文章信息
- 佟晶, 卑贵光, 李玉泽, 冉仪婷, 刘珈璐
- TONG Jing, BEI Guiguang, LI Yuze, RAN Yiting, LIU Jialu
- 体素内不相干运动成像和动态增强磁共振成像在子宫颈癌病理分级中的诊断价值
- Diagnostic Value of Intravoxel Incoherent Motion and Dynamic Contrast-Enhanced MRI in Pathological Grading of Cervical Cancer
- 中国医科大学学报, 2019, 48(12): 1112-1117
- Journal of China Medical University, 2019, 48(12): 1112-1117
-
文章历史
- 收稿日期:2019-04-03
- 网络出版时间:2019-12-05 16:12
子宫颈癌是女性常见的恶性肿瘤,发病率及死亡率呈上升趋势。子宫颈癌治疗方式及预后与病理分级密切相关[1],准确评估子宫颈癌病理分级对患者治疗方案的制订和预后预判极其重要。传统磁共振成像(magnetic resonance imaging,MRI)是诊断子宫颈癌的重要检查方法[2],但其对子宫颈癌病理分级缺乏特异性,近年来发展的体素内不相干运动(intravoxel incoherent motion,IVIM)成像和动态增强MRI(dynamic contrast enhanced-MRI,DCE-MRI)对子宫颈癌病理分级的价值日益受到国内外学者关注。IVIM和DCE-MRI可以用来评价子宫颈癌的微观结构及微循环情况[3],反映肿瘤不同分级程度在灌注上的差异。本研究探讨IVIM和DCE-MRI在子宫颈癌病理分级中的诊断价值。
1 材料与方法 1.1 研究对象回顾性分析我院放射科2017年6月至2018年5月经手术病理证实的71例子宫颈癌患者,年龄45~70岁,平均56岁。患者均术前2周内行IVIM成像和DCE-MRI检查。纳入标准:(1)病灶最大径≥1.0 cm;(2)术前未经任何治疗。排除标准:(1)经病理检查不能确定病理分级;(2)图像质量不能满足诊断要求。根据病理结果将患者分为3组:G1组(高分化,27例)、G2组(中分化,21例)和G3组(低分化,23例)。其中鳞癌46例,腺癌25例。ⅠB1期8例,ⅠB2期34例,ⅡA1期13例,ⅡA2期9例,ⅡB期7例。本研究通过我院伦理委员会审核并获得患者知情同意。
1.2 仪器与检查方法应用3.0 T MR扫描仪(Discovery MR750,美国GE Healthcare)和8通道控阵线圈对患者行盆腔MRI扫描。扫描序列包括(1)常规矢状位、轴位和冠状位T2WI(FSE序列,TR 3 156 ms,TE 85 ms,带宽50 kHz,矩阵320×224,FOV 26 cm×26 cm,层厚6.0 mm,层间距1.0 mm);(2)轴位T1WI(TR 450 ms,TE 6 ms,带宽83.33 kHz,矩阵256×192,FOV 26 cm×26 cm,层厚6.0 mm,层间距1.0 mm);(3)轴位多b值DWI(SE-EPI序列,TR 2 688 ms,TE 71 ms,带宽250.0 kHz,矩阵98×128,FOV 26 cm×26 cm,层厚6.0 mm,层间距1.0 mm,b值分别为0、10、20、50、100、200、400、800、1 200);(4)轴位动态增强序列(LAVA-T1WI,TR 3.9 ms,TE 2.2 ms,带宽166.7 kHz,反转角13°,矩阵320×200,FOV 38 cm×38 cm,层厚4.0 mm,无间断扫描10期,每期15 s,扫描第一期结束时经肘正中静脉团注Gd-DTPA,剂量0.2 mmol/kg,流率2 m/s)。
1.3 图像分析IVIM图像应用GEAW4.5 Functool MADC软件,处理生成表观扩散系数(apparent diffusion coefficient,ADC)、慢扩散系数(slow diffusion coefficient,D)、快扩散系数(fast diffusion coefficient,D*)及灌注分数(perfusion fraction,f)参数图,测量后计算D*与f乘积值(fD*)。DCE-MRI图像应用Functool自动分析软件,处理生成DCE-MRI半定量参数:最大上升斜率(maximum slop of increase,MSI)、最大下降斜率(maximum slop of decrease,MSD)、正性增强积分(positive enhancement integral,PEI)、信号增强比率(signal enhancement ratio,SER)。
