文章信息
- 礼仕可, 施文瑜, 张卓, 张锋, 孙秀华
- LI Shike, SHI Wenyu, ZHANG Zhuo, ZHANG Feng, SUN Xiuhua
- 原发性睾丸弥漫大B细胞淋巴瘤的临床特征与预后分析
- Clinical characteristics and prognosis of primary testicular diffuse large B-cell lymphoma
- 中国医科大学学报, 2023, 52(12): 1074-1081
- Journal of China Medical University, 2023, 52(12): 1074-1081
-
文章历史
- 收稿日期:2023-07-09
- 网络出版时间:2023-12-06 16:54:04
2. 南通大学附属医院肿瘤科,江苏 南通 226001;
3. 大连医科大学附属第二医院肿瘤科,辽宁 大连 116027
2. Department of Oncology, Affiliated Hospital of Nantong University, Nantong 226001, China;
3. Department of Oncology, The Second Affiliated Hospital of Dalian Medical University, Dalian 116027, China
近年来,淋巴瘤的发病率逐年上升。我国癌症统计数据[1]显示2016年新发淋巴瘤病例9万,高于2015年(新发病例8.82万) [2],死亡人数达5万/年。原发性睾丸淋巴瘤(primary testicular lymphoma,PTL) 是一种罕见的非霍奇金淋巴瘤(non-Hodgkin lymphoma,NHL),年发病率约0.26/100 000[3],占所有恶性淋巴瘤的1%~2%,占所有原发性睾丸实性恶性肿瘤的1%~9%[4-5]。弥漫大B细胞淋巴瘤(diffuse large B-cell lymphoma,DLBCL) 是PTL最常见的病理类型,约占80%~90%[6]。本研究收集近3年2所医院PT-DLBCL患者的临床资料,分析PT-DLBCL患者的临床特征及预后情况,同时采用Kaplan-Meier单因素及多因素Cox回归分析各临床指标对患者预后的影响,旨在为PT-DLBCL标准治疗提供依据。
1 材料与方法 1.1 临床资料收集南通大学附属医院及大连医科大学附属第二医院2000年1月1日至2022年12月31日期间诊治的PT-DLBCL患者的临床资料。纳入标准:(1) 临床诊断为PTL,经穿刺或手术病理证实为DLBCL;(2) 年龄≥18岁。排除标准:(1) 有HIV和(或) EBV感染和(或) 合并其他严重基础疾病;(2) 继发性睾丸淋巴瘤;(3) 既往恶性肿瘤病史和(或) 同时合并其他恶性肿瘤。本研究已获得医院伦理委员会批准(2022042.115)。
1.2 数据收集所有病例均随访至患者死亡或2023年5月31日,随访数据来源于住院病例档案及电话随访。
收集患者临床相关资料,记录一般临床特征[年龄、首发临床表现、体质量指数(body mass index,BMI)、肿瘤部位、肿瘤大小以及有无并发症],病理及免疫组织化学指标[肿瘤细胞来源(Hans分型标准),生发中心型(germinal center B,GCB) 及非生发中心型(non-germinal center B,non-GCB),CD10、CD20、CD30、CD117、CD3、BCL-2、BCL-6、MUM-1、Ki-67及PLAP],美国东部肿瘤协作组(eastern cooperative oncology group,ECOG) 评分,国际预后指数(international prognostic index,IPI) 评分,Ann Arbor分期,治疗方案[有无手术、化疗、放疗及中枢神经系统(central nervous system,CNS) 预防性治疗,是否联合应用蒽环类药物(anthracyclines,ANT)、是否联合应用利妥昔单抗(rituximab,R)],初治反应[完全缓解(complete remission,CR)、部分缓解(partial remission,PR)、稳定状态(stable disease,SD)、持续进展(progressive disease,PD)],复发部位和时间,最终生存状态。
1.3 统计学分析采用SPSS 27.0软件进行统计分析。计数资料采用率(%) 表示,计量资料采用M (P25~P75) 表示。采用Kaplan-Meier单因素分析方法评估影响总生存期(overall survival,OS) 的影响因素(排除了部分实验室指标或治疗方案缺失的患者),使用log-rank检验评估生存差异。采用Cox比例风险模型比较患者的生存时间。P < 0.05为差异有统计学意义。
2 结果 2.1 PT-DLBCL患者的临床特征、病理及免疫组织化学指标共纳入47例,患者年龄64 (53~74) 岁,BMI 24.5 (22.4~25.8) kg/m2,肿瘤直径5.2 (4.1~6.2) cm。具体临床特征及免疫组织化学结果见表 1、2。
