Current advances on the therapeutic potential of scutellarin: an updated review
Abstract
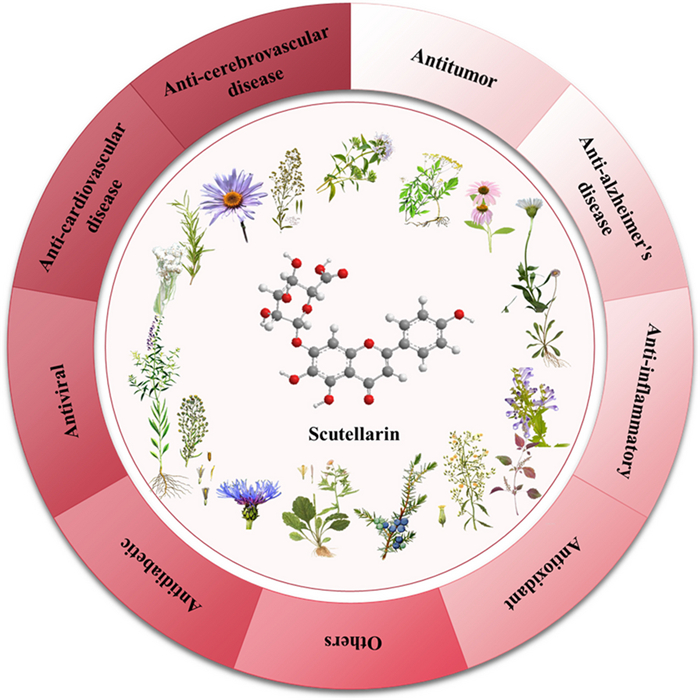
Scutellarin is widely distributed in Scutellaria baicalensis, family Labiatae, and Calendula officinalis, family Asteraceae, and belongs to flavonoids. Scutellarin has a wide range of pharmacological activities, it is widely used in the treatment of cerebral infarction, angina pectoris, cerebral thrombosis, coronary heart disease, and other diseases. It is a natural product with great research and development prospects. In recent years, with in-depth research, researchers have found that wild scutellarin also has good therapeutic effects in anti-tumor, anti-inflammatory, anti-oxidation, anti-virus, treatment of metabolic diseases, and protection of kidney. The cancer treatment involves glioma, breast cancer, lung cancer, renal cancer, colon cancer, and so on. In this paper, the sources, pharmacological effects, in vivo and in vitro models of scutellarin were summarized in recent years, and the current research status and future direction of scutellarin were analyzed.Graphical Abstract
Keywords
Scutellarin Pharmacological action Experimental study Model Mechanism1 Introduction
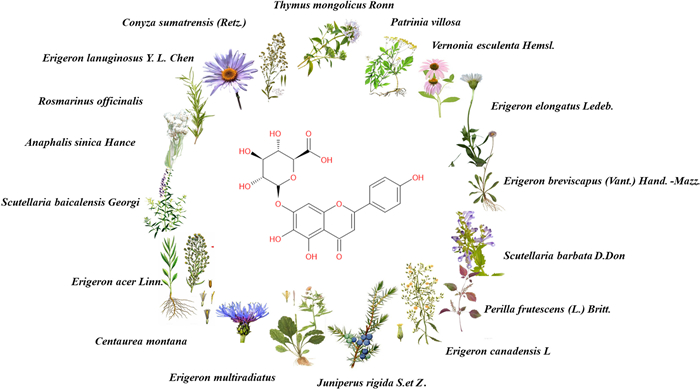
Scutellarin is a natural flavonoid extracted from plants that can be obtained from a variety of natural plants. Scutellarin is the main active substance, not only in Erigeron plants [1], but also widely distributed in Scutellaria plants [2], Opuntia plants [3], Centaurus plants [4], and Anaphalis plants [5]. Cumulative data show that scutellarin can be isolated from a variety of plants, such as Conya sumatrensis Retz [3], Centaurea montana [4], Anaphalis sinica Hance. [5], Vernonia esculenta Hemsl. [6], Erigeron breviscapus (Vant.) Hand.-Mazz. [7], Scutellaria barbata D. Don. [8], Scutellaria baicalensis Georgi. [9], Erigeron multiradiatus [10], Conyza canadensis L. [11], Thymus mongolicus (Ronniger) Ronn. [12], Perilla frutescens (L.) Britt. [13], Rosmarinus officinalis L. [14], Juniperus rigida S. et Z. [15], Patrinia villosa [16] etc. The structure, source, and function of scutellarin are shown in Fig. 1 and Table 1.
