2. 中国医学科学院阜外心血管病医院冠心病中心,北京 100037
2. Center for Coronary Heart Diseases, Fuwai Hospital of Chinese Academy of Medical Sciences, Beijing 100037 China
冠心病是一种最常见的心脏病,严重危害人类健康,是60岁以上居民的首要死因[1]。2008年,全球有730万死于冠心病,2020年全球因冠心病导致的疾病负担达8200万伤残调整寿命年[2]。由于社会经济的快速发展、生活方式的改变、工作节奏的加快、人口老龄化等因素的影响,全球冠心病发病率呈逐年上升趋势[3-5]。随着冠状动脉血管造影术、冠状动脉支架植入术、搭桥手术等介入技术的快速发展,冠心病死亡率呈逐渐下降趋势[6-8]。
经皮冠状动脉介入治疗(percutaneous coronary intervention,PCI)可减轻冠状动脉狭窄和闭塞、改善缺血组织血供,是目前用于临床治疗冠心病的有效方法[9-10]。既往研究显示,心脏病患者接受PCI治疗后焦虑、抑郁、负面情绪等症状发生率上升,从而极大影响患者治疗、术后康复、加重患者及其家庭心理负担以及影响医务工作者工作积极性[11-12]。有研究报道,25%~50%接受冠状动脉支架植入术、搭桥手术等介入治疗的患者在术后3~6个月后变得焦虑和抑郁,从而可能导致死亡或心律失常,且在医疗资源匮乏及低文化程度地区更为严重[13-14]。但有关冠心病患者在接受PCI治疗后对焦虑和抑郁的影响尚少见报道。本研究采用焦虑和抑郁量表对600例冠心病患者PCI治疗后焦虑和抑郁发生情况进行了比较研究,结果报告如下。
1 对象与方法 1.1 伦理学声明本研究获取运城市第一医院医学伦理委员会审批通过,全部研究对象均在术前签署知情同意书,并知情所有接受的治疗获益、潜在风险等情况。
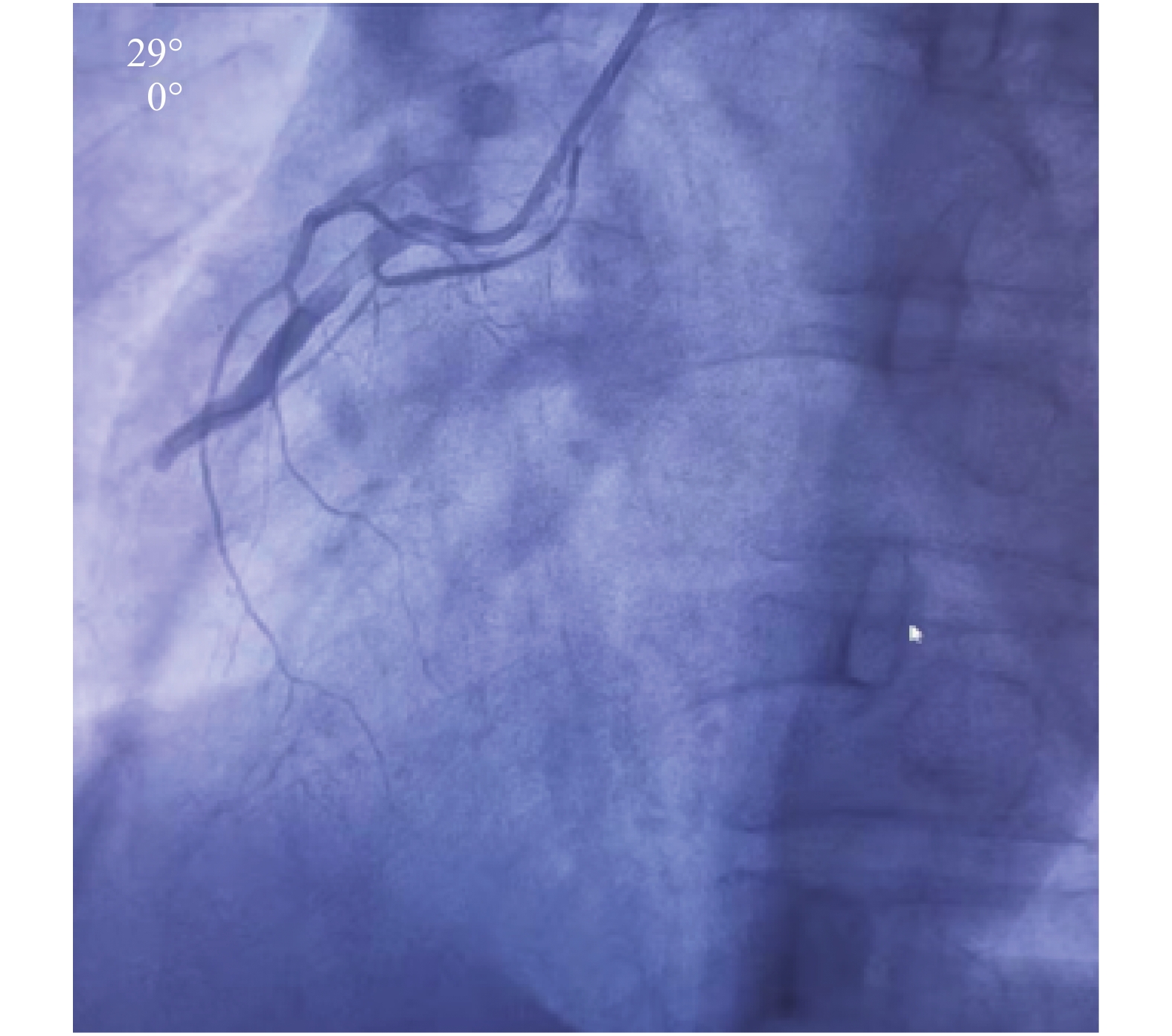
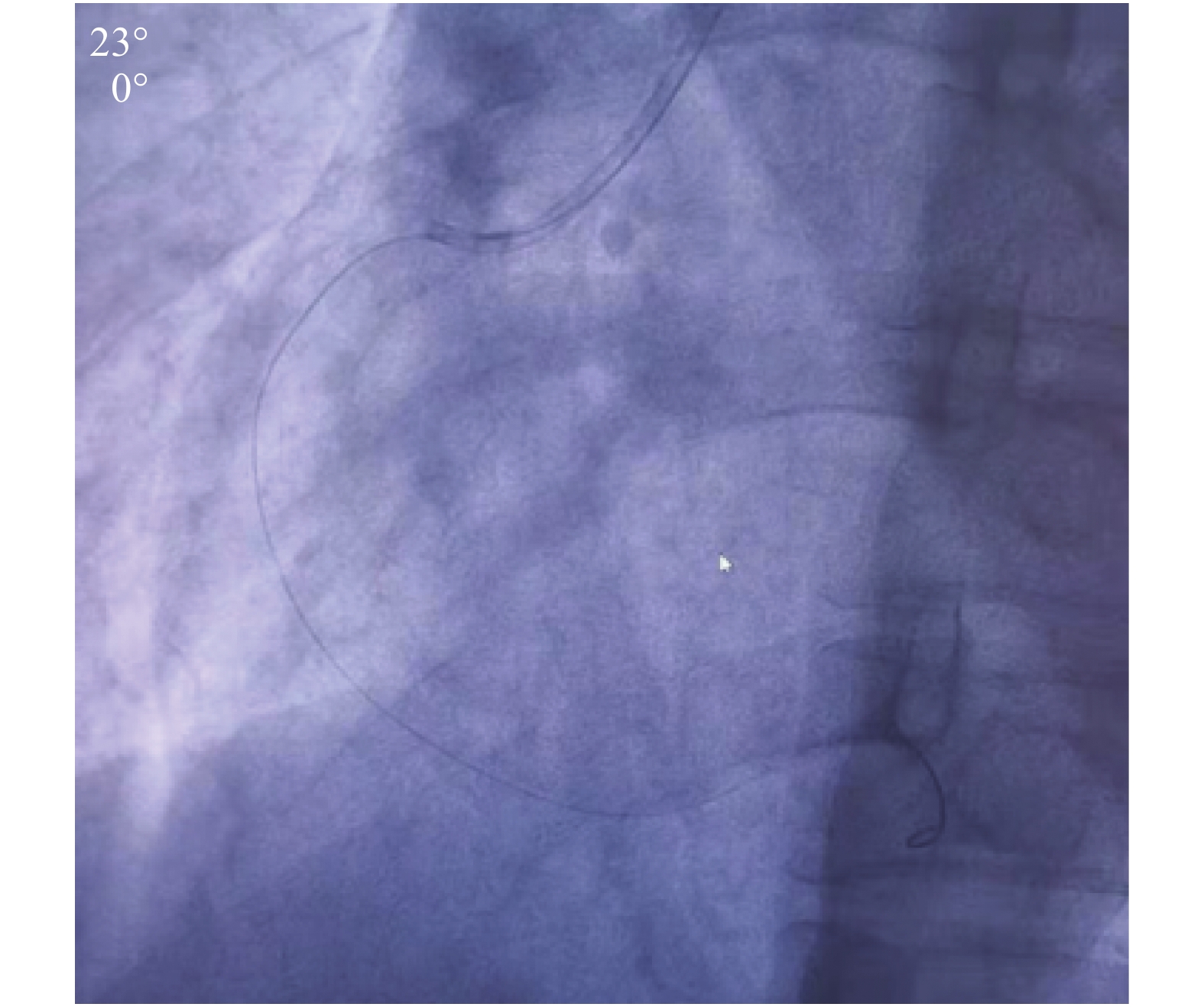
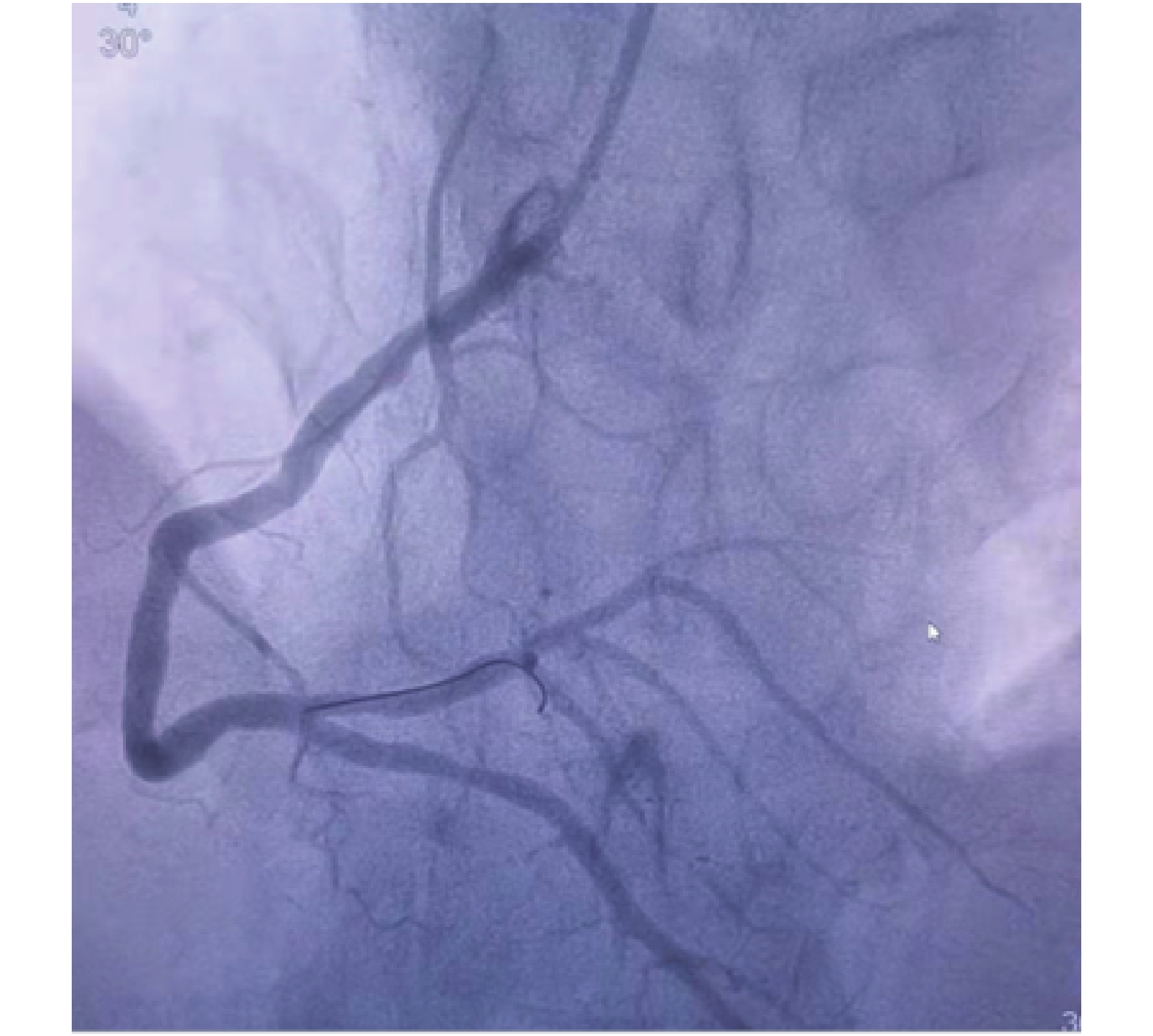
1.2 研究对象以2019年4月—2021年4月在运城市第一医院住院治疗的600例冠心病患者作为调查对象,所有病例均接受冠状动脉造影(图1~3)。病例纳入标准为:1)患者在入院后和整个治疗过程中生命体征平稳;2)患者入院时、入院后和整个治疗过程中血压稳定。病例排除标准包括:1)入院时生命体征不稳定、哺乳期妇女、孕妇、对药物治疗过敏的患者;2)严重肾病、甲状腺疾病、中风、恶性肿瘤、慢性感染、急性心力衰竭以及对碘奥酮过敏的患者;3)抑郁、焦虑、认知功能受损或简易智能精神状态检查量表评分≥27分的病例[15]。将患者分为支架组(n = 400)和非支架组(n = 200),其中支架组患者在冠状动脉造影时接受支架植入术治疗;400例支架组患者进一步随机分成干预组(n = 200)和非干预组(n = 200),其中干预组患者接受术后心理干预治疗。
|
图 1 患者PCI治疗术前冠状动脉造影检查结果 Figure 1 Coronary angiographic results in patients before PCI |
|
