文章信息
- 富维强, 刘永馥, 何旖旎
- FU Weiqiang, LIU Yongfu, HE Yini
- 超声极速成像技术在单纯夜间高血压患者颈动脉脉搏波传导速度评价中的应用
- The evaluation of carotid pulse wave velocity with ultrafast ultrasound imaging in patients with isolated nocturnal hypertension
- 中国医科大学学报, 2023, 52(1): 68-72
- Journal of China Medical University, 2023, 52(1): 68-72
-
文章历史
- 收稿日期:2022-03-11
- 网络出版时间:2023-01-18 09:11:08
2. 中国医科大学附属第一医院心血管内科, 沈阳 110001;
3. 中国医科大学附属第一医院全科医学, 沈阳 110001
2. Department of Cardiology, The First Hospital of China Medical University, Shenyang 110001, China;
3. Department of General Practice, The First Hospital of China Medical University, Shenyang 110001, China
夜间高血压(nocturnal hypertension,NH)指夜间平均收缩压≥120 mmHg或舒张压≥70 mmHg,并且白天平均收缩压 < 135 mmHg和舒张压 < 85 mmHg[1]。研究[1]显示,单纯NH占高血压人群的10.9%。由于单纯NH患者仅表现为夜间血压升高,因而临床上常常被忽视。已有研究[2-4]表明,单纯NH患者不良心血管事件的发生率比正常人群明显增高,靶器官损害程度与全天高血压相近。因此,准确检测出NH患者靶器官的损害程度,对指导临床进行早期干预意义重大。
研究[2-4]发现,高血压及血压昼夜节律异常改变可导致动脉粥样硬化斑块形成,动脉粥样硬化斑块一旦形成就很难逆转。极速超声成像(ultrafast ultrasound imaging,UFI)是近年发展起来的新技术,它可通过检测颈动脉脉搏波传导速度(pulse wave velocity,PWV)来评价动脉硬度[5],能够更加早期地监测血管的结构或功能。本研究旨采用UFI技术检测NH患者颈动脉PWV,旨在为临床早期评价NH患者动脉硬度,及时制定治疗方案及评估疗效提供参考依据。
1 材料与方法 1.1 临床资料及分组收集2017年2月至2020年10月因可疑高血压或诊室高血压于我院进行高血压筛查或血压昼夜节律评估的患者的临床资料。纳入标准:临床诊断分别为血压正常、单纯NH和全天高血压的患者。排除标准:(1)继发高血压、糖尿病、高脂血症;(2)颈动脉斑块;(3)心律失常;(4)结构性心脏病,如心力衰竭、心肌梗死、心脏瓣膜病、先天性心脏病、心肌病、心包病变等;(5)缺血或出血性脑血管病病史;(6)慢性阻塞性肺疾病、慢性肺源性心脏病;(7)肝肾功能不全;(8)患有其他疾病,如肿瘤、自身免疫性疾病、甲状腺功能异常等;(9)进行糖皮质激素或激素治疗,有药物或酒精滥用史,妊娠,颈动脉超声图像质量欠佳等。本研究已获得中国医科大学附属第一医院伦理委员会批准,所有患者均知情同意并签署知情同意书。
共纳入182例,按照血压状况[6]分为血压正常组(白天平均血压 < 135/85 mmHg,且夜间平均血压 < 120/70 mmHg,n = 75)、单纯NH组(白天平均血压 < 135/85 mmHg,且夜间平均血压≥120/70 mmHg,n = 31)、全天高血压组(白天平均血压≥135/85 mmHg,且夜间平均血压≥120/70 mmHg,n = 76)。3组性别、体质量指数(body mass index,BMI)比较无统计学差异(均P > 0.05)。与正常血压组比较,单纯NH组和全天高血压组年龄、低密度脂蛋白胆固醇、甘油三酯及空腹血糖均显著增加(均P < 0.05);而单纯NH组和全天高血压组各项指标比较均无统计学差异(均P > 0.05),见表 1。
| Item | Normotensive group (n = 75) |
Isolated nocturnal hypertension group (n = 31) |
All-day hypertension group (n = 76) |
| Age(year) | 47.8±7.9 | 51.9±8.8 | 52.4±6.1 |
| Men [n(%)] | 36(50) | 15(49) | 45(56) |
| BMI(kg/m2) | 24.56±3.11 | 25.18±2.74 | 25.44±2.36 |
| Low density lipoprotein cholesterin(mmol/L) | 2.63±0.81 | 2.84±0.47 | 2.85±0.68 |