| Item | n | Percentage (%) |
| B symptoms | ||
| Absent | 44 | 93.6 |
| Present | 2 | 4.3 |
| Unknown | 1 | 2.1 |
| Laterality | ||
| Left | 23 | 48.9 |
| Right | 23 | 48.9 |
| Bilateral | 1 | 2.1 |
| First symptom | ||
| Testicular swelling | 40 | 85.2 |
| Testicular mass | 4 | 8.5 |
| Orchialgia | 1 | 2.1 |
| Testis reduction | 1 | 2.1 |
| Others | 1 | 2.1 |
| ECOG | ||
| 0-2 | 36 | 76.6 |
| ≥3 | 7 | 14.9 |
| Unknown | 4 | 8.5 |
| IPI | ||
| 0-3 | 35 | 74.4 |
| 4-5 | 8 | 17.1 |
| Unknown | 4 | 8.5 |
| Ann Arbor stage | ||
| Ⅰ-Ⅱ | 25 | 53.4 |
| Ⅲ-Ⅳ | 18 | 38.1 |
| Unknown | 4 | 8.5 |
| Item | n | Percentage (%) |
| Classification | ||
| GCB | 7 | 14.9 |
| Non-GCB | 40 | 85.1 |
| CD10 | ||
| + | 6 | 13.6 |
| - | 38 | 86.4 |
| Bcl-6 | ||
| + | 27 | 60 |
| - | 18 | 40 |
| Mum-1 | ||
| + | 40 | 87 |
| - | 6 | 13 |
| Bcl-2 | ||
| + | 44 | 100 |
| - | 0 | 0 |
| Ki-67 | ||
| > 80% | 19 | 40.4 |
| ≤80% | 28 | 59.6 |
| CD30 | ||
| + | 6 | 13.6 |
| - | 38 | 86.4 |
| PLAP | ||
| + | 0 | 0 |
| - | 47 | 100 |
2.2 治疗方法及结局
47例PT-DLBCL患者的具体治疗方案及结局如表 3所示。其中38例(80.9%) 行睾丸切除术,8例(17%) 未手术,1例(2.1%) 手术不详;36例(76.6%) 患者行全身化疗,7例(14.9%) 未化疗,4例(8.5%) 化疗不详;化疗方案主要为CHOP或R-CHOP方案,中位化疗周期为6个周期(1~8个周期);12例(25.5%) 患者接受放疗,28例(59.6%) 接受CNS预防性治疗。参照Lugano2014疗效评价[7]进行首次评估,29例CR,3例PR,3例SD,4例PD,8例未评估,疾病控制率(disease control rate,DCR) 为89.7%。
| No. | Stage | Surgery | Further therapy | Chemotherapy cycle | Response | Site and time of relapse | Overall survival (month) |
| 1 | Ⅰ | Yes | CHOP+RT+ITC | 2 | CR | Lymph nodes throughout the body,lungs (55 months) | 55 |
| 2 | Ⅳ | Yes | No | PD | Lymph nodes throughout the body,CNS (4 months) | 4 | |
| 3 | Ⅳ | No | ZR-MTX+ITC | 1 | PD | No relapse | 3 |
| 4 | Ⅰ | Yes | CHOP/B-CHOP | 6 | CR | Left leg (36 months) | 230 |
| 5 | Ⅰ | Yes | R-CHOP+ITC+Intravenous inject R-MTX | 4 | CR | No relapse | 4 |
| 6 | Ⅰ | Yes | No | PD | Lymph nodes throughout the body,lungs (3 months) | 3 | |
| 7 | Ⅰ | No | R-CHOP+ITC | 6 | CR | 23 | |
| 8 | Ⅳ | No | R-COP/R-CHOP | 7 | PD | Bladder,retroperitoneal lymph nodes (1 month) | 16 |
| 9 | Ⅱ | No | R-CHOP+ITC+Autologous stem cell transplantation | 6 | CR | No relapse | 27 |
| 10 | Ⅱ | No | R-CHOP | 5 | CR | No relapse | 12 |
| 11 | Ⅰ | No | R-CHOP+ITC | 7 | CR | No relapse | 10 |
