医院核医学科, 河北 唐山 063000;
4. 唐山市工人医院病理科, 河北 唐山 063000
2. Graduate School of North China University of Science and Technology, Tangshan 063000, China;
3. Department of Nuclear Medicine, Tangshan Gongren Hospital, Tangshan 063000, China;
4. Department of Pathology, Tangshan Gongren Hospital, Tangshan 063000, China
甲状腺乳头状癌(papillary thyroid carcinoma,PTC)是发生于甲状腺滤泡上皮细胞的恶性肿瘤,是最常见的分化型甲状腺癌(differentiated thyroid carcinoma,DTC)[1],发病率占全部DTC的80%。PTC分化程度高,但容易发生颈部淋巴结转移,早期准确诊断颈部淋巴结是否转移能够影响术中淋巴结清扫范围,对患者的术式选择及术后生活质量十分重要。超声是甲状腺癌诊断最常见并且首选的影像学检查[2],2023年我国最新指南[3]指出甲状腺结节恶性或者可疑恶性者均应进行颈部淋巴结超声检查,但其诊断效能受操作者主观因素及经验水平影响较大。甲状腺球蛋白(thyroglobulin,Tg)是甲状腺滤泡上皮细胞分泌的特异性糖蛋白,是DTC术后转移和复发的重要检测指标。血清学Tg是最常用的检查方法,但容易受Tg抗体的影响,对转移淋巴结诊断效能不高。超声引导下细针穿刺洗脱液Tg测定(thyroglobulin measurement in fine-needle aspiration biopsy,FNA-Tg)是近年来发展的新技术,对PTC颈部淋巴结转移的灵敏度和特异度均较高[4-5]。本研究分析PTC患者术前可疑转移的颈侧区淋巴结超声表现,并对比超声、FNA-Tg及二者联合应用的诊断效能,旨在为术前颈侧区淋巴结转移准确诊断提供依据。
1 材料与方法 1.1 临床资料收集2017年1月至2023年3月唐山市工人医院130例(共144枚淋巴结)进行颈部淋巴结清扫术PTC患者的临床资料。其中男37例、女93例,年龄15~75岁,平均(45±13)岁。纳入标准:(1)术后病理确诊为PTC;(2)术前对可疑淋巴结行超声、超声引导下FNA-Tg及血清Tg检测;(3)可疑转移淋巴结位于颈侧区并明确病理诊断。本研究获得唐山市工人医院医学伦理委员会批准(批号:GRYY-LL-2019-38),患者均知情同意并签署知情同意书。
1.2 仪器与方法 1.2.1 超声检查患者充分暴露预穿刺部位并呈仰卧位,采用Philips EPIQ 7型超声诊断仪,使用频率为5~12 MHz的线阵探头,对颈部淋巴结的大小,横纵比(短轴与长轴的比值),边缘是否清楚,淋巴门结构是否清晰,内部回声是否均匀,是否伴有囊性变、钙化、异常血流进行评估并记录。超声诊断标准:怀疑存在甲状腺恶性结节且颈部淋巴结具备如下特征之一(包括皮髓质分界不清,皮质局部或弥漫性回声增强,伴有囊性变、微钙化,血流杂乱丰富)时诊断为转移淋巴结。
1.2.2 超声引导下细针抽吸活检(fine-needle aspiration biopsy,FNAB)采用Philips EPIQ 7型超声诊断仪,使用频率为5~12 MHz的线阵探头,患者充分暴露预穿刺部位并呈仰卧位,常规消毒、铺巾后局部麻醉,经超声对可疑淋巴结进行常规评估后,在超声引导下采用23G穿刺针对可疑淋巴结进行反复多点抽吸穿刺,连续穿刺3针以上;将穿刺针芯内细胞迅速涂片并注入试管处理,然后送病理科进行细胞学检查;穿刺部位局部按压15~20 min。
1.2.3 血清Tg及洗脱液Tg的制备及检测用1 mL生理盐水对23G穿刺针内的穿刺液进行反复冲洗3次以上并振荡混匀;患者同期采取静脉血5 mL;将混匀好的标本和静脉血以3 000 r/min离心5 min后,利用Mindray CL-2000i仪对血清Tg及洗脱液Tg进行全自动化学发光免疫分析。
FNA-Tg诊断根据本组数据绘制受试者操作特征(receiver operation characteristic,ROC)曲线得出的最佳临界值进行区分,≥临界值为阳性;< 临界值为阴性。超声联合FNA-Tg诊断标准:超声和FNA-Tg二者中任一个阳性即为超声联合FNA-Tg阳性诊断。
1.2.4 穿刺淋巴结标记超声引导下淋巴结穿刺后,采用细针在穿刺淋巴结内注入约0.1 mL纳米碳混悬液(重庆莱美药业股份有限公司)进行标记,同时记录淋巴结的大小及位置,以便手术清扫过程中能够准确找到标记淋巴结。