Structure and source of scutellarin
Distribution of scutellarin
Toxicological studies have proved that scutellarin is a slightly toxic or non-toxic natural small-molecule flavone compound, and the safe dose of LD50 value is 10 g/kg [17]. Based on the advantages of low toxicity and a wide range of sources, researchers found that scutellarin has a variety of pharmacological activities, including cardiovascular [18] and cerebrovascular diseases [19, 20], treatment of a variety of cancer therapies [21], and anti-inflammatory effects. In recent years, scutellarin played an important role in the treatment and protective effects of liver and kidney function caused by diabetes, the damage of brain, heart, liver, and kidney organs caused by alcohol, and eye diseases.
Animal models and cell models are important pharmacological research methods to evaluate drug activity and explore drug mechanisms, which usually need to be comprehensively evaluated by in vitro and in vivo methods combined with various models. Based on the study of different pharmacological activities of scutellarin in recent years, we combined the mechanism of scutellarin with in vivo and in vitro models to update the research progress of scutellarin’s pharmacological effects and look for changes and breakthroughs in recent years.
2 Pharmacological effects
2.1 Anti-cerebrovascular disease effect
Scutellarin is widely used in the clinical treatment of cerebral ischemia because of its anti-inflammatory, antioxidant, and vasodilator effects. The key feature of cerebral ischemia is that microglia in the brain evolve from a quiescent, branching morphology to an activated, unbranched, amoeboid morphology, which releases a large number of inflammatory mediators such as tumor necrosis factor-alpha (TNF-α), inter-leukin-1 beta (IL-1β), inducible nitric oxide synthase (iNOS), and other inflammatory mediators. TNF-α, IL-1β, iNOS, and reactive oxygen species (ROS), thereby exacerbating local inflammation and neuronal damage [22]. Chen et al. [23] found that scutellarin inhibited phosphorylated c-Jun N-terminal kinase (p-JNK), peripheral blood phosphorylated p38 mitogen-activated protein kinase (p-p38), and down-regulated inflammation in microglia by modulating the mitogen-activated protein kinases (MAPKs) pathway through the establishment of a permanent cerebral arterial occlusion model (MCAO). In addition, it can also significantly upregulate the expression level of extracellular signal-regulated kinase1/2 (p-ERK1/2), which can play a neuroprotective role. NIU [24] and others simulated neonatal hypoxic-ischemic disease (HIE) by culturing primary rat cerebral cortical neurons under the condition of hypoxia and glucose deficiency. After administration of scutellarin, it was found that scutellarin could inhibit neuronal death and regulate the Growth-associated protein (GAP43)-dependent pathway to promote axonal elongation of neurons, thus alleviating long-term nerve injury caused by HIE. Another study found that scutellarin can activate G-cyclase (GC) and produce cyclic guanosine monophosphate (cGMP) through endothelial-derived nitric oxide (NO), thus regulating the cGMP-dependent protein kinase (PKG) pathway [25–27]. PKG is a powerful vascular tone regulator. Activated PKG induces phosphorylation of vasodilator-stimulated phosphoprotein (Vasp), which in turn activates downstream ion channels and triggers endothelium-dependent vasodilation [28, 29]. DENG et al. found that scutellarin can repair oxidative stress injury in mice models of cerebral ischemia–reperfusion injury by down-regulating tMCAO-induced mRNA and protein expression of AR and NOX [30]. MENG et al. found that scutellarin can treat cerebral ischemia by regulating MARK, phosphatidylinositol 3 kinase (PI3K), hypoxia-inducible factor-1 (HIF-1), and other pathways, thus exerting vasorelaxation, anti-inflammatory and antioxidant effects [31]. Jia et al. [32] found through network pharmacology and experimental validation that Scutellarin exerts therapeutic effects on cerebral ischemia by activating astrocyte JAK2/STAT3 signaling, which provides a solid experimental basis for its clinical application. Xie et al. [33] found that Scutellarin exhibited antioxidant, anti-inflammatory, and neuroprotective effects in cerebral ischemia/reperfusion injury (CIRI) through PI3K/Akt pathway-mediated Nrf2 activation. Zhang et al. [34] found that scutellarin inhibits the inflammatory process through nuclear factor κ-B p65 and p38 mitogen-activated protein kinase signaling pathways and protects against brain damage in ischemically injured rats. Wang et al. [35] found that scutellarin exerts an effective effect on acute-phase ischemic brain injury by modulating neurotransmitter activity and reducing the toxicity of excitatory amino acids in neurons. M2 Microglia can exert neuroprotective effects and promote tissue repair. Chen et al. [36] found that scutellarin may directly promote the polarization of M2 microglia and their expression of neurotrophic factors. The protective effect was exerted through the inhibition of JNK and p38 signaling pathways. In addition, lucigenin promotes the polarization of M2 microglia by enhancing the ERK1/2 signaling pathway. In addition, scutellarin may also alleviate acute alcoholic brain injury by stimulating the activity of antioxidant enzymes and inhibiting the expression of syndromic factors [37]. Types of action and models of scutellarin in anti-cerebrovascular disease are showed in Table 2.