在b=800 s/mm2扩散加权成像(diffusion weighted imaging,DWI)图像上高信号肿瘤层面,于肿瘤边缘手动绘制感兴趣区(region of interest,ROI),包含距肿瘤边缘5 mm以内的区域,同时结合T2WI和增强扫描图像避开坏死及囊变区[4]。每个病灶测量3次取其平均值,IVIM参数图和DCE-MRI参数图ROI放置尽量保持一致。
1.4 统计学分析应用SPSS 20.0软件对数据进行统计学分析。由于数据不服从正态分布,统计描述采用中位数(四分位间距)表示,组间比较采用Kruskal-Wallis H检验,组间差异有统计学意义者采用LSD检验进行组内两两比较。对存在统计学意义的各参数行受试者工作特征(receiver operating characteristic,ROC)曲线分析,计算曲线下面积(area under curve,AUC)和最佳截断值。应用Spearman秩相关分析研究各参数和病理分级的相关性以及两种方法参数间的相关性。P < 0.05为差异有统计学意义。
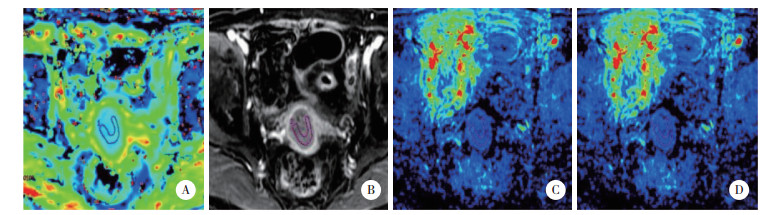
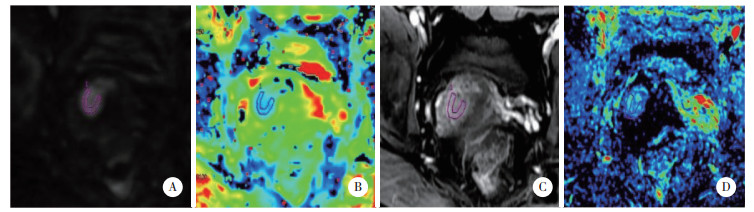
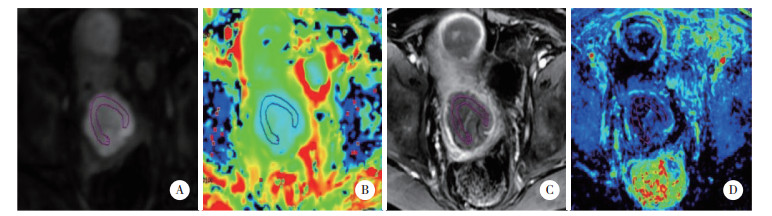
2 结果 2.1 子宫颈癌不同病理分级MRI参数比较结果显示,3组IVIM各个参数指标比较均有统计学差异(均P < 0.05)。G2组ADC值低于G1组,G3组D*值、fD*值低于G1组和G2组,G3组f值高于G1组和G2组,差异均有统计学意义(P < 0.05),见表 1。DCE-MRI半定量参数中MSD值组间比较均有统计学差异(均P < 0.05),见表 2、图 1~3。
| Group | ADC(×10-3 mm2/s) | D(×10-3 mm2/s) | D*(×10-3 mm2/s) | f(%) | fD* |
| G1 | 1.07(1.01,1.23)1) | 0.92(0.84,1.10)1),2) | 29.60(23.00,37.70)2) | 0.13(0.11,0.14)2) | 3.67(2.81,4.74)2) |
| G2 | 0.97(0.90,1.01) | 0.82(0.76,0.87)2) | 24.00(17.25,69.25)2) | 0.13(0.10,0.16)2) | 3.30(2.26,7.94)2) |
| G3 | 1.03(0.83,1.32) | 0.44(-0.27,0.76) | 5.04(2.46,27.40) | 0.42(0.11,0.81) | 2.06(1.68,3.12) |
| P | 0.034 | < 0.001 | 0.002 | 0.021 | 0.028 |
| 1) compared with G2 group, P < 0.05; 2) compared with G3 group, P < 0.05. ADC, apparent diffusion coefficient; D, slow diffusion coefficient; D*, fast diffusion coefficient; f, perfusion fraction. | |||||
| Group | MSI | MSD | PEI | SER |
| G1 | 49.32(36.32,70.60) | 51.03(33.33,70.04)1),2) | 46.68(13.70,82.39) | 59.28(44.94,97.96) |
| G2 | 40.49(29.99,267.45) | 50.33(12.33,64.15)1) | 24.41(9.84,406.99) | 47.78(24.56,79.02) |
| G3 | 56.43(29.19,151.43) | 18.91(15.98,37.66) | 73.34(33.16,197.88) | 55.13(29.41,74.92) |
| P | 0.962 | < 0.001 | 0.555 | 0.190 |
| 1) compared with G3 group, P < 0.05.2) compared with G2 group, P < 0.05. MSI, maximum slop of increase; MSD, maximum slop of decrease; PEI, positive enhancement integral; SER, signal enhancement ratio. | ||||
|