1.3 统计学分析应用SPSS 26.0软件进行数据统计分析。符合正态分布的计量资料以x±s表示,组间比较采用t检验;不符合正态分布的计量资料以M(P25~P75)表示,组间比较采用Mann-WhitneyU检验。计数资料以率(%)表示,组间比较采用χ2检验或Fisher精确概率法。以FNAB或者淋巴结清扫术后病理结果为标准,绘制超声、FNA-Tg及二者联合诊断的ROC曲线。P < 0.05为差异有统计学意义。
2 结果病理检测结果显示,144枚淋巴结中,转移性淋巴结(转移组)64枚,非转移性淋巴结(非转移组)80枚。
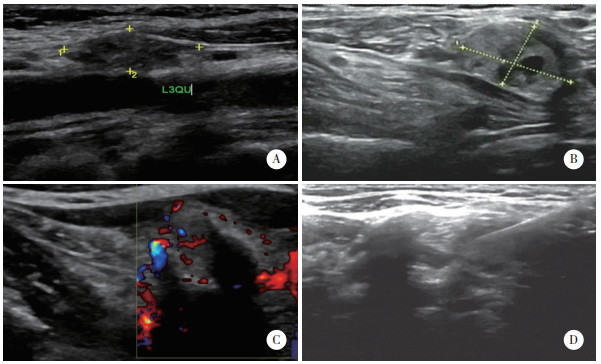
2.1 2组超声指标比较结果显示,转移组和非转移组淋巴结长径、横纵比、边缘是否清楚比较差异无统计学意义(均P > 0.05)。与非转移组比较,转移组淋巴结多皮髓质分界不清、内部回声不均匀、伴有囊性变、微钙化和存在异常血流信号比例均显著增高,差异有统计学意义(均P < 0.05),见表 1、图 1。
| Ultrasonic characteristics | Metastasis group(n = 64) | Non-metastasis group(n = 80) | Z/χ2 | P |
| Diameter(cm) | 1.1(0.7-1.6) | 1.0(0.5-1.8) | 1.086 | 0.277 |
| Cross-vertical ratio [n(%)] | 2.162 | 0.141 | ||
| ≥0.5 | 25(39.1) | 22(27.5) | ||
| < 0.5 | 39(60.9) | 58(72.5) | ||
| Regular margin [n(%)] | 1.777 | 0.183 | ||
| Yes | 57(89.1) | 76(95.0) | ||
| No | 7(10.9) | 4(5.0) | ||
| Corticomedullary differentiation [n(%)] | 13.869 | < 0.001 | ||
| Yes | 40(62.5) | 71(88.8) | ||
| No | 24(37.5) | 9(11.2) | ||
| Homogeneous echo [n(%)] | 17.280 | < 0.001 | ||
| Uniform | 28(43.8) | 62(77.5) | ||
| Nonuniform | 36(56.2) | 18(22.5) | ||
| Cystic [n(%)] | 8.018 | 0.005 | ||
| Yes | 10(15.6) | 2(2.5) | ||
| No | 54(84.4) | 78(97.5) | ||
| Macrocalcification [n(%)] | 11.859 | 0.001 | ||
| Yes | 28(43.8) | 14(17.5) | ||
| No | 36(56.2) | 66(82.5) | ||
| Abnormal blood flow [n(%)] | 6.061 | 0.014 | ||
| Yes | 38(59.4) | 31(38.8) | ||
| No | 26(40.6) | 49(61.2) |
|
| A, lymph nodes with indistinct corticomedullary demarcation and enhanced parenchymal echogenicity; B, lymph nodes with microcalcifications and cystic degeneration; C, lymph node portal structures eliminated with heterogeneous and abundant blood flow; D, metastatic lymph nodes by FNAB. 图 1 48岁男性PTC患者颈侧区淋巴结转移超声图像 Fig.1 Ultrasound image of lymph node metastasis in the lateral cervical region of a 48-year-old male patient with PTC |
2.2 2组血清Tg及洗脱液Tg水平比较
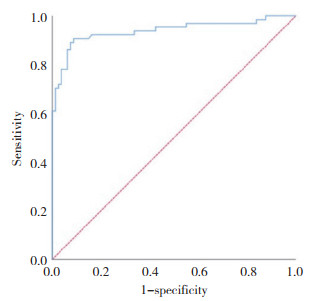