Types of action and models of scutellarin in anti-cerebrovascular disease
2.2 Anti-cardiovascular disease effect
Scutellarin has pharmacological effects such as slowing down heart rate, regulating myocardial contractility, dilating blood vessels, reducing cardiac preload and afterload, dilating coronary arteries, and increasing myocardial oxygen supply. It has been widely used in the clinical treatment of cardiovascular diseases. Li et al. [38] found that scutellarin mediates I/R-induced cardiomyocyte apoptosis and cardiac dysfunction by regulating the activation of Bcl-2/Bax/Caspase-3 signaling pathway, so as to improve treatment and improve ischemic heart disease. Zhou et al. [39] found that scutellarin ameliorates I/R-induced cardiomyocyte apoptosis and cardiac dysfunction by activating the Bcl-2/Bax/Caspase-3 signaling pathway via the cGAS-STING signaling pathway. Wang et al. [40] found that scutellarin protects against myocardial ischemia–reperfusion injury EPK1/2-CREB regulates mitochondrial autophagy. Fu et al. [41] found that scutellarin significantly reduced lipid levels and increased antioxidant enzymes in atherosclerotic (AS) rats by inhibiting mammalian sterile20-like kinases 1 (Mst1) phosphorylation, Yes-associated protein (YAP) phosphorylation, phosphorylation of forkhead box O3A (FOXO3a), nuclear translocation of FOXO3a, and up-regulation of protein kinase Bm (AKT) expression. Regulates downstream genes to inhibit vascular endothelial cell injury and apoptosis, thus exerting anti-AS effects. Scutellarin has also been used in the treatment of diabetic cardiomyopathy, where it can lower blood glucose, total cholesterol, triglyceride, and LDL levels, up-regulate HDL levels, down-regulate the levels of lactic dehydrogenase 1 (LDH1) and creatine kinase (CK), and promote mRNA and protein expression of autophagy-related factors Beclin-1 and Lc3-Ⅱ, and inhibit the apoptosis-related factors cysteine aspartic acid-specific protease (caspase), as well as the B-cell lymphocyte-associated X protein (BAX). Protein (BAX), and Cytochrome C (Cyt-C) mRNA and protein expression, thereby up-regulating autophagy-associated factors to promote autophagy signaling pathway and down-regulating apoptosis-associated factors to inhibit apoptosis signaling pathway, which improves the cardiac morphology and reduces apoptosis of cardiac myocytes and serves as a treatment for type 2 diabetic cardiomyopathy [42]. Huo and others [43] found that scutellarin could improve oxidative stress, inflammation, and reduce apoptosis by modulating NRF2/KEAP/ARE, TLR4/MYD88/NF-κB, and apoptosis pathways to treat and prevent myocardial injury complicated by type 2 diabetes mellitus. Qu et al. [44] used isolated rat hearts to study the effect of scutellarin on acute myocardial ischemia/reperfusion injury and found that scutellarin significantly increased the expression I/R (ischemia/reperfusion)-induced decrease in PPARγ and Nrf2 protein, and decreased the I/R-induced elevation of NF-κB protein expression to achieve cardioprotection. scutellarin- scutellarin (PAE) polylactic acid-glycidylglycolic acid (PLGA) nanoparticles (NPs) made by combining scutellarin with PLGA were able to reduce CK, LDH, and AST levels in serum, decrease apoptosis, and improve cardiac function [45]. Types and models of scutellarin action in anti-cardiovascular diseases are shown in Table 3.