图 2 患者PCI治疗术中冠状动脉造影检查结果 Figure 2 Coronary angiographic results in patients during PCI |
|
图 3 患者PCI治疗术中冠状动脉造影检查结果 Figure 3 Coronary angiographic results in patients during PCI |
患者入院后1 d、行冠状动脉造影检查后1 d、出院时分别采用焦虑自我量表[16]和抑郁自我量表[17]对患者焦虑和抑郁状态填写量表。对于文化程度较低者,由医务人员用通俗易懂的语言向其解释量表及每项指标的具体含义,使其充分理解指标的意义后填写量表。
1.4 实验室检测采用实验室生化检测方法测定患者空腹血糖、总胆固醇、甘油三酯、低密度脂蛋白胆固醇和高密度脂蛋白胆固醇含量。
1.5 心理干预在支架植入后,全部患者均给予常规药物治疗。心理干预措施主要包括:①医务人员强化健康教育,耐心向患者解释冠状动脉介入治疗后应采取的防范措施和康复活动;所有患者均应注意监测血压、心率、氧饱和度等生命体征变化;并向患者耐心解释冠心病治疗和预后,以获取患者的信任。②术后给予患者充分人文关怀,给予患者心理暗示手术医生和护士均具有高超医技,并予以高品质、高质量医疗服务,从而帮助他们树立战胜疾病的信心。③术后医务人员应积极与病人沟通,帮助他们释放心理压力。鼓励患者与医生沟通内心想法,包括手术后身体状况、对疾病的了解、对手术的担忧、对预后的希望、如何更好的恢复健康等。④予以患者放松治疗,如深呼吸、听舒缓音乐等,从而帮助患者调节情绪、降低基础心率。⑤根据患者身体实际状态给予康复训练。⑥定期与患者沟通疾病进展和预后,向患者传达积极向上的情绪、减少焦虑和抑郁的危险因素。
1.6 统计学分析计量资料采用均数±标准差表示,多组间比较采用单因素方差分析和SNK法,干预前后比较采用t检验;计数资料采用频数或率表示,组间比较采用χ2检验。全部数据应用PASW 18.0软件进行统计分析,检验标准α=0.05。
2 结 果 2.1 一般情况干预组患者男性123例,女性77例;年龄45~64岁,平均(53.23 ± 10.21)岁。非干预组患者男性119例,女性81例;年龄43~66岁,平均(54.11 ± 12.19)岁。非支架组患者男性120例,女性80例;年龄41~66岁,平均(53.99 ± 11.87)岁。3组患者平均年龄、性别构成、血红蛋白含量、总胆固醇含量、低密度脂蛋白胆固醇含量和高密度脂蛋白胆固醇含量差异均无统计学意义(均P > 0.05)( 表1)。
|
|
表 1 不同组别冠心病患者一般情况比较 Table 1 Comparison of general conditions among patients with coronary heart disease at different groups |
入院后1 d,3组冠心病患者焦虑和抑郁评分差异均无统计学意义(均P> 0.05);PCI治疗后1 d,干预组和非干预组冠心病患者焦虑和抑郁评分均显著高于非支架组(均P< 0.05)。PCI治疗后1 d,干预组和非干预组冠心病患者焦虑(t = 11.21,P < 0.01;t = 9.96,P < 0.01)和抑郁评分( t = 8.56,P < 0.01;t = 6.73,P < 0.01)均显著高于治疗前( 表2、3),但非支架组冠心病患者PCI治疗前后焦虑和抑郁评分差异均无统计学意义(t = 1.11,P > 0.05;t = 0.91,P > 0.05)。
