癌症晚期患者往往伴随着多发转移,大约20%~40%的患者会有脑转移[1]。全脑放射治疗(Whole-brain radiotherapy,WBRT)是治疗脑转移的最常用方法之一[2-3]。目前WBRT常采用常规三维适形放疗(3-dimensional conformal radiation therapy,3D-CRT),即90°和270°两野对穿的照射技术[4],而中耳、咽鼓管峡部位于头颅两侧浅表处,应用此技术时,高剂量恰好沉积于此处。设计放疗计划时,物理师及医生往往更关注于晶状体、视神经等危及器官(Organ at risk,OAR)的剂量分布,而忽略了中耳、咽鼓管峡部的剂量分布[5]。在WBRT患者放疗后,偶有放射性中耳炎的发生,临床表现为外耳道溢液、流脓、胀痛等症状,影响了此类患者的生活质量。国内外学者对鼻咽癌等头颈部肿瘤放疗的中耳剂量学影响做了一些研究[5-7],但对在WBRT时中耳的剂量学研究少有报道。近年来,随着放射治疗技术的发展,调强放射治疗(Intensity modulated radiotherapy,IMRT)和容积旋转调强治疗(Volumetric arc modulated therapy,VAMT)等放疗技术的广泛使用,使得在 WBRT 时可以有效的降低中耳区域的剂量。本研究采用IMRT、VMAT和3DCRT 3种放疗技术进行对比,分析在WBRT中中耳腔和咽鼓管峡部的剂量学特点,为临床选择放疗技术的提供参考依据。
1 材料与方法 1.1 临床资料选取2018年7月1日—2019年8月1日我院收治的30例WBRT患者。其中男19例,女11例。年龄40~76岁,中位年龄61岁,KPS评分 ≥ 70。患者取仰卧位,使用热塑头膜及专用碳纤维板和头架、头枕固定后,在CT模拟定位机下增强扫描,CT扫描层厚0.3 cm,扫描范围为颅顶到第3颈椎,重建后将CT图像传输至瓦里安Eclipse放疗计划工作站。
1.2 靶区和OAR勾画靶区勾画:全脑组织为临床靶区(Clinical target volume,CTV),CTV三维方向外放0.3 cm为计划靶区(Planning target volume,PTV)。OAR勾画:包括中耳腔及咽鼓管峡部、眼球、晶体、视神经、视交叉。中耳腔及咽鼓管峡部结构如图1。
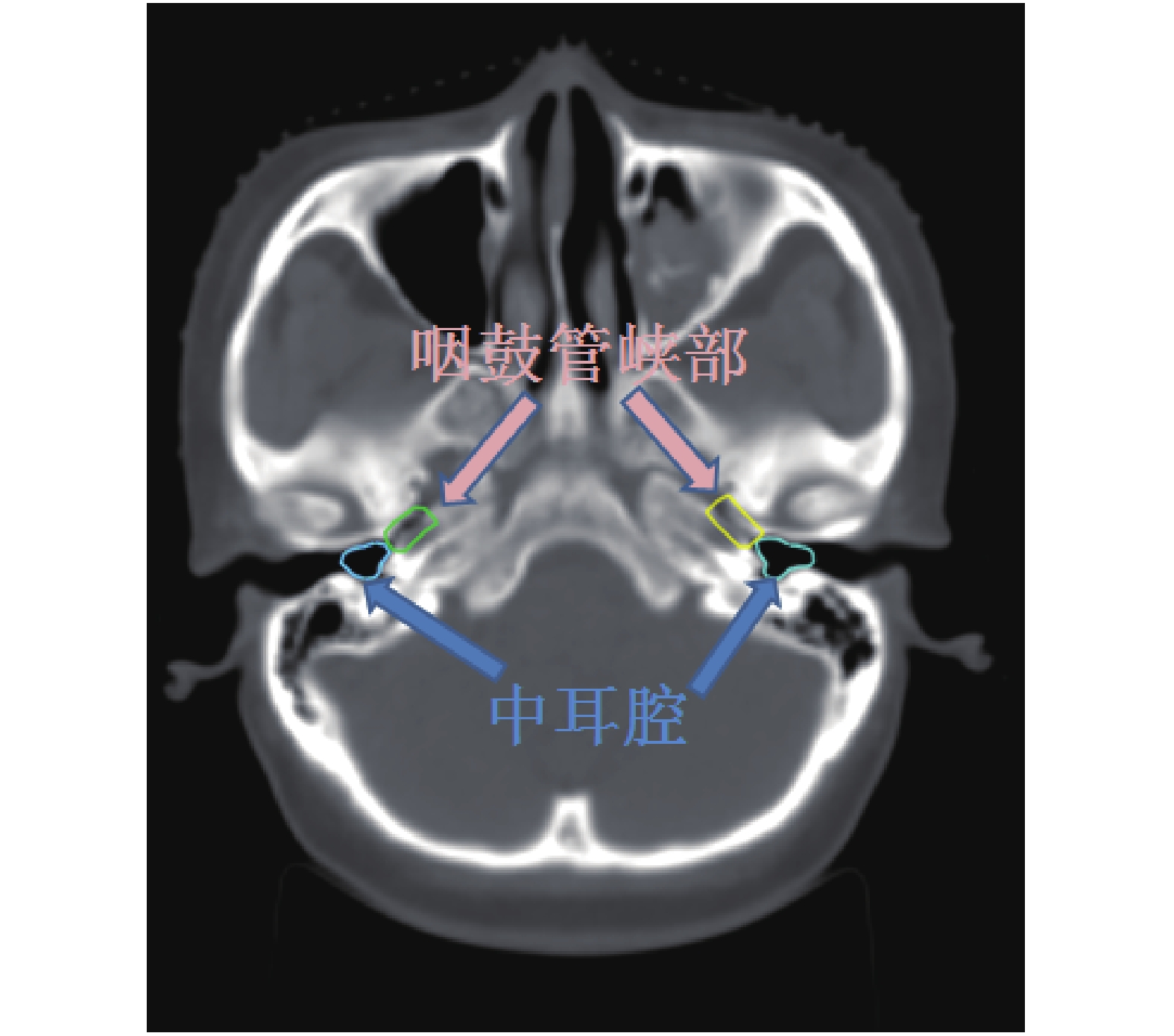
|
图 1 中耳腔及咽鼓管峡部的勾画 Figure 1 Delineation of middle ear cavity and eustachian tube isthmus |
在瓦里安Eclipse 13.6治疗计划系统(Treatment planning system,TPS)上设计放疗计划,对每个患者同一套CT图像分别设计固定野调强(Fixed field IMRT,ff-IMRT)、VMAT和3DCRT 3种治疗计划,能量为6MV-X射线,均为一个射野中心,计算方法为AAA算法,计算网格为2.5 mm,加速器机型为Varian trilogy,剂量率为500 MU/min,60对多叶光栅(MLC)。3种放疗计划的设计:(1)ff-IMRT计划,360°均分9个共面野,小机头0°;(2)VMAT计划,2个共面全弧,小机头为5°和355°;(3)3DCRT计划,90°和270°两个野对穿,PTV与MLC之间间隔0.5 cm。处方剂量为40 Gy/20 F。约束条件:处方剂量覆盖95%的PTV,PTV内Dmax小于110%的处方剂量,PTV 外不出现超过 110%处方剂量。