Types of action and models of scutellarin in anti-cardiovascular disease
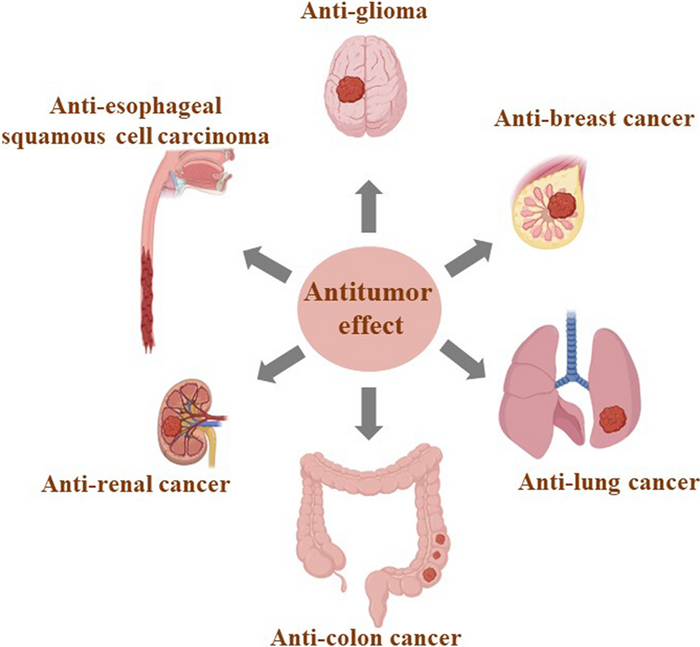
2.3 Antitumor effect
In vivo and in vitro studies have shown that scutellarin can be used for the prevention and treatment of a variety of human cancers, and the types of cancers are shown in Fig. 2. Types of action and models of scutellarin in antitumor effects are shown in Table 4.
Categories of human cancers that can be prevented and treated by scutellarin
Types of action and models of scutellarin in anti-tumor effect
2.3.1 Anti-colon cancer effect
Zeng et al. [46] found that scutellarin reduced the expression levels of TNF-α and TNF-1β in mouse serum, up-regulated the expression of BAX, and down-regulated the expression level of Bcl-2 in mouse cancer tissues through down-regulation of the Wnt/β-Catenin signaling pathway, and then inhibited the proliferation and migration of HT-29 cancer cells, and induced cell apoptosis. Scutellarin is one of the active ingredients of Erigeron breviscapu (Dengzhanxixin in China) injection (EBI). By activating the necrotic RIPK3/MLKL classical signaling pathway, EBI greatly promoted intracellular ROS production, significantly inhibited the proliferation of three human colorectal cancer (CRC) cell lines, and effectively inhibited the migration and invasion of SW620 cells, thus exerting anti-tumor effects. In addition, in the SW620 xenograft mouse model, EBI significantly inhibited tumor growth and lung metastasis and effectively circumvented drug-resistant apoptosis providing a new therapeutic pathway for anti-colon cancer [47]. Scutellarin significantly ameliorated AOM/DSS-induced CAC in mice and induced apoptosis in CAC tissues by inhibiting NF κB (nuclear factor κB)-mediated inflammation and the Hedgehog signaling axis. In addition, scutellarin inhibited cell proliferation, migration, and colony formation, and induced apoptosis in SW480 cells by down-regulating the Hedgehog signaling pathway activity, and reduced NFκB-mediated inflammatory responses in TNF-α-stimulated IEC-6 cells [48].
2.3.2 Anti-renal cancer effect
Deng et al. [49] found that scutellarin enhanced the expression of phosphatase and tensin homologue (PTEN) protein, a bispecific protein phosphatase identified as a tumor suppressor in a variety of human malignant tumors, and that activated PTEN caused second messenger lipid phosphatidylinositol 3,4,5-trisphosphate (PIP3) dephosphorylates, thereby contributing to its counteracting phosphatidylinositol-3-kinase (P13K) activity and AKT phosphorylation, inhibiting the PI3K/AKT pathway, which plays an important role in tumor cell proliferation, angiogenesis, and survival, and induces apoptosis of tumor cells, stalling their cell cycle at the G0/G1 phase, thus inhibiting the proliferation and invasion of renal cancer cells, suggesting that scutellarin has the potential to be a potential drug for the treatment of renal cancer.