结果显示,2组血清Tg水平比较差异没有统计学意义(P = 0.898);而洗脱液Tg水平比较差异有统计学意义(P < 0.001)。洗脱液Tg诊断颈侧区淋巴结转移的ROC曲线分析结果显示,最佳临界值为11.7 ng/mL,即洗脱液Tg≥11.7 ng/mL为诊断阳性,洗脱液Tg < 11.7 ng/mL时为诊断阴性,对应ROC曲线下面积(area under curve,AUC)为0.938(95%CI:0.893~0.981,P < 0.001),见表 2、图 2。
| Item | Metastasis group(n = 64) | Non-metastasis group(n = 80) | Z | P |
| Serum Tg | 19.5(1.9-70.7) | 20.4(8.9-38.3) | 0.129 | 0.898 |
| Eluate Tg | 500.0(49.4-500.0) | 2.4(0.6-6.5) | 9.068 | < 0.001 |
|
| 图 2 FNA-Tg诊断颈侧区淋巴结转移的ROC曲线 Fig.2 ROC curve of FNA-Tg for the diagnosis of lymph node metastasis in the lateral cervical region |
2.3 超声、FNA-Tg及二者联合的诊断效能比较
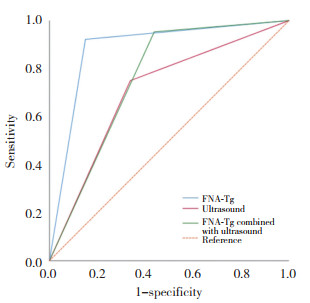
超声、FNA-Tg及二者联合诊断颈侧区淋巴结转移的AUC为分别为0.706(95%CI:0.620~0.793,P < 0.001)、0.909(95%CI:0.855~0.964,P < 0.001)、0.758(95%CI:0.679~0.837,P < 0.001)。二者联合诊断的灵敏度最高,为95.3%。3种方法灵敏度、特异度、准确度、阳性预测值及阴性预测值比较差异均有统计学意义(均P < 0.05)见表 3,图 3。
| Examination methods | Pathology result | Sensitivity(%) | Specificity(%) | Accuracy(%) | Positive predictive value(%) | Negative predictive value(%) | |
| + | - | ||||||
| Ultrasound | 75.0(48/64) | 66.3(53/80) | 70.1(101/144) | 64.0(48/75) | 76.8(53/69) | ||
| + | 48 | 27 | |||||
| - | 16 | 53 | |||||
| FNA-Tg | 90.6(58/64) | 91.3(73/80) | 91.0(131/144) | 89.2(58/65) | 92.4(73/79) | ||
| + | 58 | 7 | |||||
| - | 6 | 73 | |||||
| FNA-Tg combined with ultrasound | 95.3(61/64) | 56.3(45/80) | 73.6(106/144) | 63.5(61/96) | 93.8(45/48) | ||
| + | 61 | 35 | |||||
| - | 3 | 45 | |||||
| χ2 | 12.785 | 25.385 | 21.075 | 14.793 | 10.465 | ||
| P | 0.002 | < 0.001 | < 0.001 | 0.001 | 0.005 | ||
|
| 图 3 超声、FNA-Tg及二者联合诊断颈侧区淋巴结转移的ROC曲线 Fig.3 ROC curves for ultrasound, FNA-Tg, and their combination for the diagnosis of lymph node metastases in the lateral cervical region |
3 结论
甲状腺癌是临床上最常见的甲状腺恶性肿瘤,女性发病率是男性的3~4倍,其中最常见类型为PTC。PTC分化程度高,预后较好[6-9],患者10年生存率达90%以上,但是20%~50%患者确诊时已发生颈部淋巴结转移[10]。甲状腺癌颈部淋巴结清扫手术容易累及周围神经引起并发症[11],所以术前准确诊断淋巴结是否转移可优化手术策略并调整淋巴结的清扫范围,从而减少并发症的发生,对患者的预后及生活质量意义重大。