| 12 | Ⅱ | No | CHOP/R-CHOP+ITC | 6 | CR | No relapse | 31 |
| 13 | Unknown | No | Unknown | Loss | |||
| 14 | Ⅰ | Yes | R-CHOP-MTX+RT+ITC | 3 | CR | No relapse | 13 |
| 15 | Ⅰ | Yes | R-CHOP+ITC | 5 | PR | Contralateral testis,right inguinal lymph node,left thigh (4 months) | 41 |
| 16 | Ⅰ | Yes | No | CR | No relapse | 70 | |
| 17 | Ⅰ | Yes | R-CHOP | 6 | CR | No relapse | 48 |
| 18 | Ⅰ | Yes | R-CHOP+ITC | 4 | CR | No relapse | 11 |
| 19 | Ⅰ | Yes | R-CHOP+RT+ITC | 8 | PR | Contralateral testis (5 months) | 62 |
| 20 | Ⅳ | Yes | R-CHOP | 2 | PR | Contralateral testis (1 month) | 26 |
| 21 | Ⅳ | Yes | R-CHOP+ITC | 7 | CR | No relapse | 12 |
| 22 | Ⅳ | Yes | R-CHOP+ITC | 8 | CR | CNS (12 months) | 14 |
| 23 | Ⅰ | Yes | R-CHOP+ITC | 6 | CR | No relapse | 40 |
| 24 | Ⅰ | Yes | No | CR | No relapse | 12 | |
| 25 | Ⅳ | Yes | R-CHOP+ITC | 7 | CR | No relapse | 11 |
| 26 | Ⅰ | Yes | R-CHOP+ITC+Intravenous inject R-MTX | 6 | CR | Contralateral testis (6 months) | 60 |
| 27 | Unknown | Unknown | Unknown | Loss | |||
| 28 | Ⅰ | Yes | R-CHOP+RT+ITC+Intravenous inject R-MTX | 6 | CR | No relapse | 37 |
| 29 | Ⅳ | Yes | R-CHOP+ITC+Intravenous inject R-MTX | 6 | CR | No relapse | 12 |
| 30 | Ⅰ | Yes | R-CHOP+ITC+Intravenous inject R-MTX | 6 | CR | No relapse | 11 |
| 31 | Ⅲ | Yes | R-CHOP+RT+ITC | 6 | CR | No relapse | 11 |
| 32 | Ⅲ | Yes | R-CHOP+RT+ITC | 6 | CR | No relapse | 30 |
| 33 | Ⅰ | Yes | CHOP+RT+ITC | 3 | SD | Contralateral testis (90 months) | 168 |
| 34 | Ⅱ | Yes | R-CHOP+RT+ITC | 8 | CR | No relapse | 61 |
| 35 | Ⅲ | Yes | R-GemOx+ITC | 6 | SD | No relapse | 14 |
| 36 | Ⅰ | Yes | RT | Loss | |||
| 37 | Ⅲ | Yes | CHOP+RT+ITC | 6 | SD | CNS (8 months) | 12 |
| 38 | Ⅲ | Yes | CHOP+RT | 1 | Loss | ||
| 39 | Ⅲ | Yes | R-CHOP+ITC | 3 | CR | No relapse | 110 |
| 40 | Unknown | Yes | No | Loss | |||
| 41 | Ⅲ | Yes | R-CHOP/CHOP+ITC | 4 | CR | No relapse | 127 |
| 42 | Ⅰ | Yes | No | Loss | |||
| 43 | Ⅰ | Yes | CHOP | 4 | CR | CNS (48 months) | 48 |
| 44 | Ⅳ | Yes | No | Loss | |||
| 45 | Ⅲ | Yes | R-CHOP | 6 | CR | No relapse | 24 |
| 46 | Ⅲ | Yes | R-CHOP | 5 | CR | No relapse | 120 |
| 47 | Unknown | Yes | No | Loss | |||
| Loss,loss to follow-up. | |||||||
2.3 患者随访
本研究中位随访时间为24个月(3~230个月),47例中8例患者失访,失访率14.7% (4/47)。随访时间内14例复发,复发率为35.9% (14/39);常见复发部位为对侧睾丸及CNS。