| High density lipoprotein cholesterol(mmol/L) | 1.46±0.33 | 1.45±0.29 | 1.47±0.34 |
| Triglyceride(mmol/L) | 1.08±0.48 | 1.21±0.53 | 1.23±0.48 |
| Total cholesterol(mmol/L) | 4.63±0.51 | 4.68±0.79 | 4.57±0.82 |
| Fasting blood glucose(mmol/L) | 5.02±1.66 | 5.48±1.52 | 5.55±1.23 |
1.2 检测方法 1.2.1 动态血压测量
采用动态血压监测仪(美国Meditech公司,ABPM05型)检测患者24 h动态血压。白天(6:00~22:00)每隔20 min测量1次,夜间(22:00~6:00)每隔30 min测量1次,总佩戴时间≥ 22 h。同时嘱咐患者严格按照设定的作息时间执行,白天避免剧烈运动。统计时舍弃可信度较差的数据(收缩压 > 260 mmHg或 < 70 mmHg,舒张压 > 150 mmHg或 < 40 mmHg,脉压 > 150 mmHg或 < 20 mmHg)后,有效测量次数应不少于总测量次数的80%。白天平均收缩压及舒张压为白天6:00~22:00所测收缩压及舒张压的平均值;24 h平均收缩压及舒张压为1 d内所测收缩压及舒张压的平均值;夜间平均收缩压及舒张压为夜间22:00~6:00所测收缩压及舒张压的平均值。
1.2.2 标准颈动脉超声检查患者取仰卧位,充分暴露颈部,采用配备有SL10-2探头,并具有血管PWV模式的声科Aixplorer超声系统(法国SuperSonic Imagine公司)进行标准颈动脉超声检查[7]。首先清晰显示颈总动脉远端的二维超声图像(距颈动脉分叉部2.0 cm),测量颈总动脉收缩末内径(diameter,D)和内-中膜厚度(intima-media thickness,IMT)。同时,采用脉冲多普勒检查测量收缩期峰值血流速度(peak systolic velocity,PSV)、舒张末期血流速度(end diastolic velocity,EDV)。
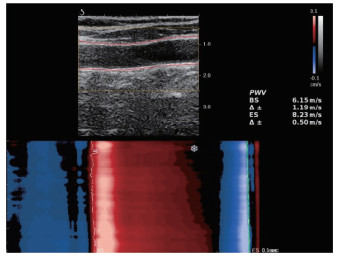
1.2.3 UFI检查调整探头平行于动脉血管壁,管壁内膜显示清晰,并避开颈内静脉。嘱患者屏气,一键自动获取图像。调整二维增益及感兴趣区域框,使追踪曲线与血管壁吻合,UFI可自动跟踪感兴趣区域内颈总动脉前壁PWV,并记录收缩起始时PWV和收缩结束时PWV,见图 1。PWV测量值误差(Δ±)≥20%时需重新测量。所有参数均测量双侧颈总动脉,分别测量3次并计算平均值。
|
| 图 1 UFI测量颈动脉前壁PWV Fig.1 Measurement of PWV at the anterior wall of the carotid artery using UFI |
1.3 重复性检验
随机选择10例受试对象,由2名医师同时测量收缩起始时PWV和收缩结束时PWV,其中1名医生间隔4周后再次测量,分别计算观察者间及观察者内的变异,评价测量重复性。计算方法为2次测量的平均值之差的绝对值/2次测量的平均值。
1.4 统计学分析采用SPSS 17.0软件进行统计分析,计量资料以x±s表示,2组比较采用独立样本t检验,3组比较采用ANOVA检验。计数资料以率(%)表示,组间比较采用χ2检验。血压与PWV的相关性采用线性回归分析。P < 0.05为差异有统计学意义。
2 结果 2.1 3组动态血压测量结果比较结果显示,单纯NH组和全天高血压组诊室收缩和舒张压均高于血压正常组(均P < 0.05),且全天高血压组高于单纯NH组(P < 0.05)。单纯NH组和全天高血压组24 h收缩压和舒张压均高于血压正常组(均P < 0.05),且全天高血压组高于单纯NH组(P < 0.05)。全天高血压组白天收缩压和舒张压均高于单纯NH组和血压正常组(均P < 0.05),而单纯NH组和血压正常组之间无统计学差异(P > 0.05)。单纯NH组和全天高血压组夜间收缩压和舒张压均高于血压正常组(P < 0.05),而单纯NH组和全天高血压组之间无统计学差异(P > 0.05),见表 2。
| Item | Normotensive group(n = 75) | Isolated NH group(n = 31) | All-day hypertension group(n = 76) |
| Office systolic pressure(mmHg) | 125.3±13.7 | 136.5±14.61) | 158.8±15.11),2) |
| Office diastolic pressure(mmHg) | 75.6±6.9 | 86.3±5.81) | 95.2±7.71),2) |
| 24 h SBP(mmHg) | 117.7±6.4 | 126.6±8.51) | 138.6±7.81),2) |