|
|
表 2 入院后1 d冠心病患者焦虑和抑郁状况比较 Table 2 Comparison of anxiety and depression scores among patients with coronary heart disease one day after admission |
|
|
表 3 PCI治疗后1 d冠心病患者焦虑和抑郁状况比较 Table 3 Comparison of anxiety and depression scores among patients with coronary heart disease one day after percutaneous coronary intervention |
出院时,3组冠心病患者焦虑和抑郁评分差异均有统计学意义(P < 0.05),干预组焦虑和抑郁评分均显著低于非干预组(均 P < 0.05)( 表4)。此外,干预组和非干预组冠心病患者出院时焦虑(t = 21.57,P < 0.01;t = 15.77,P < 0.01)和抑郁评分( t = 24.33,P < 0.01;t = 15.01,P < 0.01)均显著低于PCI治疗后 1 d。
|
|
表 4 出院时冠心病患者焦虑和抑郁状况比较 Table 4 Comparison of anxiety and depression scores among patients with coronary heart disease at discharge from hospital |
既往国内外学者对心脏病患者接受介入治疗后的郁闷和焦虑发生率进行了相关研究。戴玫等[18]调查发现,慢性阻塞性肺疾病合并冠心病患者支架植入后抑郁、焦虑患病率较植入前显著升高(P < 0.05)。孙毅等 [19]观察发现,冠心病患者在接受PCI治疗后焦虑和(或)抑郁症状发生率为42.6%,且预后较差。Zhang[20]研究发现,冠心病患者接受冠状动脉介入治疗后焦虑和抑郁状态明显加重。但亦有研究报道,成功的冠状动脉介入手术治疗并不能显著改善冠心病患者焦虑和抑郁状态[21-22]。此外,Kala等[23]报道,ST段抬高心肌梗死患者接受直接PCI治疗抑郁和焦虑症状发生率相对较低,而在治疗后1年逐渐升高。鉴于PCI治疗对心脏病患者焦虑和抑郁状态的影响尚存在争议,本研究对冠心病患者PCI治疗后焦虑和抑郁发生情况进行了观察。
本研究结果发现,冠心病患者接受PCI治疗后,焦虑和抑郁评分均显著高于未接受PCI治疗患者(均P < 0.05),且患者接受PCI治疗后的焦虑和抑郁评分均显著高于PCI治疗前(均 P < 0.01),与戴玫等 [18]、孙毅等[19]、Zhang[20]调查结果一致,但与任节等[21]、金晓萍等[22]、Kala等[23]报道结果不一致。可能与选择的调查对象、采用的焦虑和抑郁评分量表、介入治疗方法等不同有关。随着时间推移,患者出院时焦虑和抑郁评分显著低于PCI治疗后1 d,与既往报道结果一致[11,20]。