2.3.3 Anti-lung cancer effect
TGF-β is considered a tumor suppressor due to its strong growth inhibitory activity in a wide range of cells. The TGF-β/Smad signaling pathway plays an important role in tumor cell proliferation, differentiation, and apoptosis. However, scutellarin modulates this pathway to induce apoptosis in tumor cells, and it has been reported that scutellarin selectively reduces the survival rate of tumor cells without affecting normal cells [50–53]. He and others [54] found that scutellarin could enhance 125I-induced apoptosis and the antiproliferative effect of tumor cells through down-regulation of the AKT/mTOR pathway, which provided the possibility of its combination therapy. Sun and others [55] found that scutellarin could promote caspase-3-dependent apoptosis induced by the first-line antitumor drug cisplatin via the ERK/P53 pathway and promote cisplatin-induced cytotoxicity autophagy via the c-Met-AKT pathway, which in turn acted to reverse the unique properties of cisplatin resistance.
2.3.4 Anti-glioma cancer effect
Wang et al. [56] found that scutellarin was able to inhibit the growth of glioma, as well as the proliferation and migration of glioma cells. In addition, scutellarin could significantly reduce the expression of baculovirus inhibitor of apoptosis protein 5 (BIRC5), thereby reversing the inhibition of apoptosis in glioma cells and exerting its anti-glioma effect. Therefore, Scutellarin may become a new potential targeted drug for the treatment of gliomas. Du et al. [57] found that Scutellarin inhibited the proliferation of glioma cells by upregulating miR-15a expression. Scutellarin-induced apoptosis and cell cycle in the G2/M phase SF-295 cell line inhibited cell proliferation in a dose-dependent manner and inhibited the growth of gliomas through the p63 signaling pathway in a dose-dependent manner, which was similar but weaker than the effect of 5-fluorouracil [58].
2.3.5 Anti-breast cancer effect
Triple-negative breast cancer (TNBC) is an aggressive breast cancer subtype with high blood vessels and frequent metastasis. Scutellarin blocks the interaction between TNF-α and TNFR2, and inhibits the activation of RUNX1 and the production of G-CSF in endothelial cells associated with TNBC downstream, thus reducing the metastasis of TNBC [59]. Scutellarin reduces the tendency of decreased connexin expression by regulating the TNFR2-ERK1/2-EZH2 signaling pathway, which inhibits TNF-α initiated vascular endothelial barrier disruption and thus reduces TNBC metastasis [60].
2.3.6 Treatment of other tumors
AKT is a serine/threonine kinase, belonging to the AGC family, which can regulate cell proliferation and survival, and scutellarin can activate this pathway, causing tumor cells to arrest with the G2 phase, which plays a role in the treatment of esophageal squamous carcinoma [61]. Girdin is an actin-binding protein, that is involved in cancer invasion and angiogenesis, and is a prognostic biomarker. Girdin can participate in pancreatic cancer (PaCa) migration mediated by EGF signal, and SCU can inhibit cancer invasion by inhibiting Girdin, thus playing a role in anti-cancer [62]. Li et al. used an aminoethyl anisamide-targeted copolymerization approach to amplify the delivery capacity of scutellarin to facilitate the in vivo application of scutellarin in hepatocellular carcinoma (HCC) immunotherapy and demonstrated that scutellarin has the potential to trigger immunogenic cell death (ICD) in hepatocellular carcinoma HCC [63]).
