文章信息
- 刘皇亮, 杨军, 杨茹, 孙彤, 吕沐天, 单忠艳
- LIU Huangliang, YANG Jun, YANG Ru, SUN Tong, LÜ Mutian, SHAN Zhongyan
- 中国北方社区人群体脂情况对颈动脉血管壁弹性的影响
- Effect of lipid status on carotid artery elasticity: a pilot study based on a northern Chinese community
- 中国医科大学学报, 2021, 50(6): 481-485, 490
- Journal of China Medical University, 2021, 50(6): 481-485, 490
-
文章历史
- 收稿日期:2021-01-15
- 网络出版时间:2021-05-26 16:41
2. 中国医科大学附属第一医院核医学科, 沈阳 110001;
3. 中国医科大学附属盛京医院核医学科, 沈阳 110004;
4. 中国医科大学附属第一医院内分泌与代谢病科, 沈阳 110001
2. Department of Nuclear Medicine, The First Hospital of China Medical University, Shenyang 110001, China;
3. Department of Nuclear Medicine, Shengjing Hospital of China Medical University, Shenyang 110004, China;
4. Department of Endocrinology and Metabolism, The First Hospital of China Medical University, Shenyang 110001, China
动脉粥样硬化(atherosclerosis,AS)可导致缺血性心脑血管疾病的发生和发展。动脉血管壁功能异常多发生在出现结构异常之前[1]。AS早期血管壁功能减低可通过血管壁弹性改变体现,用来评价血管壁弹性程度的超声指标包括脉搏波传导速度(pulse wave velocity,PWV)[2]等。目前,颈动脉PWV可通过极速成像(ultrafast imaging,UF)技术获得,利用20 000 Hz/s的极高帧频,根据组织多普勒算法,获得脉搏波收缩期起始时速度(PWV at the beginning of the systole,PWVBS)、脉搏波收缩期结束时速度(PWV at the ending of the systole,PWVES)及标准差。体脂百分比(body fat percentage,BFP)以及腰围(waist circumference,WC)、腰臀比(waist-to-hip-ratio,WHR)可以显示脂肪含量及分布情况。本研究拟应用UF获得颈动脉PWV,并分析中国北方成年人颈动脉管壁弹性程度与脂肪含量及分布的相关性。
1 材料与方法 1.1 研究对象选取中国北方某社区居民进行流行病调查,年龄40~70岁。排除患有严重心律失常、心脑血管疾病及感染等严重慢性病者;PWV无法测量或标准差Δ± > 10%者[1]。共纳入304例,其中,男151例,女153例。体质量指数(body mass index,BMI)≥24 kg/m2者纳入肥胖组,BMI < 24 kg/m2者纳入非肥胖组[3]。
1.2 仪器与方法采用法国声科Imagine AixPlorer型超声诊断仪,探头SLl0-2,频率6~9 MHz。在二维超声模式下颈总动脉长轴切面,开启“PWV”功能,维持探头稳定至图像采集完成,PWVBS、PWVES及标准差由系统自动测得。统计双侧PWV的平均值。BFP测定应用法国MEDI LINK OSTEOCORE2双能X线骨密度仪。受试者仰卧位,扫描从头顶至足尖,软件计算自动得出BFP。
统计年龄、性别、体质量、身高、WC及臀围(hip circumference,HC)、吸烟史(连续或累积吸烟6个月及以上)等信息;测量静息状态下收缩压(systolic blood pressure,SBP)及舒张压(diastolic blood pressure,DBP)3次,取平均值;采集生化指标:总胆固醇(total cholesterol,TC)、甘油三酯(triglycerides,TG)、低密度脂蛋白(low-density lipoprotein,LDL)、高密度脂蛋白(high-density lipoprotein,HDL)、空腹血糖(fasting plasma glucose,FPG)及血尿酸(blood uric acid,BUA);计算BMI=体质量(kg)/身高2(m2)[3];计算WHR=WC(cm)/HC(cm)。
1.3 统计学分析采用SPSS 23.0软件进行统计分析,计量资料以x±s表示,计数资料以n(%)表示。两变量相关性分析采用Spearman或Pearson相关分析,计量资料组间比较采用t检验,计数资料的比较采用χ2检验,采用多元线性回归分析PWV相关危险因素,P < 0.05为差异有统计学意义。