2.4 影响预后相关因素分析将一般临床特征、ECOG评分、IPI评分及Ann Arbor分期、实验室指标、免疫组织化学及治疗及疗效等相关指标进行Kaplan-Meier单因素分析,结果显示年龄≥70岁、ECOG评分≥3分、手术、LDH水平升高、Mon水平升高、未联合应用ANT、未联合应用R、单一治疗方式、初治反应无效及复发与PT-DLBCL患者不良预后相关(均P < 0.05),而Ann Arbor分期、肿瘤大小、有无合并B症状、IPI评分≥4分、化疗、化疗周期、放疗及CNS预防性治疗均与患者预后不相关(均P > 0.05),见表 4。
| Item | n | OS (month) | Progression-free-survival (%) | P | ||
| 1 year | 3 years | 5 years | ||||
| Age | 0.001 | |||||
| < 70 years | 28 | 52.3 | 89.0 | 89.0 | 73.4 | |
| ≥70 years | 11 | 14.4 | 75.8 | 25.3 | 0 | |
| Lump size | 0.228 | |||||
| ≤5.2 cm | 20 | 50.3 | 95.0 | 78.9 | 69.1 | |
| > 5.2 cm | 18 | 34.1 | 79.9 | 71.0 | 47.4 | |
| B symptoms | 0.775 | |||||
| Yes | 1 | - | - | - | - | |
| No | 38 | - | 86.0 | 77.7 | 59.2 | |
| Subtype | 0.138 | |||||
| GCB | 6 | - | 100.0 | 100.0 | 100.0 | |
| Non-GCB | 33 | - | 83.3 | 73.5 | 52.6 | |
| CD30 | 0.497 | |||||
| Positive | 5 | 29.0 | 75.0 | 75.0 | 75.0 | |
| Negative | 31 | 45.8 | 86.6 | 76.9 | 55.9 | |
| Bcl-6 | 0.681 | |||||
| Positive | 25 | 39.6 | 95.0 | 80.9 | 61.6 | |
| Negative | 13 | 43.8 | 69.2 | 69.2 | 51.9 | |
| Mum-1 | 0.968 | |||||
| Positive | 35 | 42.5 | 84.4 | 75.5 | 61.0 | |
| Negative | 4 | 34.0 | 100.0 | 100.0 | 50.0 | |
| CD10 | 0.150 | |||||
| Positive | 5 | - | 100.0 | 100.0 | 100.0 | |
| Negative | 32 | - | 83.1 | 72.6 | 52.0 | |
| ECOG score | 0.039 | |||||
| 0-2 | 34 | 45.7 | 90.5 | 90.5 | 68.9 | |
| ≥3 | 5 | 13.8 | 60.0 | - | - | |
| IPI score | 0.087 | |||||
| 0-3 | 33 | 46.1 | 90.2 | 90.2 | 68.7 | |
| 4-5 | 6 | 17.0 | 66.7 | - | - | |
| Ann Arbor stage | 0.302 | |||||
| Ⅰ-Ⅱ | 23 | 46.8 | 90.3 | 90.3 | 61.9 | |
| Ⅲ-Ⅳ | 16 | 34.1 | 80.2 | 55.0 | 55.0 | |
| LDH | 0.018 | |||||
| Normal | 25 | 50.8 | 95.0 | 87.7 | 69.1 | |
| Abnormal | 14 | 25.2 | 70.7 | 60.6 | 40.4 | |
| Mon | 0.005 | |||||
| Normal | 28 | 51.9 | 92.0 | 86.6 | 71.5 | |
| Abnormal | 11 | 15.5 | 71.6 | 47.7 | 0 | |
| Surgery | 0.039 | |||||
| Yes | 32 | 46.9 | 86.3 | 81.2 | 61.8 | |
| No | 7 | 17.4 | 85.7 | - | - | |
| Chemotherapy | 0.986 | |||||
| Yes | 35 | 43.8 | 93.7 | 84.3 | 62.4 | |
| No | 2 | 37.0 | 50.0 | 50.0 | 50.0 | |
| Cycles | 0.344 | |||||
| < 6 | 13 | 56.8 | 92.3 | 80.8 | 46.2 | |
| ≥6 | 22 | 36.2 | 94.4 | 87.2 | 87.2 | |
| Radiotherapy | 0.862 | |||||