超声检查能够评估淋巴结形态、大小、回声及血流信号等特征,是颈部淋巴结常规检查中的首选方法。众多研究[12-13]显示,淋巴结横纵比≥0.5、淋巴门结构不清、伴有囊性变、微钙化等特征有助于诊断转移性淋巴结。横纵比增大是肿瘤细胞在淋巴结内多沿短轴生长变成圆形所致,可破坏淋巴结正常的淋巴门结构;囊性变是细胞发生液化变性或者胶质沉积造成的。本研究结果显示,转移组与非转移组间皮髓质分界不清楚,回声不均匀,伴有囊性变、微钙化、异常血流信号比较有统计学差异,与以往研究[14]结果一致。彩色多普勒超声上转移淋巴结多表现为高阻血流,这是由于肿瘤细胞在浸润淋巴结过程中不断扩大导致肿瘤边缘及间隙出现新生血管,所以血流常不规则,当新生小血管受到挤压时就会呈现为高阻血流[15]。本研究结果显示,2组淋巴结横纵比比较差异无统计学意义(P > 0.05),这可能是非转移组淋巴结因炎症等原因表现为皮质增厚造成的淋巴结增大所致。超声具有方便、简洁、无射线、费用低、可实时重复检查等优点,在甲状腺结节及颈部淋巴结的良恶性判断方面显示出巨大的优势。但淋巴结超声检查缺少定量判断指标,受操作者主观影响较大。
Tg是甲状腺组织分泌并储存在滤泡腔内的特异性糖蛋白分子,非甲状腺组织表达时提示异常,因此甲状腺癌全切术后患者Tg增高可以提示复发及转移[16]。目前,最常用的检查方法是测定血清Tg,但是因其可以与抗甲状腺球蛋白抗体(antithyroglobulin antibody,TgAb)结合从而影响准确性[17]。本研究中转移组与非转移组血清Tg比较差异无统计学意义(P > 0.05),不能作为术前判定颈部淋巴结转移的标准,与既往研究[5]结果一致。洗脱液Tg是通过超声引导下淋巴结细针穿刺获取标本并测量获得的,避免了血清中促甲状腺激素、TgAb的影响。有研究[18]表明FNA-Tg对颈部淋巴结转移的诊断灵敏度和特异度明显高于血清Tg。对于血清Tg与洗脱液Tg间的关系尚且存在争议,有研究[19]认为二者间没有相关性,但是也有研究[20]指出高血清Tg水平与洗脱液Tg呈正相关,这可能是在穿刺过程中血清中的Tg进入穿刺针芯造成洗脱液Tg异常增高所致。本研究结果显示,FNA-Tg判定淋巴结转移的最佳临界值为11.7 ng/mL(95%CI:0.893~0.981,P < 0.001),与美国甲状腺学会指南[21]中指出的FNA-Tg > 10 ng/mL时为阳性接近,因此认为FNA-Tg > 11.7 ng/mL时可以判定颈部淋巴结转移。
超声、FNA-Tg及二者联合诊断淋巴结转移的诊断效能比较结果显示,FNA-Tg诊断效能最高,其特异度、准确性及阳性预测值分别为91.3%、91.0%、89.2%;二者联合诊断的灵敏度和阴性预测值最高,达到95.3%、93.8%。超声的诊断效能相对较低,灵敏度和特异度只有75.0%、66.3%,可能是由于解剖结构复杂造成超声对颈侧区淋巴结转移诊断不敏感[22]。另外,超声不能够探查较深的组织和淋巴结,从而导致超声诊断的假阴性率过高。除此之外,超声检查受操作者影响较大,不同的探查手法和方向可能导致部分淋巴结漏诊,对于病变的描述也受主观性影响,无客观定量指标进行诊断。FNA-Tg避免了主观因素影响,在诊断PTC颈部转移淋巴结中更为准确。本研究中FNA-Tg诊断假阴性淋巴结有6枚,这可能是因为淋巴结处于转移早期仅累及部分淋巴结区域,穿刺时未穿刺到转移部分造成的,这提示在淋巴结穿刺抽吸时应进行多点、多次抽吸,从而增加取材满意度。
本研究的局限性:(1)未对血清Tg和FNA-Tg取样操作方法带来的误差进行深入分析;(2)样本量较小,需要多中心大样本进行进一步论证。
综上所述,PTC颈部淋巴结转移的超声表现有一定特征,常表现为边界清楚的肿大淋巴结,皮髓质分界不清,内部回声不均匀,常伴囊性变、微钙化、不规则或者条带状丰富异常血流,当PTC患者颈部淋巴结出现这些征象时提示有转移的可能。FNA-Tg具有较高的诊断效能,当FNA-Tg > 11.7 ng/mL时可以判定颈部淋巴结转移。临床工作中超声怀疑PTC颈部淋巴结异常时,应进一步进行FNA-Tg,二者联合应用可能有助于提高PTC颈部淋巴结转移的诊断效能。
| [1] |
KITAHARA CM, SOSA JA. The changing incidence of thyroid cancer[J]. Nat Rev Endocrinol, 2016, 12(11): 646-653. DOI:10.1038/nrendo.2016.110 |
| [2] |
ALEXANDER EK, CIBAS ES. Diagnosis of thyroid nodules[J]. Lancet Diabetes Endocrinol, 2022, 10(7): 533-539. DOI:10.1016/S2213-8587(22)00101-2 |