2.4 Anti-diabetic effect
2.4.1 Therapeutic effect on insulin resistance
Insulin resistance (IR) is a condition in which the peripheral tissues of the body become less sensitive to insulin and is present in various metabolic disorders such as diabetes mellitus, obesity, and hypertension. IR can occur in the liver, muscle, and adipose tissues, and when the levels of insulin, free fatty acids, or glucose in them are elevated tissues produce ROS and oxidative stress, as a vicious cycle IR and oxidative stress reinforce each other and exacerbate the body damage. LUAN et al. found that scutellarin reduced insulin-dependent lipid accumulation and mRNA expression upregulated Akt phosphorylation and improved the insulin signaling pathway in HepG2 cells in vitro. Down-regulation of rapamycin-targeted protein (mTOR) phosphorylation and n-SREBP-1c protein levels in high-fat diet (HFD)-fed mice and reduction of lipid accumulation in IR and lipid metabolism disorders through mTOR-dependent pathways [64]. Gao et al. found that scutellarin could activate the AMPK-α-mediated insulin signaling pathway, which in turn up-regulated P85α, activated the PI3K/AKT pathway, and ultimately affected the expression of the glucose transporter GLUT4, which indirectly exerted a hypoglycemic and lipid-lowering effect. in addition, scutellarin could also be a multi-targeted treatment for IR through its anti-oxidative stress, but the mechanism of the synergism of scutellarin’s modulation of the AMPK pathway and the anti-oxidative stress in the treatment of IR is still unclear and needs to be further investigated [65].
2.4.2 Antidiabetic-induced retinal injury
Scutellarin has a favorable therapeutic effect on diabetes-induced endothelial cell damage and retinopathy (DR). Scutellarin reduces the expression of BCL2, BAX, and fine cYTC, and inhibits apoptosis through a mitochondria-dependent pathway to treat diabetes-induced endothelial cell damage. Scutellarin also improves the decrease in mitochondrial membrane potential with ROS overload, decreases the protein expression of superoxide dismutase (SOD), and promotes the expression of microtubule-associated protein LC3II and autophagy-related gene ATG5. In addition, scutellarin can upregulate mitogen phagocytosis by modulating the PINK1/Parkin signaling pathway, thereby exerting a protective effect against hyperglycemia-induced vascular endothelial cell injury [66]. Vascular endothelial growth factor (VEGF) is the main cause of retinal neovascularization, vascular leakage, and is a therapeutic target for anti-angiogenesis in DR. Oral administration of scutellarin attenuates microvascular dysfunction caused by hyperglycemia and hypoxia in vitro and in vivo and inhibits vascular neovascularization, which may be related to its inhibition of VEGF and its downstream proteins, p-ERK, phosphorylated adhesion plaque kinase (p-FAK), and phosphorylated tyrosine protein kinase (p-Src) activation. It is evident that scutellarin is a VEGF inhibitor and has the potential to be a therapeutic agent for diabetic microangiopathy. Li et al. [67] found induced DR cell focussing in DM rats, particularly in retinal ganglion cells (RGCs), and found that scutellarin administration significantly inhibited cell focussing in DR and explained the molecular network mechanisms involved.
2.4.3 Antidiabetic-induced liver and kidney damage
Fan et al. [68] found that scutellarin may ameliorate T2DM liver injury by inhibiting hepatocyte apoptosis in vitro and in vivo. Huang et al. [69] found that scutellarin was effective in ameliorating various features of diabetic nephropathy (DN) in vivo, including proteinuria, glomerular dilatation, accumulation of tethered matrix, renal fibrosis, and podocyte injury, by modulating the TGF-β1 signaling pathway and its interaction with the Erk and Wnt/β-linker pathways. Scutellarin plays an important role in the treatment of diabetes and its complications, and types of action and models informations are showed in Table 5.
Types of action and models of scutellarin in anti-diabetic effect
2.5 Therapeutic role in Alzheimer’s disease
Alzheimer’s disease (AD) is a neurodegenerative disease associated with aging, characterized by progressive memory impairment, and cognitive and social decline. At present, there is no drug to cure this disease. As for the pathogenesis of AD, it is widely assumed that amyloid (Aβ) aggregates and is accompanied by the production of neurotoxic ROS. In addition, gene mutation, abnormal phosphorylation of tau protein, neuroinflammation, cholinergic injury, and imbalance of neurovascular lesions are also causes of AD. Scutellarin binds to Aβ-42 receptors in the brain, effectively inhibits the generation of Aβ oligomers and fibers, attenuates its induced neurotoxicity and reduces the expression of phosphorylated Tau protein, increases the expression levels of superoxide dismutase and acetylcholine, inhibits the expression levels of ROS and pro-inflammatory factors TNF-α and IL-6, and attenuates neuroinflammation. It also antagonizes Aβ-induced expression of anti-apoptotic protein Bcl2, inhibits expression of pro-apoptotic protein Bax and cleaved caspase 3, reduces apoptosis, and alleviates AD [70–73]. Defective mitochondrial bioenergetics and its resulting low glucose metabolism are key pathophysiologic regulators that promote neurodegeneration, Sheng et al. [74] found that scutellarin rescue mitochondrial damage by improving mitochondrial glucose oxidation via the Pdk-Pdc axis and that active components that ameliorate mitochondrial bioenergetic deficiencies may be valuable in the treatment of neurological disorders. Microglia are essential for the development and homeostasis of the neonatal central nervous system (CNS). Types of action and models of scutellarin in the treatment of Alzheimer’s diseases are showed in Table 6.