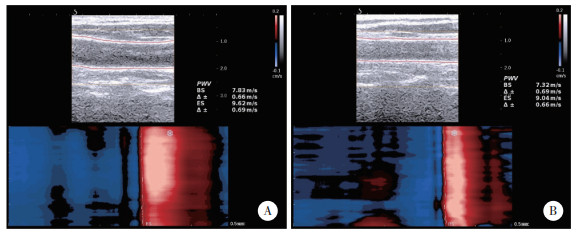
2 结果 2.1 研究对象的基本资料男性年龄40~70岁,平均年龄为(54.12±6.73)岁。女性年龄41~69岁,平均年龄为(53.85±7.30)岁。男性BMI、WC、WHR、SBP、DBP、FPG、TG、BUA及吸烟率高于女性,BFP低于女性,差异有统计学意义(P < 0.05)。男性PWVBS、PWVES与女性比较无统计学差异(P > 0.05)。见图 1、表 1。
|
| A,PWVBS and PWVES of male;B,PWVBS and PWVES of female. 图 1 超声极速成像技术测得的男性颈动脉PWV与女性颈动脉PWV Fig.1 PWV of the carotid artery measured by UF in the male and female groups |
| Characteristic | Male(n = 151) | Female(n = 153) | P |
| Age(x±s,year) | 54.12±6.72 | 53.85±7.30 | 0.738 |
| BMI(x±s,kg/m2) | 25.85±3.14 | 25.03±3.18 | 0.025 |
| WC(x±s,cm) | 91.76±8.65 | 85.09±10.87 | < 0.001 |
| WHR(x±s,%) | 89.54±6.77 | 85.58±9.23 | < 0.001 |
| SBP(x±s,mmHg) | 143.75±21.41 | 136.55±19.41 | 0.001 |
| DBP(x±s,mmHg) | 93.38±12.97 | 85.52±9.92 | < 0.001 |
| FPG(x±s,mmol/L) | 6.32±1.80 | 5.63±1.59 | < 0.001 |
| TC(x±s,mmol/L) | 5.08±0.97 | 5.21±1.04 | 0.286 |
| TG(x±s,mmol/L) | 1.79±1.45 | 1.41±1.06 | 0.008 |
| HDL(x±s,mmol/L) | 1.36±0.90 | 1.50±0.36 | 0.078 |
| LDL(x±s,mmol/L) | 3.31±0.84 | 3.37±0.90 | 0.548 |
| BUA(x±s,μmol/L) | 351.41±102.16 | 263.39±64.63 | < 0.001 |
| BFP(x±s,%) | 29.41±7.46 | 45.09±8.43 | < 0.001 |
| Smoking(%) | 74.80 | 5.20 | < 0.001 |
| PWVBS(x±s,m/s) | 5.62±1.11 | 5.60±1.24 | 0.837 |
| PWVES(x±s,m/s) | 8.46±1.73 | 8.68±1.66 | 0.251 |
2.2 肥胖组与非肥胖组指标比较
男性非肥胖组(n = 46)WC、WHR、DBP、TC、LDL、BUA及BFP低于男性肥胖组(n = 105),年龄及吸烟率高于肥胖组;女性非肥胖组(n = 65)WC、SBP、DBP、BUA及BFP低于女性肥胖组(n = 88);差异均有统计学意义(P < 0.05)。PWVBS和PWVES组间比较差异均无统计学意义(P > 0.05)。见表 2。
| Characteristic | Male | Female | |||
| Non-obesity(n = 46) | Obesity(n = 105) | Non-obesity(n = 65) | Obesity(n = 88) | ||
| Age(x±s,year) | 56.72±6.171) | 52.98±6.67 | 52.65±7.08 | 54.74±7.78 | |
| WC(x±s,cm) | 84.01±6.631) | 95.16±7.11 | 79.67±12.901) | 89.14±6.70 | |
| WHR(x±s,%) | 86.10±6.321) | 91.05±6.43 | 84.65±13.00 | 86.28±4.78 | |
| SBP(x±s,mmHg) | 140.48±20.36 | 145.18±21.79 | 130.23±17.751) | 141.23±19.36 | |
| DBP(x±s,mmHg) | 89.78±14.021) | 94.96±12.22 | 82.34±9.921) | 87.86±9.30 | |
| FPG(x±s,mmol/L) | 6.40±2.60 | 6.28±1.33 | 5.34±1.19 | 5.85±1.81 | |
| TC(x±s,mmol/L) | 4.82±0.941) | 5.20±0.96 | 5.13±0.89 | 5.27±1.14 | |