| [3] |
中华医学会内分泌学分会, 中华医学会外科学分会甲状腺及代谢外科学组, 中国抗癌协会头颈肿瘤专业委员会, 等. 甲状腺结节和分化型甲状腺癌诊治指南(第二版)[J]. 中华内分泌代谢杂志, 2023, 39(3): 181-226. DOI:10.3760/cma.j.cn311282-20221023-00589 |
| [4] |
杨汶士, 张艳, 张凤凤, 等. 细针穿刺洗脱液测定甲状腺球蛋白和细针穿刺细胞学诊断甲状腺乳头状癌颈部淋巴结转移的Meta分析[J]. 肿瘤研究与临床, 2022, 34(2): 137-141. DOI:10.3760/cma.j.cn115355-20210711-00304 |
| [5] |
WU XL, LIU Y, LI KJ, et al. Predictive value of FNA-Tg and TgAb in cervical lymph node metastasis of papillary thyroid carcinoma[J]. Technol Cancer Res Treat, 2022, 21: 15330338221127605. DOI:10.1177/15330338221127605 |
| [6] |
王莎莎, 石远凯, 韩晓红. FNA-Tg检测分化型甲状腺癌淋巴结转移的诊断效能及其影响因素[J]. 中华检验医学杂志, 2020, 43(6): 670-677. DOI:10.3760/cma.j.cn114452-20200213-00068 |
| [7] |
PIZZATO M, LI MM, VIGNAT J, et al. The epidemiological landscape of thyroid cancer worldwide: globocan estimates for incidence and mortality rates in 2020[J]. Lancet Diabetes Endocrinol, 2022, 10(4): 264-272. DOI:10.1016/S2213-8587(22)00035-3 |
| [8] |
MIRANDA-FILHO A, LORTET-TIEULENT J, BRAY F, et al. Thyroid cancer incidence trends by histology in 25 countries: a population-based study[J]. Lancet Diabetes Endocrinol, 2021, 9(4): 225-234. DOI:10.1016/S2213-8587(21)00027-9 |
| [9] |
BALOCH ZW, ASA SL, BARLETTA JA, et al. Overview of the 2022 WHO classification of thyroid neoplasms[J]. Endocr Pathol, 2022, 33(1): 27-63. DOI:10.1007/s12022-022-09707-3 |
| [10] |
陈易来, 陈煜东, 詹维伟, 等. 甲状腺乳头状癌转移性淋巴结大小与FNA-Tg测值的关系[J]. 分子影像学杂志, 2024, 47(3): 237-241. |
| [11] |
PINO A, MAZZEO C, FRATTINI F, et al. Lymph node dissection morbidity in thyroid cancer: an integrative review[J]. Sisli Etfal Hastan Tip Bul, 2021, 55(4): 433-437. DOI:10.14744/SEMB.2021.33401 |
| [12] |
CHASEN NN, WANG JR, GAN Q, et al. Imaging of cervical lymph nodes in thyroid cancer: ultrasound and computed tomography[J]. Neuroimaging Clin N Am, 2021, 31(3): 313-326. DOI:10.1016/j.nic.2021.04.002 |
| [13] |