| 24 h DBP(mmHg) | 69.3±7.7 | 78.5±6.61) | 86.2±6.01),2) |
| dSBP(mmHg) | 124.3±6.2 | 128.2±7.8 | 146.4±8.21),2) |
| dDBP(mmHg) | 76.4±6.3 | 79.6±7.5 | 89.5±6.11),2) |
| nSBP(mmHg) | 109.6±8.6 | 127.8±6.41) | 130.1±7.81) |
| nDBP(mmHg) | 62.8±6.5 | 77.3±7.31) | 80.4±8.91) |
| 1)compared with the normotensive group,P < 0.05;2)compared with the isolated NH group,P < 0.05. dSBP:daytime mean systolic blood pressure;dDBP:daytime mean diastolic blood pressure;24 h SBP:24-hour mean systolic blood pressure;24 h DBP:24-hour mean diastolic blood pressure;nSBP:nocturnal mean systolic blood pressure;nDBP:nocturnal mean diastolic blood pressure. | |||
2.2 3组颈动脉超声检查结果比较
结果显示,3组颈总动脉收缩末内径、IMT、收缩起始时PWV比较差异均无统计学意义(均P > 0.05)。单纯NH组和全天高血压组PSV及EDV均高于血压正常组(P < 0.05),全天高血压组PSV及EDV高于单纯NH组(P < 0.05)。全天高血压组和单纯NH组患者收缩结束时PWV均大于血压正常组(均P < 0.05),全天高血压组患者收缩结束时PWV大于单纯NH组患者(P < 0.05),见表 3。
| Item | Normotensive group(n = 75) | Isolated NH group(n = 31) | All-day hypertension group(n = 76) |
| D(mm) | 6.30±0.60 | 6.50±0.60 | 6.50±0.70 |
| IMT(mm) | 0.58±0.21 | 0.63±0.13 | 0.66±0.19 |
| PSV(cm/s) | 70.36±15.66 | 82.05±17.851) | 90.44±16.521),2) |
| EDV(cm/s) | 23.82±6.33 | 30.48±5.471) | 34.64±6.911),2) |
| BS(m/s) | 5.74±1.32 | 5.83±1.34 | 5.72±1.65 |
| ES(m/s) | 6.63±1.99 | 7.44±2.171) | 8.14±2.081),2) |
| 1)compared with the normotensive group,P < 0.05;2)compared with the isolated NH group,P < 0.05. D,carotid internal diameter;IMT,carotid intra-medial thickness;PSV,peak systolic blood flow velocity;EDV,end-diastolic blood flow velocity;BS,pulse wave conduction velocity at the onset of systole;ES,pulse wave conduction velocity at the end of systole. | |||
2.3 全天高血压和单纯NH组血压与颈总动脉收缩结束时PWV的相关分析
结果显示,全天高血压和单纯NH患者夜间平均收缩压和平均舒张压均与颈总动脉收缩结束时PWV相关(均P < 0.001)。多元线性回归分析果显示,调整年龄、空腹血糖、低密度脂蛋白胆固醇、甘油三酯及PSV后,全天高血压和单纯NH患者夜间平均收缩压和平均舒张压均与颈总动脉收缩结束时PWV相关(均P < 0.01)。
重复性检验结果显示,颈总动脉收缩起始时、结束时PWV观察者内的差异分别为0.11和-0.06,变异系数分别为(4.80±1.44)%和(4.17±1.62)%,观察者间的差异分别为-0.08和-0.03,变异系数分别为(9.55±1.89)%和(8.34±1.16)%,说明重复性较好。
3 讨论高血压可引起心脏、脑及肾等靶器官功能损害[8]。传统的血压计只反映机体某一时间点的血压,不能反映血压的动态变化,从而导致了单纯NH被忽视而未能及时得到有效管理。动态血压监测可提供24 h血压变化,可更好反映血压波动。正常人24 h内血压节律性呈“杓型曲线”变化,即白天血压高,夜间血压低。单纯NH患者血压节律呈非杓型[9],目前认为可能的机制是与夜间自主神经功能失衡迷走神经张力减弱或交感神经作用增强、肾素-血管紧张素-醛固酮系统活性异常有关[1]。