1.4 计划评估利用剂量-体积直方图(Dose-Volume histogram,DVH)来评价靶区和危及器官的剂量学参数,比较3种计划方式的PTV剂量分布。评估指标采用适形度指数(Conformity index,CI),均匀性指数(Homogeneity index,HI)、剂量梯度指数(Gradient index,GI)以及接受相应处方剂量照射体积百分比V95%、V110%、D98%、D95%、D2%、D50%,其中Vx%表示接受x%处方剂量的靶区体积,Dx%表示x% PTV所受到的照射剂量,D2%表示靶区最大剂量,D98%表示靶区最小剂量,D50%表示为靶区的中位剂量。CI= (VT,ref/VT) × (VT,ref/Vref),其中VT,ref为处方剂量所覆盖的靶区体积,VT为靶区体积,Vref为处方剂量所覆盖的总体积,CI取值为0~1,且越接近于1,靶区的适形度越好;HI = (D2% − D98%)/D50%,HI的理想值为0,HI值越大说明超过处方剂量越大,PTV内剂量分布也越不均匀;GI = V50%/V100%,GI越接近于1,剂量跌落越陡。比较3种计划OAR中耳腔、咽鼓管峡部的Dmax和平均剂量(Dmean),眼球、晶体、视神经、视交叉的Dmax。此外比较3种计划的机器跳数(Monitor unit,MU)。
1.5 统计学处理所有数据采用SPSS 22.0软件进行统计处理,数据以(
图2是3种治疗计划的断层图像剂量色阶图,图3是对应的DVH图。从色阶图及DVH图显示,3DCRT计划中耳及咽鼓管峡部剂量均高于ff-IMRT和VMAT2种调强计划。

|
图 2 ff-IMRT(a)、VMAT(b)、3DCRT(c)3种计划断层图 Figure 2 Tomography of ff-IMRT(a),VMAT(b),3DCRT(c)plans |
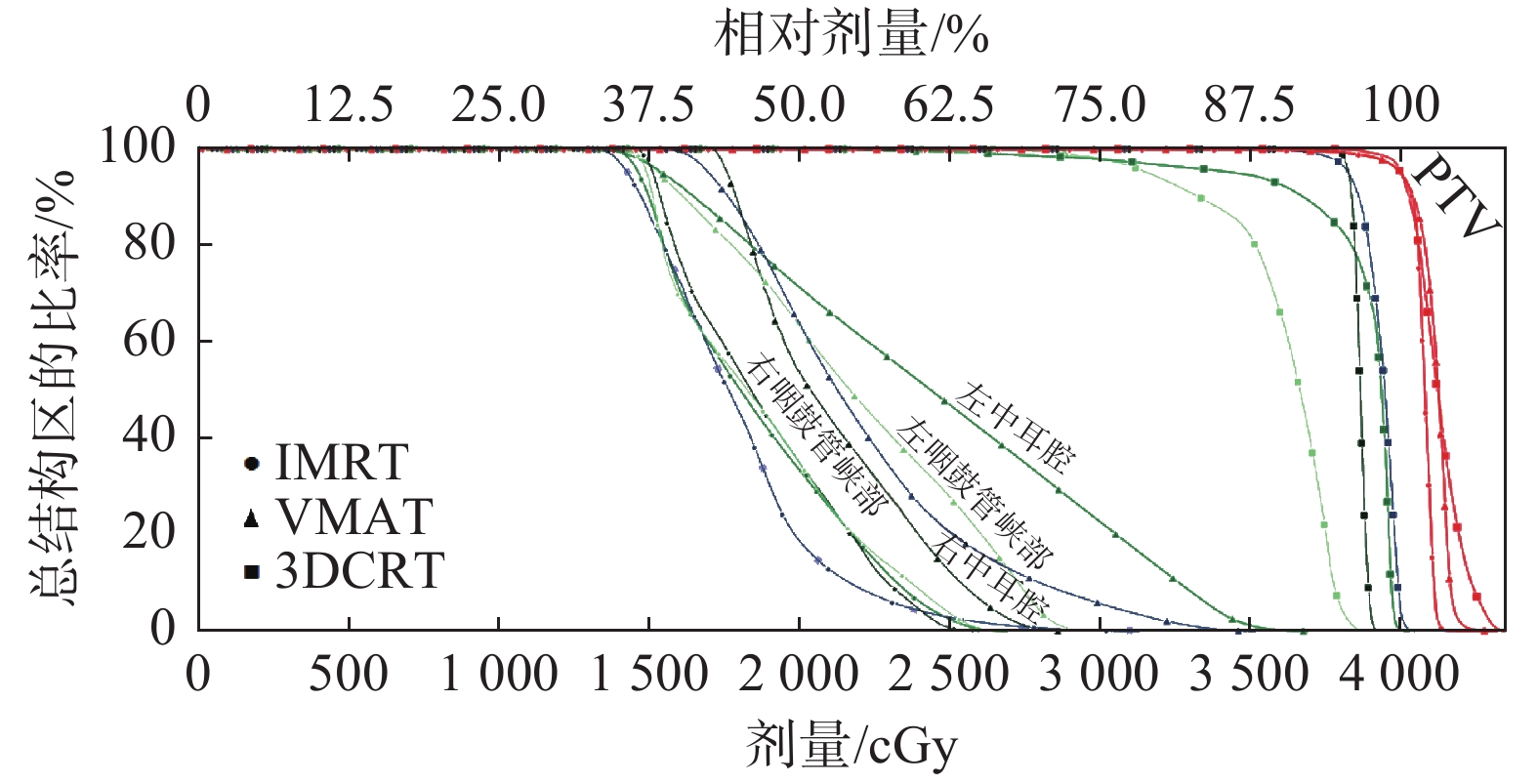
|
图 3 ff-IMRT(a)、VMAT(b)、3DCRT(c)3种计划剂量-体积曲线 Figure 3 DVH of PTV and middle ear cavity and eustachian tube isthmus |
3种计划的靶区最大值D2%、最小值D98%、平均值Dmean、CI、HI、GI的对比结果见表1。靶区D98%、D2%、Dmean,均为3DCRT计划组 > VMAT计划组 > ff-IMRT计划组,差异有统计学意义( P < 0.05);适形指数、梯度指数,均为3DCRT计划组 < VMAT计划组 < ff-IMRT计划组,差异有统计学意义( P < 0.05)。均匀性指数3种计划差异无统计学意义( P > 0.05)。
|
|
表 1 3种放疗计划靶区剂量学参数比较(
|
考虑到危及器官摆位误差等因素,使用“结构边界”功能建立中耳腔周围3 mm的三维边界作为计划危及器官(PRV)。3种计划的中耳腔最大值Dmax、平均值Dmean、对应PRV的最大值Dmax、平均值Dmean;咽鼓管峡部Dmax和Dmean如表2。3种放疗计划对中耳腔及其PRV、咽鼓管峡部剂量的Dmax、Dmean均为3DCRT计划组 > VMAT计划组 > ff-IMRT计划组,差异有统计学意义( P < 0.05)。
|
|
表 2 3种放疗计划中耳腔和咽鼓管峡部的剂量学参数比较(
|
由表3统计数据,左右晶体Dmax均是是3DCRT计划 < VMAT计划 < ff-IMRT计划,差异有统计学意义( P < 0.05)。左、右视神经的 Dmax是3DCRT计划 > VMAT计划 > ff-IMRT计划,视交叉的 Dmax是ff-IMRT计划 > 3DCRT计划 > VMAT计划,差异有统计学意义( P < 0.05);对于眼球,3种计划差异无统计学意义( P > 0.05)。