Types of action and models of scutellarin in Alzheimer’s disease
2.6 Anti-inflammatory effect
As a natural small molecule, scutellarin has good anti-inflammatory activity and can be used in the prevention and treatment of pneumonia, arthritis, and neuroinflammation. scutellarin can inhibit the inflammatory response by modulating the NF-ĸb/NLRP3 pathway, which exerts an antagonistic effect [75]. Lipopolysaccharide (LPS) is a common inflammatory factor that activates the inflammatory sensory protein caspase-11 and produces an inflammatory response. Scutellarin induces Ser/Thr phosphorylation of caspase-11 at PKA-specific sites, which counteracts the activation of caspase11 and antagonizes the inflammatory response caused by LPS [76]. Cerebrovascular diseases are often accompanied by neuroinflammation, which can lead to increased morbidity and mortality. In the central nervous system, microglia are resident innate immune cells Neuroinflammation is regulated by microglia, which play a dual role in the developing brain, both neuroprotective and neurotoxic. Activated microglia release inflammatory factors such as TNF-α, IL-1β, and NO, which further stimulate microglia activation and promote the accumulation of pro-inflammatory mediators, ultimately leading to neuronal death and exacerbating brain damage. Scutellarin can inhibit the production of inflammatory factors by regulating the AKT/NF-κB and p38/JNK pathways, which in turn inhibits microglia activation to alleviate neuroinflammation [77]. In addition, it has been shown that scutellarin can also alleviate and treat osteoarthritis by modulating the NF-ĸB pathway [78]. Yang et al. [79] found that scutellarin significantly reduced subchondral bone loss and cartilage degeneration in a mouse model of cartilage injury in medial meniscus (DMM) destabilization and in ovariectomy (OVX)-induced mouse subchondral bone loss. By inhibiting interleukin 1β-induced extracellular matrix degradation of cartilage NF-κB/mitogen-activated protein kinase (NF-κB/MAPK) signaling pathway. Li et al. [80] found that scutellarin attenuated complete Freund’s adjuvant (CFA)-induced rheumatoid arthritis (RA) in mice by modulating the Keap1/Nrf2/HO-1 pathway, and the results provide preliminary evidence for the treatment of arthritis with Scutellarin. Ulcerative colitis (UC) is an inflammatory bowel disease of unknown etiology that lacks effective treatments, Aksit et al. [81] found that scutellarin may prevent UC by downregulating pro-inflammatory cytokines and inhibiting apoptosis and oxidative stress. Types of action and models of scutellarin in anti-inflammatory effects are shown in Table 7.
Types of action and models of scutellarin in anti-inflammatory and antioxidant effect
2.7 Antioxidant effect
The presence of phenolic hydroxyl groups in the chemical structure of scutellarin provides hydrogen atoms to exert antioxidant effects. Scutellarin can effectively scavenge a variety of free radicals such as 1,1-diphenyl-2-trinitrophenylhydrazine (DPPH), 2,2ʹ-biamine-bis-(3-ethylbenzothiazoline-6-sulfonic acid) (ABTS+), and superoxide anion (O2–), and mitigate the damage caused by the accumulation of free radicals on the body [82]. Hu et al. found that scutellarin could antagonize the effects of H2O2-induced damage to the retina in the mouse retina by culturing H2O2-induced damage to the retina in the mouse retina cells (APRE-19), and after administration of scutellarin, they found that it could antagonize the H2O2-induced increase in BAX expression and decrease in bcl-2 expression, which in turn decreased the expression of ROS, MDA, SOD, and GSH, reduced oxidative damage, and increased the survival rate of APRE-19 [83]. Types of action and models of scutellarin in antioxidan effect is shown in Table 7.