| Yes | 10 | 45.3 | 85.7 | 85.7 | 65.6 | |
| No | 26 | 44.0 | 92.3 | 79.9 | 62.1 | |
| CNS prevention | 0.944 | |||||
| Yes | 28 | 44.3 | 91.8 | 91.8 | 71.4 | |
| No | 8 | 40.0 | 87.5 | 54.7 | 36.5 | |
| Anthracyclines | 0.007 | |||||
| Yes | 33 | 46.0 | 96.3 | 86.6 | 62.4 | |
| No | 6 | 17.7 | 33.3 | 33.3 | 33.3 | |
| Rituximab | 0.025 | |||||
| Yes | 30 | 66.9 | 96.7 | 84.5 | 73.9 | |
| No | 9 | 34.0 | 55.6 | 55.6 | 33.3 | |
| Multimodal therapy | 0.015 | |||||
| Yes | 33 | 45.6 | 93.2 | 80.7 | 62.5 | |
| No | 6 | 19.5 | 50.0 | 25.0 | 25.0 | |
| Initial treatment effect | 0.001 | |||||
| Effective | 35 | 45.6 | 93.1 | 88.2 | 67.2 | |
| Ineffective | 4 | 6.5 | 25.0 | 0 | 0 | |
| Relapse | 0.023 | |||||
| Yes | 14 | 35.2 | 71.4 | 47.6 | 31.7 | |
| No | 25 | 53.0 | 94.7 | 94.7 | 94.7 | |
| Relapse time | 0.166 | |||||
| ≤6 months | 8 | 26.9 | 62.5 | 37.5 | 25.0 | |
| > 6 months | 6 | 87.8 | 83.3 | 83.3 | 41.7 | |
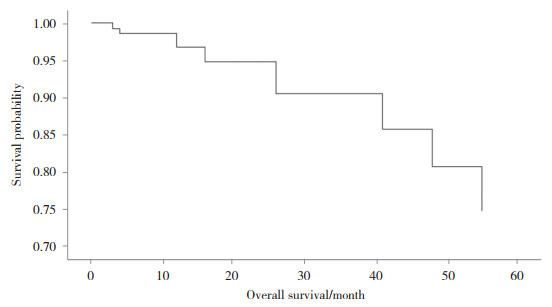
将单因素分析有统计学意义(P < 0.05) 指标纳入Cox回归模型中,结果显示ECOG评分≥3分、未联合应用R及初治反应无效是患者预后不良的独立危险因素(均P < 0.05)。见表 5。PT-DLBCL患者中位生存时间为41.6个月,1年、3年及5年生存率分别为93%、77%、59%。见图 1。
| Variable | B | SE | Wald | P | HR | 95%CI |
| ECOG score | -2.245 | 1.029 | 4.757 | 0.029 | 0.106 | 0.014-0.797 |
| Rituximab | 2.294 | 0.935 | 6.019 | 0.014 | 9.919 | 1.586-62.012 |
| Initial treatment effect | -3.025 | 0.998 | 9.179 | 0.002 | 0.049 | 0.007-0.344 |
|
| 图 1 PT-DLBCL患者的Cox回归生存分析 Fig.1 Survival analysis of PT-DLBCL patients by Cox regression analysis |
3 讨论
PTL是60岁以上男性最常见的睾丸恶性肿瘤,80%~90%病理类型为DLBCL,大部分为non-GCB型[6]。有研究[3, 8-11]发现PT-DLBCL的中位发病年龄为66~70岁,单侧无痛性睾丸肿胀是最常见的临床症状,可持续数周至数月,甚至数年,少数伴有剧痛,绝大多数不合并B症状。XU等[12]对1 169例PTL患者的回顾性研究表明确诊年龄是预后的重要影响因素,年龄 > 70岁患者预后更差,与本研究结果一致。一项包含1 581例PTL患者的回顾性研究[13]证实年龄越小,预后越好。因此,临床上遇到因无痛性睾丸肿块就诊的老年男性时,要注意鉴别PTL。
尽管PT-DLBCL的表现是无害的,但它的临床病程具有侵袭性,且倾向于在免疫隔离部位(睾丸和CNS) 生长及复发。研究[9]显示,患者也多复发于对侧睾丸及CNS,且与预后不良显著相关;分析原因主要是由于特定的界面屏障(血-睾屏障或血-脑屏障) 的保护,使恶性肿瘤细胞在特定部位内形成一种特殊的免疫微环境,这些区域不在免疫系统的作用范围内;其次,也可能与NF-κB通路信号传导异常、染色体畸变和肿瘤浸润免疫细胞有关。因此,PT-DLBCL容易复发且OS较短,其复发甚至可以在最初治疗的15年后[14]。