| A, DWI obtained with b of 800 s/mm2, ROI drawn at the edge of the tumor; B, on the D parametric map, the value of D was 0.86×10-3 s/mm2; C, on the dynamic contrast enhanced MRI, ROI was as consistent as possible with that on the DWI, avoiding necrosis and cystic area; D, on the MSD parametric map, the value of MSD was 61.73. 图 1 高分化子宫颈癌患者影像结果(女,59岁) Fig.1 Imaging results of a patient with highly differentiated cervical cancer (female, 59 years old) |
|
| A, DWI obtained with b of 800 s/mm2; B, on the D parametric map, the value of D was 0.79×10-3 s/mm2; C, dynamic contrast enhanced MRI; D, on the MSD parametric map, the value of MSD was 46.98. 图 2 中分化子宫颈癌患者影像结果(女,56岁) Fig.2 Imaging results of a patient with moderately differentiated cervical cancer (female, 56 years old) |
|
| A, DWI obtained with b of 800 s/mm2; B, on the D parametric map, the value of D was 0.76×10-3 s/mm2; C, dynamic contrast enhanced MRI; D, on the MSD parametric map, the value of MSD was 20.89. 图 3 低分化子宫颈癌患者影像结果(女,52岁) Fig.3 Imaging results of a patient with poorly differentiated cervical cancer (female, 52 years old) |
2.2 各参数诊断效能的ROC曲线分析
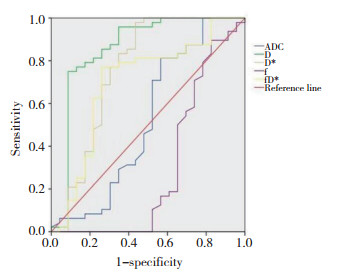
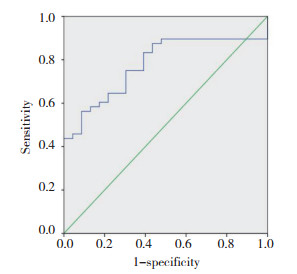
对有鉴别诊断意义的参数行ROC曲线分析,结果显示,IVIM参数中D对低分化子宫颈癌诊断的敏感度及特异度均高;其他参数敏感度高,特异度不高;DCE-MRI半定量参数MSD特异度高,敏感度不高,见表 3,图 4、5。
| Item | AUC | Cut-off | Sensitivity(%) | Specificity(%) |
| ADC | 0.525 | 0.903 | 81.3 | 43.5 |
| D | 0.857 | 0.793 | 75.0 | 91.3 |
| D* | 0.758 | 8.285 | 97.9 | 56.5 |
| f | 0.296 | 0.100 | 89.6 | 17.4 |
| fD* | 0.697 | 2.415 | 77.1 | 73.9 |
| MSD | 0.778 | 43.598 | 56.3 | 91.3 |
| ADC, apparent diffusion coefficient; D, slow diffusion coefficient; D*, fast diffusion coefficient; f, perfusion fraction; MSD, maximum slop of decrease. | ||||
|
| 图 4 IVIM各参数的ROC曲线 Fig.4 ROC curves of IVIM parameters |
|
| 图 5 DCE-MRI半定量参数中MSD的ROC曲线 Fig.5 ROC curves of MSD in the semiquantitative DCE-MRI parameters |
2.3 IVIM、DCE-MRI各参数之间及与病理分级的相关性分析
结果显示,D、D*、fD*及MSD与病理分级呈负相关(r分别为-0.620、-0.368、-0.270、-0.504,均P < 0.05),f与病理分级呈正相关(r = 0.287,P < 0.05)。ADC、D、D*及fD*与MSD呈正相关(r分别为0.312、0.435、0.282、0.254,均P < 0.05)。