|
|
表 3 3种放疗计划危及器官的剂量学参数比较(
|
ff-IMRT、VMAT、3DCRT单次计划中各射野机器跳数MU累加之和分别为1551.97 ± 85.02、303.7 ± 24.28、226.2 ± 2.5,3者之间有统计学意义(P < 0.05)。
3 讨 论放射治疗是脑转移瘤常用的治疗方法。主要有WBRT、立体定向放射外科治疗(Stereotactic radiosurgery,SRS)、IMRT、VMAT等放疗方式,WBRT治疗脑转移瘤可提高患者中位生存期。但放射性中耳炎作为毒副反应降低了患者放疗后期的生活质量,临床目前尚无有效的治疗方法。通过本研究表明,IMRT、VMAT放疗技术可以降低中耳腔和咽鼓管峡部受量,从而有效的预防放射性中耳炎的发生。
目前国内外学者对WBRT的研究大多是与神经认知缺陷有关的海马体的研究[8-9],本研究较为系统地比较、分析了IMRT、VMAT和3DCRT 3种放疗方式在WBRT应用中对OAR及其PRV的剂量学影响,旨在为此类患者提供临床参考依据。对于放射性中耳炎的发生率,叶峰[10]报道了160例病人中耳腔、咽鼓管峡部中心点平均剂量分别为39 Gy、62 Gy,放疗半年内有65例(40.63%)出现听力下降。既往研究证实放射性中耳炎与中耳受照剂量有明确相关性[11],Wang等[12]和林浩然等[13]研究认为鼻咽癌放疗后发生放射性中耳炎与中耳腔和咽鼓管峡部的剂量有关。有报道[14]指出咽鼓管D100%为38 Gy,发生放射性中耳炎概率显著增加,剂量在30 Gy和40 Gy,放射性中耳炎发生概率为5%和50%。Pan等[15]和Chan等[16]报道了耳蜗剂量在45~60 Gy可导致听力受损,Wang SZ等[12]报道了中耳腔和咽鼓管峡部耐受剂量分别为34 Gy和40 Gy,叶峰等[10]则建议中耳腔剂量限制在34 Gy以下。Jereczek-Fossa等[17]报道了当咽鼓管和中耳平均剂量分别为33 Gy和30.9 Gy,3个月后发生放射性中耳炎比例为18%。本研究中,3DCRT放疗方式中耳腔的最大剂量为(4055.37 ± 71.45) cGy,大于VMAT(3107.9 ± 362.28) cGy和ff-IMRT(2557.54 ± 477.39) cGy 2种调强放疗方式,3DCRT放疗方式对中耳的剂量达到甚至超过了这些报道的耐受剂量,另外有研究认为,放疗同步放化疗对中耳的限制剂量比单纯放疗还应更低[18]。
本研究显示,ff-IMRT和VMAT在全脑放疗对中耳的保护方面明显优于3DCRT,靶区适形指数也有优势,但在机器跳数,VMAT和3DCRT比ff-IMRT更有优势。
综上,通过对 WBRT的剂量学分析,ff-IMRT和VMAT与3DCRT相比,均能对中耳起到保护作用,同时VMAT技术可以大大减少放疗时间,对WBRT更为合适,WBRT时建议使用VMAT技术。
| [1] |
Korkmaz Kirakli E, Oztekin O. Is hippocampal avoidance during whole-brain radiotherapy risky for patients with small-cell lung cancer?hippocampal metastasis rate and associated risk factors[J]. Technol Cancer Res Treat, 2017, 16(6): 1202-1208. DOI:10.1177/1533034617742301 |