马跃文等[24]调查发现,心理干预联合运动训练可显著改善冠状动脉搭桥术后患者焦虑和抑郁评分、促进患者不良情绪改善。张月安等[25]探索出一套个体化认知行为干预措施,该措施可有效缓解冠心病患者PCI治疗后焦虑、紧张等负性情绪。席明霞等[26]比较了常规治疗 + 护理和常规治疗 + 护理 + 认知行为干预对PCI术后患者负性情绪的影响,发现2组患者焦虑和抑郁评分差异均具有统计学意义(均P < 0.01),从而认为认知行为干预可有效降低PCI术后患者负性情绪。Zhang [20]发现,冠心病患者PCI术后给予心理疏导和干预可改善焦虑、紧张等负性情绪。本研究发现,出院时干预组焦虑和抑郁评分均显著低于非干预组(均P < 0.05),提示心理干预可有效减轻冠心病患者焦虑和抑郁状态。
本研究结果表明,冠心病患者PCI术后焦虑和抑郁状态加重,但随着推荐而逐渐减轻;因此,应密切关注冠心病患者PCI治疗前后负性情绪变化。鉴于心理干预治疗可减轻焦虑和抑郁状态,应根据患者实际情况给予有针对性心理疏导和行为干预,从而减轻患者负性情绪、提高患者生命质量。
| [1] |
Sanchis-Gomar F, Perez-Quilis C, Leischik R, et al. Epidemiology of coronary heart disease and acute coronary syndrome[J]. Ann Transl Med, 2016, 4(13): 256. DOI:10.21037/atm.2016.06.33 |
| [2] |
Vilahur G, Badimon JJ, Bugiardini R, et al. Perspectives: The burden of cardiovascular risk factors and coronary heart disease in Europe and worldwide[J]. Eur Heart J Suppl, 2014, 16(suppl A): A7-A11. DOI:10.1093/eurheartj/sut003 |
| [3] |
Arciero TJ, Jacobsen SJ, Reeder GS, et al. Temporal trends in the incidence of coronary disease[J]. Am J Med, 2004, 117(4): 228-233. DOI:10.1016/j.amjmed.2004.04.008 |
| [4] |
Mensah GA, Roth GA, Fuster V. The global burden of cardiovascular diseases and risk factors: 2020 and beyond[J]. J Am Coll Cardiol, 2019, 74(20): 2529-2532. DOI:10.1016/j.jacc.2019.10.009 |
| [5] |
Joseph P, Leong D, McKee M, et al. Reducing the global burden of cardiovascular disease, part 1: the epidemiology and risk factors[J]. Circ Res, 2017, 121(6): 677-694. DOI:10.1161/CIRCRESAHA.117.308903 |
