文章信息
- 崔作伟, 蒋晶晶, 吴秀英
- CUI Zuowei, JIANG Jingjing, WU Xiuying
- 超声引导下胸椎旁神经阻滞用于胸腔镜肺癌根治术麻醉及镇痛效果的临床观察
- Effects of Ultrasound-Guided Thoracic Paravertebral Block in Combination with General Anesthesia and Analgesia during Radical Thoracoscopic Surgery for Lung Cancer
- 中国医科大学学报, 2019, 48(4): 354-358
- Journal of China Medical University, 2019, 48(4): 354-358
-
文章历史
- 收稿日期:2017-10-31
- 网络出版时间:2019-04-14 7:03
胸腔镜下肺癌根治术是目前胸科常用的手术方式,与以往的手术方式相比较有切口小、术后恢复快等优势。但其术后的早期疼痛刺激与开胸手术类似[1],往往由于镇痛不彻底,使得肺部并发症增多,延缓了肺功能的恢复。当前的快速康复理念提倡加强围术期麻醉管理,减轻患者疼痛及不良反应,促进患者早期康复。经静脉患者自控镇痛(patient controlled intravenous analgesia,PCIA)是目前最常用的术后镇痛方式,但大量使用阿片类药物及非甾体类抗炎药同样会产生呼吸抑制、恶心呕吐等不良反应[2-3],因此,越来越多的学者[4-5]认为多模式镇痛在胸科手术中存在很大优势。
近年来,随着超声技术的引用,许多风险和失败率较高的传统镇痛方式应用越来越广泛,其中胸椎旁神经阻滞(thoracic paravertebral block,TPVB)取得了良好效果,RENSE等[6]报道了36例超声引导下的椎旁神经阻滞实验,成功率达100%。本研究探讨TPVB在胸腔镜肺癌根治术的应用,为临床应用提供参考。
1 材料与方法 1.1 研究对象选择2017年1月至9月于中国医科大学附属盛京医院进行的择期全麻下行胸腔镜肺癌根治手术的患者50例。纳入标准:年龄45~70岁,切口长度3~5 cm,ASA分级Ⅰ~Ⅱ级,体质量指数18.5~24.9 kg/m2,气道分级Ⅰ~Ⅱ级。排除标准:术前检查存在神经精神系统疾病史,严重心脏、肺、肝脏、肾脏疾病,胸廓或脊柱畸形,出凝血功能障碍,穿刺部位感染,局麻药过敏史等。本研究获得中国医科大学附属盛京医院伦理委员会批准,患者及家属签署知情同意书。
1.2 方法 1.2.1 麻醉方法入室后常规监测血压、心率、血氧,行有创血压监测。麻醉诱导采用长托宁0.5 mg、舒芬太尼0.4 μg/kg、依托咪酯0.3 mg/kg和顺苯磺酸阿曲库铵0.2 mg/kg。经口插入双腔支气管导管后行单肺容量控制通气,调节呼吸参数使呼气末二氧化碳维持在35~45 mmHg,脑电双频指数(bispectral index,BIS)维持在40~60。间断追加顺苯磺酸阿曲库铵0.03~0.06 mg/kg,术中补液按公斤体质量5 mL/(kg·h)。持续泵入瑞芬太尼、丙泊酚和吸入七氟烷,维持呼吸循环稳定。P组患者在全身麻醉后最低肺泡有效浓度(minimum alveolar concentration,MAC)达0.8时在超声引导下实行TPVB。手术结果前30 min给予酮咯酸氨丁三醇30 mg镇痛和盐酸雷莫司琼0.3 mg止吐,在关胸时停止丙泊酚和瑞芬太尼输注。拔管后根据患者状态及视觉模拟评分(visual analogue scale,VAS)决定是否给予舒芬太尼5 μg镇痛。镇痛泵配方为100 mL盐水内加入300 mg氟比洛芬酯和10 mg托烷司琼,持续泵注48 h,背景剂量2 mL/h。如镇痛效果不满意可口服泰勒宁325 mg。
1.2.2 神经阻滞方法P组患者在全麻后取侧卧位患侧在上,在超声引导下行TPVB,选择凸阵探头,频率为4 Mz。根据手术切口位置选择T4或T5下缘于脊柱旁2~3 cm处,沿脊柱平行的纵切面可观察到弓背弯曲两横突(柱形暗区),中间有一条线性亮影为胸膜,可观察到亮影随呼吸运动而上下摆动,在其上方有一黑色暗区即为椎旁间隙。采用平面外进针技术,到达位置回抽无气体和血液后注入2 mL盐水,观察胸膜亮影下移且黑色暗区增宽,然后注入0.3%的罗哌卡因10~15 mL。同理在T8同样注入5~10 mL,2处共计罗哌卡因100 mg,10 min后开始手术。
1.2.3 观察指标记录2组患者血压和心率的波动情况。手术过程中通过调节瑞芬太尼浓度来改变麻醉镇痛程度。血压或心率高于正常值20%时,静脉推注瑞芬太尼(0.5 μg/kg)并增加瑞芬太尼泵注剂量。在血压低于正常值20%或心率低于50次/min时使用麻黄素及阿托品治疗。拔管后送入术后恢复室,记录患者术后舒芬太尼的使用情况。记录患者术后30 min、6 h、12 h和24 h的VAS评分。术后24 h内使用泰勒宁的情况。