3 讨论IVIM成像是在DWI技术基础上发展而来的一项新的功能磁共振技术。LE BIHAN等[5]提出的体素内不相干加权运动理论旨在将组织中进行布朗运动的纯水分子扩散与进行非布朗运动的微循环灌注相关的扩散区分开来,用以反映组织的微观结构及微循环情况。D为组织内水分子纯扩散系数,D*为微循环灌注相关系数,f为微循环灌注在DWI信号衰减中所占的比重[6]。目前很多研究[7-9]显示IVIM参数在子宫颈癌与正常子宫颈中有显著差异,但在子宫颈癌分级方面的研究结果尚不一致。LEE等[7]研究发现子宫颈癌的f值与D值显著低于正常子宫颈,而二者D*值无显著差异。李靖等[8]研究发现子宫颈癌的ADC值、D值及f值均显著低于正常子宫颈,D值较ADC值诊断子宫颈癌更准确。本研究对不同病理分级的子宫颈癌进行比较,发现IVIM-DWI各参数组间比较均有统计学差异,但仅D值在组内两两比较中有统计学差异,D值与低分化子宫颈癌病理分级呈负相关,可能是因为低分化子宫颈癌细胞增殖活跃,细胞密度增加,细胞内间隙减小,细胞内水分子扩散运动受限,进而导致D值降低。ZHOU等[4]研究发现不同病理分级子宫颈癌的ADC值、D值和f值差异显著(均P < 0.05),而D*值组间比较无统计学差异(P > 0.05)。相世峰等[10]研究发现中低分化子宫颈癌的ADC值与D值显著低于高分化子宫颈癌,而D*值与f值2组比较差异无统计学意义(P > 0.05)。张洁等[11]研究发现子宫颈癌级别越高D值越低,但不同级别子宫颈癌的D*值及f值未见显著差异。由此可见,D值对子宫颈癌分级的诊断价值较高,本研究中D*值和f值结果与其他研究不同,可能因为D*值和f值变异度较高。LEE等[12]研究发现fD*与子宫颈癌肿瘤毛细血管渗漏和血流量相关。本研究发现低分化子宫颈癌的fD*值显著低于中分化和高分化子宫颈癌,而中分化和高分化子宫颈癌的fD*值无统计学差异,其诊断价值尚需进一步研究证实。
DCE-MRI是通过注射对比剂前后连续的MRI扫描定量分析组织血管,对病变血液微循环和血管通透性进行评价[13]。DCE半定量参数中MSI反映微血管血液流入的速度,MSD反映微血管血液流出的速度,PEI与相对血容量有关,SER是病变增强前后灌注信号强度之差的绝对值同增强前信号强度之比,与组织微血管血容量、血管通透性及细胞外间隙有关。目前DCE-MRI半定量参数在子宫颈癌方面的研究大多为评估肿瘤放化疗的疗效及预后[14-15]。YANG等[14]研究发现MSI与子宫颈癌疗效相关,并且是肿瘤复发的独立危险因素。赵博等[15]研究发现MSI和PEI是子宫颈癌同步放化疗无疾病生存的影响因素。尚未发现DCE-MRI半定量参数在子宫颈癌病理分级方面的研究。本研究结果显示MSD值在不同级别子宫颈癌组间及组内比较中均有显著差异,且与病理分级呈负相关,可能是低分化子宫颈癌的微血管密度高于中分化和高分化子宫颈癌[16-17],加上血管更加扭曲走行紊乱,使其阻力相对增高,血流速度下降。
LE BIHAN等[18]首次研究IVIM和DCE灌注参数在脑部的相关性,发现f和脑血容量、D*和平均通过时间、fD*和脑血流量间具有相关性。随后不同研究者[19-22]尝试在多个系统论证IVIM和DCE灌注参数的相关性,但结论不一。本研究发现ADC值、D值、D*值及fD*值与MSD值呈正相关,其中D值与MSD值相关性最大。尽管DCE-MRI在子宫颈癌分级上有一定价值,但是临床应用受到数据获得和图像后处理的技术限制,而且可能存在引发磁共振钆对比剂相关的肾源性系统性纤维化的风险。IVIM优势在于不依赖外源性的磁共振对比剂,对新生毛细血管引起的不相干运动更敏感,而且较少受大血管的影响[23]。
综上所述,IVIM和DCE-MRI对子宫颈癌病理分级有一定的诊断价值,且两者部分参数具有相关性。本研究患者均依据术后病理进行子宫颈癌分级,比活检等方法得到的病理结果更准确,但是IVIM和DCE-MRI存在一定技术限制,模型和后处理方法、多b值的数量和大小等差异存在主观性,均可能使研究结果存在偏差。另外,本研究样本量偏少,仍需扩大样本量进一步论证。
| [1] |
FERLAY J, SOERJOMATARAM I, DIKSHIT R, et al. Cancer incidence and mortality worldwide:Sources, methods and major patterns in GLOBOCAN 2012[J]. Int J Cancer, 2015, 136(5): E359-E386. DOI:10.1002/ijc.29210 |
| [2] |
SALA E, ROCKALL AG, FREEMAN SJ, et al. The added role of MR imaging in treatment stratification of patients with gynecologic malignancies:what the radiologist needs to know[J]. Radiology, 2013, 266(3): 717-740. DOI:10.1148/radiol.12120315 |
| [3] |