| [6] |
Meng Khoo C, Tai ES. Trends in the incidence and mortality of coronary heart disease in Asian Pacific region: the Singapore experience[J]. J Atheroscler Thromb, 2014, 21(Suppl1): S2-S8. DOI:10.5551/jat.21_sup.1-s2 |
| [7] |
Pagan E, Chatenoud L, Rodriguez T, et al. Comparison of trends in mortality from coronary heart and cerebrovascular diseases in north and south America: 1980 to 2013[J]. Am J Cardiol, 2017, 119(6): 862-871. DOI:10.1016/j.amjcard.2016.11.040 |
| [8] |
Vaartjes I, O'Flaherty M, Grobbee DE, et al. Coronary heart disease mortality trends in the Netherlands 1972-2007[J]. Heart, 2011, 97(7): 569-573. DOI:10.1136/hrt.2010.206565 |
| [9] |
Al-Lamee RK, Nowbar AN, Francis DP. Percutaneous coronary intervention for stable coronary artery disease[J]. Heart, 2019, 105(1): 11-19. DOI:10.1136/heartjnl-2017-312755 |
| [10] |
陈三保, 李毅, 裘淼涵, 等. 肝素与比伐芦定对女性冠心病患者经皮冠状动脉介入治疗影响比较[J]. 临床军医杂志, 2021, 49(3): 246-250. Chen SB, Li Y, Qiu MH, et al. Effects of heparin and bivalirudin on percutaneous coronary intervention in women with coronary heart disease[J]. Clin J Med Off, 2021, 49(3): 246-250. |
| [11] |
Roohafza H, Sadeghi M, Khani A, et al. Psychological state in patients undergoing coronary artery bypass grafting surgery or percutaneous coronary intervention and their spouses[J]. Int J Nurs Pract, 2015, 21(2): 214-220. DOI:10.1111/ijn.12234 |
| [12] |