1.3 统计学分析采用spss 22.0统计软件进行分析,计量资料以x±s表示,2组间资料采用t检验比较,计数资料采用χ2检验进行比较。P < 0.05为差异有统计学意义。
2 结果 2.1 2组患者一般情况本研究共50例患者,其中1例患者术中大出血抢救,2例患者因术中需要改为开胸。最终47例患者纳入研究,其中实验组(P组)23例,对照组(G组)24例。2组患者的年龄、术前血压、心率、手术时间等无统计学差异(P > 0.05)。见表 1。
| Group | Age(year) | BP(mmHg) | HR(beat/min) | Hight(cm) | Weight(kg) |
| P | 58.61±5.74 | 92.61±8.48 | 72.52±10.24 | 165.26±7.02 | 62.37±10.38 |
| G | 59.17±4.30 | 95.92±6.73 | 73.5±11.51 | 165.29±8.67 | 64.85±9.66 |
| P | 0.707 | 0.145 | 0.76 | 0.989 | 0.565 |
| BP,blood pressure;HR,heart rate. | |||||
2.2 2组患者观察指标的变化情况
P组术中可以提供良好的镇痛效果,在切皮后P组血压和心率变化明显小于G组(P < 0.05),手术过程中使用的瑞芬太尼剂量也明显少于G组(P < 0.05)。P组患者术后苏醒期躁动的情况明显减少(P < 0.05)。2组患者手术过程中使用的血管活性药物无统计学差异(P > 0.05)。术后使用舒芬太尼和泰勒宁镇痛的患者人数明显少于G组(P < 0.05)。见表 2。
| Index | Group P(n = 23) | Group G(n = 24) | P |
| Change in blood pressure(x±s, mmHg) | 13.74±7.48 | 38.50±8.24 | < 0.001 |
| Change in heart rate(x±s, beat/min) | 5.35±4.56 | 16.17±4.56 | < 0.001 |
| Dose of remifentanil used every hour(x±s) | 235.83±23.13 | 320.44±34.63 | < 0.001 |
| Number of patients using sufentanil after extubation | 4 | 12 | 0.018 |
| Number of patients with dysphoria after extubation | 2 | 9 | 0.020 |
| Number of patients using tylox after the operation | 3 | 10 | 0.028 |
| Number of patients using ephedrine | 9 | 11 | 0.654 |
2.3 2组患者不同时间点的VAS评分
术后6 h内P组镇痛效果明显好于G组(P < 0.05),尤其是在麻醉结束后30 min内。虽然P组患者在12 h和24 h的时间点上VAS评分低于G组,但差异无统计学意义(P > 0.05)。见表 3。
| Group | 30 min | 6 h | 12 h | 24 h |
| P | ||||
| Resting | 3.30±0.7651) | 2.91±0.5151) | 2.57±0.507 | 2.13±0.344 |
| Coughing | 4.61±1.0301) | 4.13±0.7571) | 3.65±0.573 | 3.43±0.590 |
| G | ||||
| Resting | 4.63±0.824 | 2.91±0.515 | 2.62±0.494 | 2.33±0.481 |
| Coughing | 6.17±0.963 | 5.50±0.722 | 3.83±0.637 | 3.50±0.511 |
| 1)P < 0.05, compared with group G at the same time point. | ||||
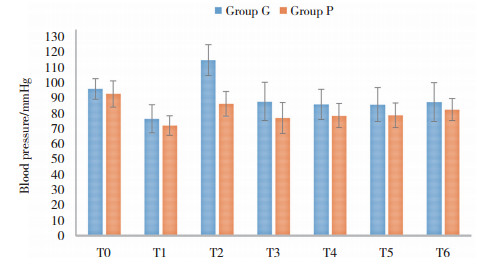
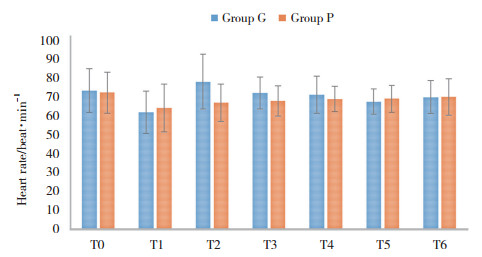
2.4 2组患者术中血流动力学的变化情况
2组患者除切皮后血压和心率变化较大之外(P < 0.05),其他时间的血压和心率均很稳定。P组术中各时间点的血压略低于G组,而心率较G组变化的更小,差异均无统计学意义(P > 0.05)。见图 1、2。
|
| 图 1 血压随时间变化的柱状图 Fig.1 Broken line diagram of changes in blood pressure with time |