| [2] |
孟曼, 毕金玲, 黄勇. 脑转移瘤全脑放疗疗效与预后相关因素分析[J]. 中国辐射卫生, 2019, 28(4): 458-461, 472. Meng M, Bi JL, Huang Y. Analysis of factors related to the efficacy and prognosis of brain metastases in whole brain radiotherapy[J]. Chin J Radiol Health, 2019, 28(4): 458-461, 472. DOI:10.13491/j.issn.1004-714x.2019.04.030 |
| [3] |
宋俊韬, 李学源, 聂东. 两种适形放疗技术在肺癌脑转移瘤中的疗效对比[J]. 中国辐射卫生, 2016, 25(1): 104-106. Song JT, Li XY, Nie D. Comparative analysis of two methods for 3D-CRT with brain metastases of non-small cell lung cancer[J]. Chin J Radiol Health, 2016, 25(1): 104-106. DOI:10.13491/j.cnki.issn.1004-714x.2016.01.042 |
| [4] |
陈杰, 朱云云, 陈明东, 等. 全脑照射调强放疗和常规放疗剂量学对比[J]. 医疗卫生装备, 2016, 37(2): 109-111. Chen J, Zhu YY, Chen MD, et al. Dosimetric comparision of cranial irradiation between intensity-modulated radiotherapy and conventional radiotherapy[J]. Chin Med Equip J, 2016, 37(2): 109-111. DOI:10.7687/J.ISSN1003-8868.2016.02.109 |
| [5] |
Upadhya I, Jariwala N, Datar J. Ototoxic effects of irradiation[J]. Indian J Otolaryngol Head Neck Surg, 2011, 63(2): 151-154. DOI:10.1007/s12070-011-0142-9 |
| [6] |
杨建明. 鼻咽癌放疗前后腭帆张肌横截面积的改变与放射性中耳炎的相关性[J]. 山东大学耳鼻喉眼学报, 2014, 28(1): 31-33. Yang JM. Relationship between radioactive otitis media and changes in cross section area of tensor veli palatine(TVP)muscle after radiotherapy in patients with nasopharyngeal carcinoma[J]. J Otolaryngol Ophthalmol Shandong Univ, 2014, 28(1): 31-33. DOI:10.6040/j.issn.1673-3770.0.2013.212 |
| [7] |