Furuya RK, Costa Ede C, Coelho M, et al. Anxiety and depression among men and women who underwent percutaneous coronary intervention[J]. Rev Esc Enferm USP, 2013, 47(6): 1333-1337. DOI:10.1590/S0080-623420130000600012 |
| [13] |
Davidson PM, Salamonson Y, Rolley J, et al. Perception of cardiovascular risk following a percutaneous coronary intervention: a cross sectional study[J]. Int J Nurs Stud, 2011, 48(8): 973-978. DOI:10.1016/j.ijnurstu.2011.01.012 |
| [14] |
Dudek D, Datka W, Iwek MS, et al. The quality of life related to depressive symptoms in coronary artery disease patients after successful coronary angioplasty: one-year follow up[J]. Psychiatr Pol, 2007, 41(2): 229-242. |
| [15] |
方云华, 陈善佳, 周小炫, 等. MoCA、MMSE、NCSE等6个脑卒中认知康复评价工具的使用现状调查[J]. 中国康复, 2014, 29(1): 40-42. Fang YH, Chen SJ, Zhou XX, et al. Investigation on the use of 6 cognitive rehabilitation assessment tools[J]. Chin J Rehabilitation, 2014, 29(1): 40-42. DOI:10.3870/zgkf.2014.01.012 |
| [16] |
王文菁, 许明智. 焦虑自评量表在精神疾病患者中的因子结构研究[J]. 广东医学, 2009, 30(10): 1416-1418. Wang WJ, Xu MZ. Factorial structure of the self-rating anxiety scale patients with psychosis diseases[J]. Guangdong Med J, 2009, 30(10): 1416-1418. DOI:10.13820/j.cnki.gdyx.2009.10.069 |
| [17] |
苏占清, 康冰, 邵伟波, 等. 脑卒中后焦虑、抑郁自评量表测评的临床研究[J]. 现代康复, 2001, 5(3): 20-21. Su ZQ, Kang B, Shao WB, et al. A clinical study of post stroke evaluation with SAS and SDS[J]. Mod Rehabilitation, 2001, 5(3): 20-21. DOI:10.3321/j.issn:1673-8225.2001.03.006 |