|
| 图 2 心率随时间变化的柱状图 Fig.2 Broken line diagram of changes in heart rate with time |
3 讨论
胸腔镜手术目前是胸科手术最常用的手术方式,虽然其创伤小,但VOGT等[7]认为胸腔镜手术在早期仍可产生中等以上的疼痛刺激。主要来源于切口处在术中受到长时间的挤压所产生的炎症介质,引起术后的肋间神经痛,且术后置入引流管,在呼吸运动时,引流管皮肤切口处产生疼痛刺激,使患者不敢用力呼吸,同时疼痛刺激也可以抑制咳嗽反射,不利于患者早期排痰,继发性地增加了术后肺炎和肺不张的风险[8-10]。因此,良好的镇痛对于患者术后肺功能的恢复有着重要作用[11-12]。
TPVB是将局麻药注射到胸椎旁间隙以实现同侧相邻的多个节段躯体和交感神经的阻滞。传统的盲探法依靠阻力消失穿刺成功的只有50%,且并发症发生率高[13-14]。因此,在很长一段时间内在临床应用中受到了限制。但随着超声技术的引进,可以更加直观地观察到阻滞部位,提高了成功率,使阻滞更加充分,也降低了并发症的发生率[15]。本研究在超声引导下的23例患者均未出现上述并发症,有研究[16-17]发现,TPVB相对于硬膜外镇痛而言,两者效果相当,对应激反应及全身炎症反应的抑制程度、肺功能的影响无明显差别,但TPVB不会造成双侧阻滞,且对血流动力的影响更小。本研究也证实了P组在手术过程中与G组在血流动力学上无明显差别。因此,TPVB在胸腔镜肺癌根治手术中有着独特的优势。
本研究结果显示,P组患者获得了良好的镇痛效果,减少了阿片类和非甾体抗炎类药物的用量。术后6 h内的VAS评分明显低于G组。这与之前在其他类型的手术研究[18-20]中得到了相似的镇痛效果。还有研究[21]表明,疼痛刺激能够导致下丘脑—垂体—肾上腺皮质轴功能亢进,糖皮质激素和炎性细胞因子释放增多,作用于中枢神经系统和大脑海马区使患者发生精神紊乱和认知功能障碍的风险升高。本研究也证明了良好的神经阻滞镇痛使拔管后患者躁动的发生率明显降低。
本研究只观察了术后24 h内的镇痛情况,是由单次给药的作用时间和罗哌卡因的药效动力学决定的[22]。为了减少患者的紧张情绪及体动的不配合而采用全麻后实施神经阻滞,因此不能确定所有患者均成功阻滞。但2组患者在切皮前维持相同的麻醉深度和镇痛程度时,P组只有1例患者切皮时血压升高超过术前的20%,而G组所有患者在切皮时血压升高均超过术前的20%。因此,也可以从切皮后血压和心率的变化上侧面反映出TPVB的成功率以及镇痛程度。
综上所述,超声引导下TPVB镇痛效果良好,安全性高,减少了镇痛药物的应用,降低患者术后躁动发生率,提高患者满意度。不仅符合当前的快速康复理念,也为胸科手术围术期管理提供了帮助。
| [1] |
SENTURK M. Acute and chronic pain after thoracotomies:editorial review[J]. Curr Opin Anaesthesiol, 2005, 18(1): 1-4. DOI:10.1097/00001503-200502000-00002 |
| [2] |
BOTTIGER BA, ESPER SA, STAFFORD-SMITH M. Pain management strategies for thoracotomy and thoracic pain syndromes[J]. Semin Cardiothorac Vasc Anesth, 2014, 18(1): 45-56. DOI:10.1177/1089253213514484 |
| [3] |
FINE M. Quantifying the impact of NSAID-associated adverse events[J]. Am J Manag Care, 2013, 19(14): s267-s272. |
| [4] |
MARHOFER D, MARHOFER P, KETTNER SC, et al. Magnetic resonance imaging analysis of the spread of local anesthetic solution after ultrasound-guided lateral thoracic paravertebral blockade:a volunteer study[J]. Anesthesiology, 2013, 118(5): 1106-1112. DOI:10.1097/ALN.0b013e318289465f |
| [5] |
张高峰, 孙立新, 陈怀龙, 等. 不同镇痛方式在胸腔镜肺叶切除术患者术后镇痛效果的比较[J]. 临床麻醉学杂志, 2014, 30(10): 984-988. |
| [6] |