Hsin CH, Tseng HC, Lin HP, et al. Post-irradiation otitis media, rhinosinusitis, and their interrelationship in nasopharyngeal carcinoma patients treated by IMRT[J]. Eur Arch Otorhinolaryngol, 2016, 273(2): 471-477. DOI:10.1007/s00405-015-3518-8 |
| [8] |
Stoker J, Vora S, Patel A, et al. Advantages of intensity modulated proton therapy during hippocampal avoidance whole brain radiation therapy[J]. Phys Imaging Radiat Oncol, 2018, 8: 28-32. DOI:10.1016/j.phro.2018.11.001 |
| [9] |
单书灿, 欧丹, 韩一旻, 等. 全脑放射治疗海马区保护的剂量学研究[J]. 中国医学物理学杂志, 2019, 36(5): 546-550. Shan SC, Ou D, Han YM, et al. Dosimetric research on hippocampal-sparing whole brain radiotherapy[J]. Chin J Med Phys, 2019, 36(5): 546-550. DOI:10.3969/j.issn.1005-202X.2019.05.010 |
| [10] |
叶峰. 鼻咽癌调强放疗放射毒性与临床及放射剂量学因素的相关性分析[D]. 广州: 南方医科大学, 2012. Ye F. Analyses of clinical and dosimetric parameters associated with radiation-induced toxicities in patients with nasopharyngeal carcinoma treated with intensity-modulated radiation therapy[D]. Guangzhou: Southern Medical University, 2012. |
| [11] |
Wang SZ, Wang WF, Zhang HY, et al. Analysis of anatomical factors controlling the morbidity of radiation-induced otitis media with effusion[J]. Radiother Oncol, 2007, 85(3): 463-468. DOI:10.1016/j.radonc.2007.10.007 |
| [12] |
Wang SZ, Li J, Miyamoto CT, et al. A study of middle ear function in the treatment of nasopharyngeal carcinoma with IMRT technique[J]. Radiother Oncol, 2009, 93(3): 530-533. DOI:10.1016/j.radonc.2009.09.013 |
| [13] |