| [18] |
戴玫, 曾雪峰, 王超, 等. 慢性阻塞性肺疾病合并冠心病患者支架植入前后抑郁焦虑情绪调查[J]. 中国呼吸与危重监护杂志, 2015, 14(5): 439-441. Dai M, Zeng XF, Wang C, et al. Analysis of depression and anxiety in patients with chronic obstructive pulmonary disease complicated coronary artery disease before and after percutaneous intracoronary arterial stenting[J]. Chin J Respir Crit Care Med, 2015, 14(5): 439-441. DOI:10.7507/1671-6205.2015109 |
| [19] |
孙毅, 张权宇, 刘威, 等. 经皮冠状动脉介入治疗术后冠心病患者合并焦虑和(或)抑郁对预后影响[J]. 临床军医杂志, 2020, 48(5): 518-520,525. Sun Y, Zhang QY, Liu W, et al. Effects of anxiety and/or depression on the clinical prognosis of patients with coronary artery disease after percutaneous coronary intervention[J]. Clin J Med Off, 2020, 48(5): 518-520,525. DOI:10.16680/j.1671-3826.2020.05.11 |
| [20] |
Zhang PY. Study of anxiety/depression in patients with coronary heart disease after percutaneous coronary intervention[J]. Cell Biochem Biophys, 2015, 72(2): 503-507. DOI:10.1007/s12013-014-0495-2 |
| [21] |
任节, 钱钧, 毛建华. 冠状动脉介入手术对冠心病患者心理状态影响[J]. 中华全科医学, 2010, 8(9): 1158-1159. Ren J, Qian J, Mao JH. Effect of interventional operation on mental state in patients with coronary heart disease[J]. Chin J Gen Pract, 2010, 8(9): 1158-1159. DOI:10.16766/j.cnki.issn.1674-4152.2010.09.030 |
| [22] |