WANG等[15] 1项39例PTL患者的回顾性研究发现,ECOG评分≥2分、邻近组织肿瘤浸润和巨大的肿瘤直径(> 9 cm) 是影响预后的因素。CHEAH等[16]研究发现年龄 > 70岁、Ann Arbor Ⅲ~Ⅳ期、合并B症状、ECOG评分 > 1分、多结外部位浸润、巨大肿块直径(> 10 cm)、高LDH及β2-MG水平、低白蛋白血症及肿瘤位于左侧睾丸是PTL患者预后的不良因素;王昀哲等[17]在63例PTL患者的回顾性研究中也得出了类似结论。此外,徐鸣睿[18]还发现未接受CNS预防性治疗也是PTL患者预后不良的影响因素;通过多因素Cox回归分析发现,进展期(Ann Arbor Ⅲ~Ⅳ期)、肿瘤直径≥7 cm、IPI评分≥2分、高β2-MG水平是PTL患者预后不良的独立危险因素。本研究共纳入47例PT-DLBCL患者,8例失访,失访率14.7%,与学术界认可的失访率(20%) 接近[7],数据可信。本研究单因素分析结果表明年龄≥70岁、ECOG评分≥3分、IPI评分≥4分、高LDH及Mon水平、未联合应用ANT、未联合应用R、单一治疗方式、初治反应无效及复发是PT-DLBCL患者预后不良的影响因素;多因素Cox回归分析显示ECOG评分≥3分、未联合应用R及初治反应无效是PT-DLBCL预后不良的独立危险因素。而Ann Arbor分期、未接受CNS预防、化疗周期及病理分型等与患者OS不相关。此外,多项研究[18-21]表明PT-DLBCL患者OS与病理亚型有关,GCB型比non-GCB型的PT-DLBCL患者有更好的OS,但本研究中两者比较无统计学差异,可能是样本量较少、患者治疗方案不同以及随访时间较短所致。未来需大样本、前瞻性的研究来进一步论证。
PT-DLBCL发病率低,缺乏病例及大型前瞻性试验,目前文献多为回顾性研究,尚无标准化治疗指南。公认的治疗方案包括患侧睾丸切除、化疗、放疗及CNS预防性治疗联合[8, 16],本研究患者整体1年、3年及5年OS分别为86.2%,77.9%,59.3%,联合治疗患者1年、3年、5年OS分别为93.2%,80.7%,62.5%,高于单一治疗模式(OS分别为50.0%、25.0%、25.0%),且联合治疗OS与Ⅱ期临床试验结果一致[22-23]。1项373例PT-DLBCL患者的回顾性研究[4]发现,良好的IPI评分、无B症状、使用ANT和预防性阴囊放疗与较长的OS显著相关;含ANT的化疗方案、CNS预防性治疗和对侧睾丸放疗似乎可以改善预后。一系列回顾性研究和1项IELSG10前瞻性Ⅱ期试验提示加入R联合化疗可增加疗效,改善PT-DLBCL患者预后[10, 22, 24-26],但也有部分研究[5, 27]未发现R化疗可以提高预后。本研究结果显示,联合应用ANT、R可显著改善PT-DLBCL患者预后,多因素Cox模型分析结果显示联合应用R是OS的独立影响因素。有研究[4, 8-9, 13]证实放疗及CNS预防性治疗可降低复发风险,提高生存率;但本研究未发现放疗、CNS预防性治疗与OS的相关性,可能是样本量较少且随访时间较短所致,后续研究需增大样本量,延长随访时间。
综上所述,PT-DLBCL罕见且预后差,尽早诊断且联合应用ANT、R可能改善患者预后。本研究收集2家医院的临床数据,较全面反映了PT-DLBCL患者的临床特征。另外,本研究全面分析了PT-DLBCL的临床特征、病理特征及实验室指标与预后的关系,为以后大样本、前瞻性队列研究奠定了基础。本研究属于回顾性研究,且样本量较少,存在偏倚,后续需要纳入更多所医院,收集更多PT-DLBCL患者的资料来进一步论证。
| [1] |
郑荣寿, 张思维, 孙可欣, 等. 2016年中国恶性肿瘤流行情况分析[J]. 中华肿瘤杂志, 2023, 45(3): 212-220. DOI:10.3760/cma.j.cn112152-20220922-00647 |
| [2] |
CHEN WQ, ZHENG RS, BAADE PD, et al. Cancer statistics in China, 2015[J]. CA A Cancer J Clin, 2016, 66(2): 115-132. DOI:10.3322/caac.21338 |
| [3] |
AHMAD SS, IDRIS SF, FOLLOWS GA, et al. Primary testicular lymphoma[J]. Clin Oncol Royal Coll Radiol G B, 2012, 24(5): 358-365. DOI:10.1016/j.clon.2012.02.005 |
| [4] |
ZUCCA E, CONCONI A, MUGHAL TI, et al. Patterns of outcome and prognostic factors in primary large-cell lymphoma of the testis in a survey by the International Extranodal Lymphoma Study Group[J]. J Clin Oncol, 2003, 21(1): 20-27. DOI:10.1200/JCO.2003.11.141 |
| [5] |
GUNDRUM JD, MATHIASON MA, MOORE DB, et al. Primary testicular diffuse large B-cell lymphoma: a population-based study on the incidence, natural history, and survival comparison with primary nodal counterpart before and after the introduction of rituximab[J]. J Clin Oncol, 2009, 27(31): 5227-5232. DOI:10.1200/jco.2009.22.5896 |