林浩然, 李郁明, 杨田福, 等. 鼻咽癌放疗并发分泌性中耳炎的临床病理特征及影响因素分析[J]. 临床医学工程, 2020, 27(7): 875-876. Lin HR, Li YM, Yang TF, et al. Analysis on the clinicopathological characteristics and influencing factors of nasopharyngeal carcinoma radiotherapy complicated with secretory otitis media[J]. Clin Med Eng, 2020, 27(7): 875-876. DOI:10.3969/j.issn.1674-4659.2020.07.0875 |
| [14] |
Akazawa K,Doi H, Ohta S, et al. Relationship between Eustachian tube dysfunction and otitis media with effusion in radiotherapy patients[J]. J Laryngol Otol, 2018, 132(2): 111-116. DOI:10.1017/S0022215118000014 |
| [15] |
Pan CC, Eisbruch A, Lee JS, et al. Prospective study of inner ear radiation dose and hearing loss in head-and-neck cancer patients[J]. Int J Radiat Oncol Biol Phys, 2005, 61(5): 1393-1402. DOI:10.1016/j.ijrobp.2004.08.019 |
| [16] |
Chan SH, Ng WT, Kam KL, et al. Sensorineural hearing loss after treatment of nasopharyngeal carcinoma: a longitudinal analysis[J]. Int J Radiat Oncol, 2009, 73(5): 1335-1342. DOI:10.1016/j.ijrobp.2008.07.034 |
| [17] |
Jereczek-Fossa BA, Rondi E, Zarowski A, et al. Prospective study on the dose distribution to the acoustic structures during postoperative 3D conformal radiotherapy for parotid tumors: dosimetric and audiometric aspects[J]. Et Al, 2011, 187(6): 350-356. DOI:10.1007/s00066-011-2170-5 |
| [18] |
Hitchcock YJ, Tward JD, Szabo A, et al. Relative contributions of radiation and cisplatin-based chemotherapy to sensorineural hearing loss in head-and-neck cancer patients[J]. Int J Radiat Oncol Biol Phys, 2009, 73(3): 779-788. DOI:10.1016/j.ijrobp.2008.05.040 |