与动态血压正常者相比,单纯NH患者的靶器官损害更严重,心血管事件的发生率更高[10-11]。因此,早期检测单纯NH患者靶器官损害具有重要的意义。PWV可无创、早期评估动脉硬度。传统PWV的方法包括肱-踝、颈-股、颈-桡测量等[12]。传统PWV的测量均依赖于PWV传播时间和两点间距离的测量,存在一定的局限性,如PWV传播时间和距离存在较大的测量误差,局部病变(动脉粥样硬化斑块或动脉瘤等)可影响PWV值,操作繁琐、不适用于肥胖患者等。
UFI技术能够以10 000帧/s以上的极高速度对图像进行采样,对局部脉搏波进行实时跟踪和捕获,并采用脉冲多普勒和彩色多普勒原理,快速记录血管壁的脉搏波传播细节,测量血管前壁收缩起始时和收缩结束时PWV。UFI测量PWV具有其独特的优势,可一键获取、省时省力、重复性高、可靠性强且不受传统PWV测量方法的限制。已有研究[5, 13]表明UFI测量PWV可准确、敏感地评价动脉硬度。本研究采用UFI技术评价单纯NH患者动脉硬度的结果显示,与血压正常组比较,单纯NH组收缩结束时颈总动脉PWV增大。与全天高血压组比较,单纯NH组收缩结束时PWV减小;且全天高血压和单纯NH患者夜间平均收缩压和平均舒张压均与收缩结束时PWV相关,提示单纯NH患者动脉硬度亦增加,临床上应密切关注和动态随访。可见,UFI是监测单纯NH患者病情变化可靠的技术手段,本研究亦显示了UFI测量PWV具有良好重复性。
以往研究[8, 14]主要针对诊室高血压或全天高血压患者的血管硬度进行评价,而忽视了血压的昼夜节律变化以及单纯NH对血管硬度的影响。本研究提示单纯夜间血压升高亦可导致血管硬度增加,因而需密切关注单纯NH患者的血压节律变化,采用UFI早期监测其动脉硬度改变,为临床早期干预提供依据。
综上所述,单纯NH患者颈总动脉收缩结束时PWV增大,UFI测量PWV可较IMT更加敏感地评价单纯NH患者早期动脉硬度,具有重要的临床价值。本研究的不足之处:(1)样本量较少,且单纯NH的发生率较全天高血压及血压正常的发生率低,3组之间样本量不匹配;(2)本研究排除了合并颈动脉硬化斑块的患者,PWV在单纯NH风险分层中是否具有增量价值尚未明确;(3)本研究未对患者随访,未明确PWV在单纯NH患者病程中的变化规律,因而尚需要多中心、大样本的数据进一步论证。
| [1] |
KARIO K. Nocturnal hypertension: new technology and evidence[J]. Hypertension, 2018, 71(6): 997-1009. DOI:10.1161/HYPERTENSIONAHA.118.10971 |
| [2] |
KARIO K, HOSHIDE S, MIZUNO H, et al. Nighttime blood pressure phenotype and cardiovascular prognosis: practitioner-based nationwide JAMP study[J]. Circulation, 2020, 142(19): 1810-1820. DOI:10.1161/CIRCULATIONAHA.120.049730 |
| [3] |
CUSPIDI C, FACCHETTI R, BOMBELLI M, et al. Nighttime blood pressure and new-onset left ventricular hypertrophy: findings from the Pamela population[J]. Hypertension, 2013, 62(1): 78-84. DOI:10.1161/HYPERTENSIONAHA.111.00682 |
| [4] |
OGEDEGBE G, SPRUILL TM, SARPONG DF, et al. Correlates of isolated nocturnal hypertension and target organ damage in a population-based cohort of African Americans: the Jackson Heart Study[J]. Am J Hypertens, 2013, 26(8): 1011-1016. DOI:10.1093/ajh/hpt064 |
| [5] |
GOUDOT G, PAPADACCI C, DIZIER B, et al. Arterial stiffening with ultrafast ultrasound imaging gives new insight into arterial phenotype of vascular ehlers-danlos mouse models[J]. Ultraschall Med, 2019, 40(6): 734-742. DOI:10.1055/a-0599-0841 |