| [6] |
MENTER T, ERNST M, DRACHNERIS J, et al. Phenotype profiling of primary testicular diffuse large B-cell lymphomas[J]. Hematol Oncol, 2014, 32(2): 72-81. DOI:10.1002/hon.2090 |
| [7] |
CHESON BD, FISHER RI, BARRINGTON SF, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification[J]. J Clin Oncol, 2014, 32(27): 3059-3068. DOI:10.1200/JCO.2013.54.8800 |
| [8] |
CHEN B, CAO DH, LAI L, et al. Adult primary testicular lymphoma: clinical features and survival in a series of patients treated at a high-volume institution in China[J]. BMC Cancer, 2020, 20(1): 1-11. DOI:10.1186/s12885-020-6711-0 |
| [9] |
POLLARI M, LEIVONEN SK, LEPPÄ S. Testicular diffuse large B-cell lymphoma—clinical, molecular, and immunological features[J]. Cancers, 2021, 13(16): 4049. DOI:10.3390/cancers13164049 |
| [10] |
KRIDEL R, TELIO D, VILLA D, et al. Diffuse large B-cell lymphoma with testicular involvement: outcome and risk of CNS relapse in the rituximab era[J]. Br J Haematol, 2017, 176(2): 210-221. DOI:10.1111/bjh.14392 |
| [11] |
廖冶丹, 余顺玲, 周永红, 等. 52例原发性睾丸淋巴瘤的临床分析[J]. 昆明医科大学学报, 2019, 40(5): 42-48. DOI:10.3969/j.issn.1003-4706.2019.05.008 |
| [12] |
XU HT, YAO FS. Primary testicular lymphoma: a SEER analysis of 1, 169 cases[J]. Oncol Lett, 2019, 3(Pt.B): 17. DOI:10.3892/ol.2019.9953 |
| [13] |
BERJAOUI MB, HERRERA-CACERES JO, LI TG, et al. Age related differences in primary testicular lymphoma: a population based cohort study[J]. Urol Oncol Semin Orig Investig, 2023, 41(3): 151.e1-151.e10. DOI:10.1016/j.urolonc.2022.10.032 |
| [14] |
LAGMAY J, TERMUHLEN A, FUNG B, et al. Primary testicular presentation of ALK-1-negative anaplastic large cell lymphoma in a pediatric patient[J]. J Pediatr Hematol, 2009, 31(5): 330-332. DOI:10.1097/mph.0b013e3181979c5e |
| [15] |
WANG Y, LI ZM, HUANG JJ, et al. Three prognostic factors influence clinical outcomes of primary testicular lymphoma[J]. Tumor Biol, 2013, 34(1): 55-63. DOI:10.1007/s13277-012-0510-4 |
| [16] |
CHEAH CY, WIRTH A, SEYMOUR JF. Primary testicular lymphoma[J]. Blood, 2014, 123(4): 486-493. DOI:10.1182/blood-2013-10-530659 |
| [17] |
王昀哲. 原发性睾丸淋巴瘤的临床特征及预后因素分析[D]. 石家庄: 河北医科大学, 2022.