ÇETIN TUNÇEZ H, MURATKOÇ A, HILAL ADıBELLI Z, et al. Diagnostic efficacy of ultrasonography, Doppler ultrasonography and elastography in the evaluation of suspected malignant lymph nodes[J]. J Ultrason, 2023, 23(92): 1-9. DOI:10.15557/JoU.2023.0001 |
| [14] |
陈思. 超声特征联合FNAC、FNA-Tg对分化型甲状腺癌术后颈部淋巴结转移的预测价值及临床指导作用[D]. 广州: 南方医科大学, 2022. DOI: 10.27003/d.cnki.gojyu.2022.000952.
|
| [15] |
李俨育, 王茜, 范公林, 等. 基于超声与细针穿刺洗脱液甲状腺球蛋白检测建立甲状腺乳头状癌颈侧区淋巴结转移的预测模型[J]. 中华超声影像学杂志, 2020, 29(2): 131-137. DOI:10.3760/cma.j.issn.1004-4477.2020.02.006 |
| [16] |
LIM JH, KIM DW, PARK JY, et al. Ultrasonography, cytology, and thyroglobulin measurement results of cervical nodal metastasis in patients with unclear papillary thyroid carcinoma[J]. Front Endocrinol (Lausanne), 2019, 10: 395. DOI:10.3389/fendo.2019.00395 |
| [17] |
LIU QH, MAO L, ZHANG ZW, et al. Diagnostic efficacy of FNA-Tg in DTC cervical LN metastasis and its impact factors: a large retrospective study[J]. J Clin Endocrinol Metab, 2023, 108(12): 3311-3319. DOI:10.1210/clinem/dgad335 |
| [18] |
WANG YX, DUAN YS, ZHOU MQ, et al. The diagnostic value of thyroglobulin in fine-needle aspiration of metastatic lymph nodes in patients with papillary thyroid cancer and its influential factors[J]. Surg Oncol, 2021, 39: 101666. DOI:10.1016/j.suronc.2021.101666 |
| [19] |
曹亚, 张辉, 孟林, 等. 彩色超声、FNA-C、FNA-Tg在诊断甲状腺乳头状癌(PTC) 颈部淋巴结转移中的价值[J]. 昆明医科大学学报, 2021, 42(11): 105-110. DOI:10.12259/j.issn.2095-610X.S20211119 |
| [20] |
WANG J, JIANG X, XIAO G, et al. Excellent diagnostic performance of FNA-Tg in detecting lymph nodes metastases from papi- llary thyroid cancer[J]. Future Oncol, 2020, 16(33): 2735-2746. DOI:10.2217/fon-2020-0213 |
| [21] |
HAUGEN BR, ALEXANDER EK, BIBLE KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer[J]. Thyroid, 2016, 26(1): 1-133. DOI:10.1089/thy.2015.0020 |
| [22] |
ZHAO HQ, LI HH. Meta-analysis of ultrasound for cervical lymph nodes in papillary thyroid cancer: diagnosis of central and lateral compartment nodal metastases[J]. Eur J Radiol, 2019, 112: 14-21. DOI:10.1016/j.ejrad.2019.01.006 |
 2024, Vol. 53
2024, Vol. 53