DAPPA E, ELGER T, HASENBURG A, et al. The value of advanced MRI techniques in the assessment of cervical cancer:a review[J]. Insights Imaging, 2017, 8(5): 471-481. DOI:10.1007/s13244-017-0567-0 |
| [4] |
ZHOU Y, LIU JY, LIU CR, et al. Intravoxel incoherent motion diffusion weighted MRI of cervical cancer-Correlated with tumor differentiation and perfusion[J]. Magn Reson Imaging, 2016, 34(8): 1050-1056. DOI:10.1016/j.mri.2016.04.009 |
| [5] |
LE BIHAN D. Intravoxel incoherent motion imaging using steady-state free precession[J]. Magn Reson Med, 1988, 7(3): 346-351. DOI:10.1002/mrm.1910070312 |
| [6] |
TAMURA T, USUI S, MURAKAMI S, et al. Comparisons of multi b-value DWI signal analysis with pathological specimen of breast cancer[J]. Magn Reson Med, 2012, 68(3): 890-897. DOI:10.1002/mrm.23277 |
| [7] |
LEE EY, YU X, CHU MM, et al. Perfusion and diffusion characteristics of cervical cancer based on intraxovel incoherent motion MR imaging-a pilot study[J]. Eur Radiol, 2014, 24(7): 1506-1513. DOI:10.1007/s00330-014-3160-7 |
| [8] |
李靖, 曲金荣, 黎海亮, 等. 宫颈癌患者MR体素内不一致运动序列的成像特征[J]. 中华放射学杂志, 2013, 47(11): 1019-1022. DOI:10.3760/cma.j.issn.1005-1201.2013.11.015 |
| [9] |
胡莎莎, 陈小莉, 刘海峰, 等. 磁共振DWI、IVIM与宫颈癌病理学特征的相关性研究[J]. 磁共振成像, 2017, 8(10): 780-784. |
| [10] |
相世峰, 高云云, 张莉华, 等. 小视野体素不相干运动MRI在宫颈癌术前分级中的可行性[J]. 中国医学影像学杂志, 2015, 23(3): 219-221. DOI:10.3969/j.issn.1005-5185.2015.03.018 |
| [11] |
张洁, 薛华丹, 张玮, 等. 多b值DWI与宫颈癌病理学特征的相关性研究[J]. 放射学实践, 2014, 29(2): 127-130. DOI:10.13609/j.cnki.1000-0313.2014.02.006 |
| [12] |
LEE EY, HUI ES, CHAN KK, et al. Relationship between intravoxel incoherent motion diffusion-weighted MRI and dynamic contrast-enhanced MRI in tissue perfusion of cervical cancers[J]. J Magn Reson Imaging, 2015, 42(2): 454-459. DOI:10.1002/jmri.24808 |
| [13] |
TOFTS PS, BRIX G, BUCKLEY DL, et al. Estimating kinetic parameters from dynamic contrast-enhanced T (1)-weighted MRI of a diffusable tracer:standardized quantities and symbols[J]. J Magn Reson Imaging, 1999, 10(3): 223-232. DOI:10.1002/(SICI)1522-2586(199909)10:3<223::AID-JMRI2>3.0.CO;2-S |
| [14] |