金晓萍, 陈绍良, 单守杰, 等. 介入治疗对冠心病患者焦虑和抑郁状态的影响[J]. 实用心电学杂志, 2009, 18(2): 89-90. Jin XP, Chen SL, Shan SJ, et al. Psychological testing of patients with coronary heart disease before and after interventional operation[J]. J Pract Electrocardiol JS, 2009, 18(2): 89-90. DOI:10.13308/j.issn.1008-0740.2009.02.054 |
| [23] |
Kala P, Hudakova N, Jurajda M, et al. Depression and anxiety after acute myocardial infarction treated by primary PCI[J]. PLoS One, 2016, 11(4): e0152367. DOI:10.1371/journal.pone.0152367 |
| [24] |
马跃文, 刘畅, 朱佳琪, 等. 心脏康复促进冠状动脉搭桥术后患者体能恢复及不良情绪改善[J]. 中国动脉硬化杂志, 2012, 20(6): 536-540. Ma YW, Liu C, Zhu JQ, et al. The effects of rehabilitation on improving the physical capacity and ameliorating emotional disorders in patients of coronary artery bypass grafting[J]. Chin J Arterioscler, 2012, 20(6): 536-540. DOI:SUN:KDYZ.0.2012-06-013 |
| [25] |
张月安, 朱利军, 曾晓霞, 等. 个体化认知行为干预对经皮冠状动脉介入治疗术后患者负性情绪及预后的影响分析[J]. 中国药物与临床, 2016, 16(1): 62-64. Zhang YA, Zhu LJ, Zeng XX, et al. Impact of individualized cognitive behavioral interventions on negative emotions and prognosis among patients with percutaneous coronary intervention[J]. Chin Remedies Clin, 2016, 16(1): 62-64. DOI:10.11655/zgywylc2016.01.025 |
| [26] |
席明霞, 唐朝, 覃琴, 等. 认知行为干预对经皮冠状动脉支架植入术后患者负性情绪的影响[J]. 当代护士, 2015(7): 33-35. Xi MX, Tang (C/Z), Qin Q, et al. Impact of cognitive behavioral interventions on negative emotions among patients with percutaneous coronary stenting[J]. Today Nurse, 2015(7): 33-35. DOI:CNKI:SUN:DDHZ.0.2015-07-017 |