| TG(x±s,mmol/L) | 1.48±1.29 | 1.93±1.50 | 1.23±0.75 | 1.54±1.23 | |
| HDL(x±s,mmol/L) | 1.45±0.33 | 1.32±1.06 | 1.57±0.38 | 1.45±0.33 | |
| LDL(x±s,mmol/L) | 3.00±0.761) | 3.45±0.85 | 3.32±0.78 | 3.41±0.97 | |
| BUA(x±s,μmol/L) | 322.30±79.931) | 364.16±108.39 | 236.19±58.851) | 283.48±61.56 | |
| BFP(x±s,%) | 24.10±6.321) | 31.74±6.72 | 40.47±7.721) | 48.51±7.25 | |
| Smoking(%) | 91.301) | 67.62 | 6.82 | 3.08 | |
| PWVBS(x±s,m/s) | 5.39±0.96 | 5.72±1.16 | 5.51±1.19 | 5.66±1.28 | |
| PWVES(x±s,m/s) | 8.21±1.77 | 8.57±1.71 | 8.43±1.52 | 8.87±1.74 | |
| 1)P < 0.05 vs obesity group. | |||||
2.3 PWV与体脂及其他临床指标相关性分析
男性PWVBS与BMI、WC、SBP、DBP、TG、BUA及BFP呈正相关。男性PWVES与SBP、DBP、TG及BUA呈正相关,见表 3。女性PWVBS与年龄、WC、WHR、SBP、DBP及LDL呈正相关。女性PWVES与年龄、WC、SBP、DBP、HDL及BFP呈正相关,见表 4。
| Characteristic | PWVBS | PWVES | |||
| r | P | r | P | ||
| Age | 0.093 | 0.256 | 0.149 | 0.067 | |
| BMI | 0.167 | 0.040 | 0.130 | 0.111 | |
| WC | 0.199 | 0.014 | 0.149 | 0.067 | |
| WHR | 0.047 | 0.563 | -0.004 | 0.965 | |
| SBP | 0.230 | 0.004 | 0.332 | < 0.001 | |
| DBP | 0.293 | < 0.001 | 0.337 | < 0.001 | |
| FPG | -0.068 | 0.406 | -0.015 | 0.851 | |
| TC | 0.119 | 0.145 | 0.036 | 0.663 | |
| TG | 0.181 | 0.026 | 0.197 | 0.015 | |
| HDL | 0.026 | 0.749 | -0.009 | 0.910 | |
| LDL | 0.031 | 0.708 | 0.039 | 0.637 | |
| BUA | 0.240 | 0.003 | 0.229 | 0.005 | |
| BFP | 0.265 | 0.001 | 0.135 | 0.098 | |
| Smoking | 0.061 | 0.457 | 0.078 | 0.344 | |
| Characteristic | PWVBS | PWVES | |||
| r | P | r | P | ||
| Age | 0.212 | 0.009 | 0.380 | < 0.001 | |
| BMI | 0.016 | 0.840 | 0.125 | 0.122 | |
| WC | 0.234 | 0.004 | 0.246 | 0.002 | |
| WHR | 0.231 | 0.004 | 0.146 | 0.073 | |
| SBP | 0.230 | 0.004 | 0.337 | < 0.001 | |
| DBP | 0.169 | 0.037 | 0.274 | 0.001 | |
| FPG | 0.119 | 0.144 | 0.055 | 0.502 | |
| TC | 0.116 | 0.152 | 0.099 | 0.222 | |
| TG | -0.008 | 0.926 | 0.021 | 0.796 | |
| HDL | 0.085 | 0.297 | 0.174 | 0.032 | |
| LDL | 0.162 | 0.045 | 0.112 | 0.170 | |
| BUA | 0.080 | 0.324 | 0.151 | 0.062 | |
| BFP | -0.024 | 0.767 | 0.162 | 0.045 | |
| Smoking | 0.001 | 0.990 | -0.003 | 0.654 | |
2.4 PWV相关因素多元线性回归分析
以男性PWVBS为因变量,DBP、BFP及BUA是独立危险因素(表 5);以男性PWVES为因变量,DBP、年龄、BUA及TG是独立危险因素(表 6)。以女性PWVBS为因变量,SBP及WC是独立危险因素(表 7);以女性PWVES为因变量,年龄、DBP、HDL及WC是独立危险因素(表 8)。