RENSE SH, BRUHN J, GIELEN MJ, et al. In-plane ultrasound guided thoracic paravertebral block:a preliminary report of 36 cases with radiologic confirmation of catheter position[J]. Reg Anesth Pain Med, 2010, 35(2): 212-216. DOI:10.1097/AAP.0b013e3181c75a8b |
| [7] |
VOGT A, STIEGER DS, THEURILLAT C, et al. Single injection thoracic paravertebral block for postoperative pain treatment after thoracoscopic surgery[J]. Br J Anaesth, 2005, 95(6): 816-821. DOI:10.1093/bja/aei250 |
| [8] |
DAS S, BHATTACHARYA P, MANDAL MC, et al. Multiple-injection thoracic paravertebral block as an alternative to general anaesthesiafor elective breast surgeries:a randomised controlledtrial[J]. Indian J Anaesth, 2012, 56(1): 27-33. DOI:10.4103/0019-5049.93340 |
| [9] |
FATMA NK, GURKAN T, ELIF BM. Thoracic paravertebral block for video-assisted thoracoscopic surgery:single injection versus multiple injections[J]. J Cardiothorac Vasc Anesth, 2012, 26(1): 90-94. DOI:10.1053/j.jvca.2011.09.008 |
| [10] |
MOAWAD HE, MOUSA SA, EI-HEFNAWY AS. Single-dose paravertebral blockade versus epidural blockade for pain relief after open renal surgery:a prospective randomized study[J]. Saudi J Anaesth, 2013, 7(1): 61-67. DOI:10.4103/1658-354X.109814 |
| [11] |
KAYA FN, TURKER G, MOGOL EB, et al. Thoracic paravertebral block for video-assisted thoracoscopic surgery:single injection versus multiple injections[J]. J Cardiothorac Vasc Anesth, 2012, 26(1): 90-94. |
| [12] |
FAHY AS, JAKUB JW, DY BM, et al. Paravertebral blocks in patients undergoing mastectomy with or without immediate reconstruction provides improved pain control and decreased postoperative nausea and vomiting[J]. Ann Surg Oncol, 2014, 21(10): 3284-3289. DOI:10.1245/s10434-014-3923-z |
| [13] |
WALKER BJ, LONG JB, DE OLIVEIRA GS, et al. Peripheral nerve catheters in children:an analysis of safety and practice patterns from the pediatric regional anesthesia network(PRAN)[J]. Br J Anaesth, 2015, 115(3): 457-462. DOI:10.1093/bja/aev220 |
| [14] |
RICHARDSON J, JONES J, ATKINSON R. The effect of thoracicparavertebral blockade on intercostal somatosensory evoked potentials[J]. Anesth Analg, 1998, 87(2): 373-376. |