| [6] |
WHELTON PK, CAREY RM, ARONOW WS, et al. Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines[J]. Circulation, 2018, 138(17): e426-e483. DOI:10.1161/CIR.0000000000000597 |
| [7] |
ABOYANS V, RICCO JB, BARTELINK MLEL, et al. 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO) the task force for the diagnosis and treatment of peripheral arterial diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS)[J]. Eur Heart J, 2018, 39(9): 763-816. DOI:10.1093/eurheartj/ehx095 |
| [8] |
MANCIA G, FAGARD R, NARKIEWICZ K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)[J]. J Hypertens, 2013, 31(7): 1281-1357. DOI:10.1097/01.hjh.0000431740.32696.cc |
| [9] |
PATETTA LMA, REFFO A, TREVISAN C, et al. Orthostatic hypotension and night-time dipper patterns in geriatric outpatients[J]. Hypertens Res, 2022, 45(9): 1468-1475. DOI:10.1038/s41440-022-00950-z |
| [10] |
KOLLIAS A, NTINERI A, STERGIOU GS. Association of night-time home blood pressure with night-time ambulatory blood pressure and target-organ damage: a systematic review and meta-analysis[J]. J Hypertens, 2017, 35(3): 442-452. DOI:10.1097/HJH.0000000000001189 |
| [11] |
YI JE, SHIN J, IHM SH, et al. Not nondipping but nocturnal blood pressure predicts left ventricular hypertrophy in the essential hypertensive patients: the Korean Ambulatory Blood Pressure multicenter observational study[J]. J Hypertens, 2014, 32(10): 1999-2004. DOI:10.1097/HJH.0000000000000272 |
| [12] |
BALDO MP, CUNHA RS, MOLINA MDCB, et al. Carotid-femoral pulse wave velocity in a healthy adult sample: the ELSA-Brasil study[J]. Int J Cardiol, 2018, 251: 90-95. DOI:10.1016/j.ijcard.2017.10.075 |
| [13] |
MIRAULT T, PERNOT M, FRANK M, et al. Carotid stiffness change over the cardiac cycle by ultrafast ultrasound imaging in healthy volunteers and vascular Ehlers-Danlos syndrome[J]. J Hypertens, 2015, 33(9): 1890-1896. DOI:10.1097/HJH.0000000000000617 |
| [14] |
SAFAR ME. Arterial stiffness as a risk factor for clinical hypertension[J]. Nat Rev Cardiol, 2018, 15(2): 97-105. DOI:10.1038/nrcardio.2017.155 |
 2023, Vol. 52
2023, Vol. 52