| Item | B | SE | β | t | P |
| DBP | 0.023 | 0.006 | 0.22 | 2.66 | 0.01 |
| BFP | 2.487 | 1.207 | 0.17 | 2.06 | 0.04 |
| BUA | 0.002 | 0.001 | 0.19 | 2.45 | 0.02 |
| Item | B | SE | β | t | P |
| DBP | 0.039 | 0.009 | 0.30 | 4.08 | < 0.001 |
| Age | 0.055 | 0.019 | 0.22 | 2.90 | < 0.001 |
| TG | 0.181 | 0.087 | 0.15 | 1.99 | 0.050 |
| BUA | 0.003 | 0.001 | 0.20 | 2.62 | 0.010 |
| Item | B | SE | β | t | P |
| SBP | 0.013 | 0.005 | 0.20 | 2.48 | 0.01 |
| WC | 0.022 | 0.009 | 0.20 | 2.46 | 0.01 |
| Item | B | SE | β | t | P |
| Age | 0.078 | 0.016 | 0.34 | 4.71 | < 0.001 |
| DBP | 0.035 | 0.012 | 0.21 | 2.90 | < 0.001 |
| HDL | 1.016 | 0.333 | 0.22 | 3.05 | < 0.001 |
| WC | 0.027 | 0.011 | 0.17 | 2.27 | 0.020 |
3 讨论
UF测量颈动脉PWV具有操作简单等优势[4],能作为评价动脉弹性减低的指标[5]。肥胖的常用评价指标是BMI [3],但是由于体内脏器、肌肉、骨骼等影响,BMI评价肥胖存在局限性[6]。BFP能够直观显示体内脂肪占比。依照脂肪分布部位可以将肥胖分为周围型肥胖和腹型肥胖,评价腹型肥胖的指标为WC [3]和WHR[7]。本研究结果显示,BFP和WC分别作为男性和女性肥胖评价指标,对预防血管壁弹性减低更有意义。脂肪组织是一种具有内分泌及旁分泌功能的器官,体内堆积大量脂肪组织,罹患与脂肪相关疾病的风险升高,这种情况在内脏脂肪堆积时更为显著[8]。腹型肥胖能促进AS的发展已被许多研究[9]证实。女性体内的雌激素水平会在更年期及绝经后下降,增加肥胖风险,多表现为腹型肥胖,进而增加患心脑血管疾病的风险[10]。
有研究[5]表明,原发性高血压患者的血管壁弹性可以应用UF测量的颈动脉PWV进行早期评估。本研究结果中DBP作为独立危险因素,可引起女性PWVES及男性PWVES、PWVBS升高;SBP作为独立危险因素,可引起女性组PWVBS升高。男性组及女性组单纯收缩期高血压患者分别为3例及18例,且血压正常者及患1、2、3级高血压者构成比也略有区别,这可能会导致影响PWVBS升高的危险因素产生差异。
此外,HDL作为独立危险因素,可导致女性PWVES升高。以往经验认为较高水平的HDL能够减低AS相关疾病的患病风险[11]。但有学者[12]指出,冠状动脉粥样硬化性心脏病患者HDL提高72.1%,并没有降低血管不良事件发生率,相反却增高。另外有研究[13]显示,绝经后女性的HDL高于绝经前女性,在病态肥胖者中,绝经前和绝经后女性心血管疾病风险因素的差异减弱。
受限于被研究人群性别、人种、饮食结构等影响因素,BUA水平升高是否会促进AS发展尚无定论。本研究与既往针对国人的研究[14]结果相似,男性更需要关注BUA的变化,以预防血管弹性减低。
关于中国北方成年人血管壁弹性减低的危险因素,成年男性为脂肪含量增高,而成年女性为腹型肥胖。各因素对UF测量的PWV影响,还需要进一步结合相关药物综合分析。
| [1] |
邱兰燕, 钱林学, 刘冬, 等. 极速成像技术检测的脉搏波传导速度与颈动脉硬化相关性的研究[J]. 中华超声影像学杂志, 2014, 23(3): 203-205. DOI:10.3760/cma.j.issn.1004-4477.2014.03.008 |
| [2] |
《中国高血压防治指南》修订委员会. 中国高血压防治指南2018年修订版[J]. 心脑血管病防治, 2019, 19(1): 1-44. DOI:10.3969/j.issn.1009-816X.2019.01.001 |
| [3] |
中国心血管病风险评估和管理指南编写联合委员会. 中国心血管病风险评估和管理指南[J]. 中华预防医学杂志, 2019, 53(1): 13-35. DOI:10.3760/cma.j.issn.0253-9624.2019.01.004 |
| [4] |
PAN FS, YU L, LUO J, et al. Carotid artery stiffness assessment by ultrafast ultrasound imaging: feasibility and potential influencing factors[J]. J Ultrasound Med, 2018, 37(12): 2759-2767. DOI:10.1002/jum.14630 |