| [15] |
VECCHIONE T, ZURAKOWSKI D, BORETSKY K. Thoracic paravertebral nerve blocks in pediatric patients:safety and clinical experience[J]. Anesth Analg, 2016, 123(6): 1588-1590. DOI:10.1213/ANE.0000000000001576 |
| [16] |
PINTARIC TS, POTOCNIK I, HADZIC A, et al. Comparison of continuous thoracic epidural with paravertebral block on perioperative analgesia and hemodynamic stability in patients having open lung surgery[J]. Reg Anesth Pain Med, 2011, 36(3): 256-260. DOI:10.1097/AAP.0b013e3182176f42 |
| [17] |
YOKOYAMA Y, NAKAGOMI T, SHIKATA D, et al. Combined analgesic treatment of epidural and paravertebral block after thoracic surgery[J]. J Thorac Dis, 2017, 9(6): 1651-1657. DOI:10.21037/jtd.2017.05.27 |
| [18] |
SARAN JS, HOEFNAGEL AL, SKINNER KA. Comparison of single-injection ultrasound-guided approach versus multilevel landmark-based approach for thoracic paravertebral blockade for breast tumor resection:a retrospective analysis at a tertiary care teaching institution[J]. J Pain Res, 2017, 28(10): 1487-1492. DOI:10.2147/JPR.S135973 |
| [19] |
GUPTA K, SRIKANTH K, GIRDHAR KK, et al. Analgesic efficacy of ultrasound-guided paravertebral block versus serratus plane block for modified radical mastectomy:a randomised, controlled trial[J]. Indian J Anaesth, 2017, 61(5): 381-386. DOI:10.4103/ija.IJA_62_17 |
| [20] |
SALVIZ, EMINE A, SIVRIKOZ NUKHET, OZONUR ANIL, et al. Ultrasound-guided bilateral thoracic paravertebral blocks as an adjunct to general anesthesia in patients undergoing reduction mammaplasty:a historical cohort study[J]. Plast Reconstr Surg, 2017, 139(1): 20-28. DOI:10.1097/PRS.0000000000002842 |
| [21] |
RASMUSSEN LS. Postoperative cognitive dysfunction:incidence and prevention[J]. Best Pract Res Clin Anaesthesiol, 2006, 20(2): 315-330. DOI:10.1016/j.bpa.2005.10.011 |
| [22] |
LI M, WAN L, MEI W. Update on the clinical utility and practical use of ropivacaine in Chinese patients[J]. Drug Des Develop Ther, 2014, 9(8): 1269-1276. DOI:10.2147/DDDT.S57258 |
 2019, Vol. 48
2019, Vol. 48