YANG W, QIANG JW, TIAN HP, et al. Multi-parametric mri in cervical cancer:early prediction of response to concurrent chemoradiotherapy in combination with clinical prognostic factors[J]. Eur Radiol, 2018, 28(1): 437-445. DOI:10.1007/s00330-017-4989-3 |
| [15] |
赵博, 曹崑, 李晓婷, 等. MRI动态增强成像参数直方图分析对局部晚期宫颈癌放化疗后的预后评估价值[J]. 中华放射学杂志, 2019, 53(3): 218-223. DOI:10.3760/cma.j.issn.1005-1201.2019.03.011 |
| [16] |
LIU Y, YE ZX, SUN HR, et al. Grading of uterine cervical cancer by using the ADC difference value and its correlation with microvascular density and vascular endothelial growth factor[J]. Eur Radiol, 2013, 23(3): 757-765. DOI:10.1007/s00330-012-2657-1 |
| [17] |
KAN ZX, PHONGKITKARUN S, KOBAYASHI S, et al. Functional CT for quantifying tumor perfusion in antiangiogenic therapy in a rat model[J]. Radiology, 2005, 237(1): 151-158. DOI:10.1148/radiol.2363041293 |
| [18] |
LE BIHAN D, TURNER R. The capillary network:a link between IVIM and classical perfusion[J]. Magn Reson Med, 1992, 27(1): 171-178. DOI:10.1002/mrm.1910270116 |
| [19] |
BANE O, WAGNER M, ZHANG JL, et al. Assessment of renal function using intravoxel incoherent motion diffusion-weighted imaging and dynamic contrast-enhanced MRI[J]. J Magn Reson Imaging, 2016, 44(2): 317-326. DOI:10.1002/jmri.25171 |
| [20] |
MARZI S, PILUDU F, FORINA C, et al. Correlation study between intravoxel incoherent motion MRI and dynamic contrast-enhanced MRI in head and neck squamous cell carcinoma:Evaluation in primary tumors and metastatic nodes[J]. Magn Reson Imaging, 2017, 37: 1-8. DOI:10.1016/j.mri.2016.10.004 |
| [21] |
JIANG JX, XIAO ZB, TANG ZH, et al. Differentiating between benign and malignant sinonasal lesions using dynamic contrast-enhanced MRI and intravoxel incoherent motion[J]. Eur J Radiol, 2018, 98: 7-13. DOI:10.1016/j.ejrad.2017.10.028 |
| [22] |
林蒙, 张琪, 孔月, 等. 子宫颈癌IVIM与DCE-MRI灌注相关性研究[J]. 磁共振成像, 2018, 9(5): 354-359. |
| [23] |
FEDERAU C, O'BRIEN K, MEULI R, et al. Measuring brain perfusion with intravoxel incoherent motion (IVIM):initial clinical experience[J]. J Magn Reson Imaging, 2014, 39(3): 624-632. DOI:10.1002/jmri.24195 |
 2019, Vol. 48
2019, Vol. 48