| [5] |
张光华, 安静, 洪林巍. 极速成像技术检测脉搏传导速度早期评价原发性高血压患者颈动脉弹性的研究[J]. 中国临床医学影像杂志, 2016, 27(4): 297-299. |
| [6] |
BOSELLO O, DONATACCIO MP, CUZZOLARO M. Obesity or obesities? Controversies on the association between body mass index and premature mortality[J]. Eat Weight Disord, 2016, 21(2): 165-174. DOI:10.1007/s40519-016-0278-4 |
| [7] |
EUN Y, LEE SN, JUNG J, et al. Association between waist-hip ratio and coronary artery calcification in postmenopausal women[J]. Menopause, 2020, 27(9): 1010-1014. DOI:10.1097/gme.0000000000001581 |
| [8] |
FERRIS WF, CROWTHER NJ. Once fat was fat and that was that: our changing perspectives on adipose tissue[J]. Cardiovasc J Afr, 2011, 22(3): 147-154. DOI:10.5830/cvja-2010-083 |
| [9] |
REIJRINK M, DE BOER SA, SPOOR DS, et al. Visceral adipose tissue volume is associated with premature atherosclerosis in early type 2 diabetes mellitus independent of traditional risk factors[J]. Atherosclerosis, 2019, 290: 87-93. DOI:10.1016/j.atherosclerosis.2019.09.016 |
| [10] |
HONG SC, YOO SW, CHO GJ, et al. Correlation between estrogens and serum adipocytokines in premenopausal and postmenopausal women[J]. Menopause, 2007, 14(5): 835-840. DOI:10.1097/gme.0b013e31802cddca |
| [11] |
TENENBAUM A, KLEMPFNER R, FISMAN EZ. Hypertriglyceridemia: a too long unfairly neglected major cardiovascular risk factor[J]. Cardiovasc Diabetol, 2014, 13: 159. DOI:10.1186/s12933-014-0159-y |
| [12] |
BARTER PJ, CAULFIELD M, ERIKSSON M, et al. Effects of torcetrapib in patients at high risk for coronary events[J]. N Engl J Med, 2007, 357(21): 2109-2122. DOI:10.1056/nejmoa0706628 |
| [13] |
VAN MIL SR, BITER LU, VAN DE GEIJN GJM, et al. The effect of sex and menopause on carotid intima-media thickness and pulse wave velocity in morbid obesity[J]. Eur J Clin Invest, 2019, 49(7): e13118. DOI:10.1111/eci.13118 |
| [14] |
HSU PF, CHUANG SY, CHENG HM, et al. Associations of serum uric acid levels with arterial wave reflections and central systolic blood pressure[J]. Int J Cardiol, 2013, 168(3): 2057-2063. DOI:10.1016/j.ijcard.2013.01.164 |
 2021, Vol. 50
2021, Vol. 50