|
| [18] |
徐鸣睿. 原发性睾丸弥漫大B细胞淋巴瘤的免疫表型对患者预后的影响[D]. 大连: 大连医科大学, 2020.
|
| [19] |
KING RL, GOODLAD JR, CALAMINICI M, et al. Lymphomas arising in immune-privileged sites: insights into biology, diagnosis, and pathogenesis[J]. Virchows Arch, 2020, 476(5): 647-665. DOI:10.1007/s00428-019-02698-3 |
| [20] |
YAN Z, YAO SN, WANG YY, et al. Primary testicular lymphoma with central nervous system relapse was successfully treated by a chemo-free regimen: a case report and literature review[J]. Cancer Manag Res, 2021, 13: 9489-9500. DOI:10.2147/cmar.s341342 |
| [21] |
苗雨青, 徐浩, 李建勇. 原发性睾丸淋巴瘤的研究进展[J]. 白血病·淋巴瘤, 2018, 27(8): 509-512. DOI:10.3760/cma.j.issn.1009-9921.2018.08.017 |
| [22] |
VITOLO U, CHIAPPELLA A, FERRERI AJM, et al. First-line treatment for primary testicular diffuse large B-cell lymphoma with rituxi-mab-CHOP, CNS prophylaxis, and contralateral testis irradiation: final results of an international phaseⅡtrial[J]. J Clin Oncol, 2011, 29(20): 2766-2772. DOI:10.1200/JCO.2010.31.4187 |
| [23] |
AVILÉS A, NAMBO MJ, CLETO S, et al. Rituximab and dose-dense chemotherapy in primary testicular lymphoma[J]. Clin Lymphoma Myeloma, 2009, 9(5): 386-389. DOI:10.3816/clm.2009.n.075 |
| [24] |
MAZLOOM A, FOWLER N, MEDEIROS LJ, et al. Outcome of patients with diffuse large B-cell lymphoma of the testis by era of treatment: the M. D. Anderson Cancer Center experience[J]. Leuk Lymphoma, 2010, 51(7): 1217-1224. DOI:10.3109/10428191003793358 |
| [25] |
DENG L, XU-MONETTE ZY, LOGHAVI S, et al. Primary testicular diffuse large B-cell lymphoma displays distinct clinical and biological features for treatment failure in rituximab era: a report from the International PTL Consortium[J]. Leukemia, 2016, 30(2): 361-372. DOI:10.1038/leu.2015.237 |
| [26] |
SHIMADA K, YAMAGUCHI M, ATSUTA Y, et al. Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone combined with high-dose methotrexate plus intrathecal chemotherapy for newly diagnosed intravascular large B-cell lymphoma (PRIMEUR-IVL): a multicentre, single-arm, phase 2 trial[J]. Lancet Oncol, 2020, 21(4): 593-602. DOI:10.1016/S1470-2045(20)30059-0 |
| [27] |
廖冶丹. 原发性睾丸淋巴瘤临床、病理特点及预后分析[D]. 昆明: 昆明医科大学, 2018.
|
 2023, Vol. 52
2023, Vol. 52