2.8 Antiviral effect
Modern studies have shown that scutellarin has some antiviral activity. Its antiviral pharmacological action is a specific manifestation of the purgative and detoxifying action in classical Chinese medicine [84]. Details of scutellarin’s antiviral activity were reported as research progressed. Wang et al. [85] found that scutellarin significantly inhibited the activities of sortase A (SrtA) and caseinolytic peptidase P (ClpP) of methicillin-resistant Staphylococcus aureus (MRSA) strain USA300 by screening hundreds of compounds, fluorescence quenching assay and molecular docking results showed that scutellarin directly binds to SrtA molecules, and also inhibits hemolytic activity of Staphylococcus aureus (SA) by inhibiting Hla expression in a SrtA-independent way. It can also inhibit the hemolytic activity of SrtA by suppressing the expression of Hla in a SrtA-independent manner. Therefore, the combination of scutellarin with vancomycin has the effect of preventing MRSA invasion of A549 cells and pneumonia in mice.
2.9 Protect the liver and kidney
Scutellarin may be a promising drug for the prevention of liver and renal injury. Miao et al. [86] established a model of CCL4-induced hepatic injury in mice and found that scutellarin exerted potential CCl4-induced hepatic injury by inhibiting the CYP2E1 and IĸBα/NF-ĸB pathways, modulating the intestinal microbiota, and endogenous metabolites involved in lipid metabolism and bile acid homeostasis, and exerting potential hepatoprotective effects. Scutellarin can play a protective role in renal protection. Dai et al. found that Scutellarin activated Nrf2 signaling protects the kidney from ischemia/reperfusion-induced oxidative damage by reducing inflammatory factors through up-regulation of the HO-1 pathway as revealed in vivo and in vitro experiments [87]. Acute renal injury (AKI) has a high mortality and morbidity. The oxidative stress induced in the kidneys after acute and excessive alcohol intake leads to acute kidney injury (AKI), resulting in causing severe swelling and damage groups of tubular epithelial cells with glomerular atrophy, necrosis, and inflammatory infiltration. Yang et al. found that langoustine exerts a protective effect against AKI through anti-inflammation and antioxidant activity [88]. Shahmohammadi et al. found that scutellarin can inhibit acute renal injury induced by regulating Nrf2/PPAR-c/PGC-1a/NF-kB/TLR4 [89].
2.10 Other effects
Scutellarin also has pharmacological activities such as treatment of glaucoma, liver protection, kidney protection, and hyperuricemia. Zhu et al. established a mouse model of glaucoma and found that scutellarin could maintain the retinal structure and visual function of mice when intraocular pressure was elevated, suggesting that scutellarin is a potentially novel neurotherapeutic agent used in the treatment of glaucoma [90]. Li et al. found that scutellarin reduced renal injury and lowered the glomerular filtration rate in hyperuricemic mice (HN), which may be alleviated by a regulatory mechanism of extracellular cellular communication network factor 1 (CCN1) on the activation of NLRP3 inflammatory vesicles [91]. Duan et al. found that scutellarin inhibited the onset and duration of convulsions and reduced the severity of PTZ-induced seizures in mice by modulating changes in the levels of gamma-aminobutyric acid (GABA), glutamate, and dopamine, as well as the activities of Ca2+ ATPase and Na+ K+ ATPase [92]. Types of action and models of scutellarin in other effects are shown in Table 8.
Types of action and models of scutellarin in other effects
3 Conclusion
Scutellarin is a slightly toxic or non-toxic natural small-molecule flavone compound with good effects against cardiovascular and cerebrovascular diseases, anti-tumor, anti-insulin resistance, anti-virus, anti-diabetic complications, anti-Alzheimer’s disease, liver and renal protection, with a complex mechanism of action involving numerous targets and signaling pathways, and scutellarin exerts these therapeutic effects mainly related to its anti-inflammatory, antioxidant, apoptosis-regulating, and vasodilating effects, but the current study was not specific enough and in-depth enough to explain the link between each target, pathway, and disease as a whole, and was unable to connect them to form a holistic mechanistic network, which requires a more in-depth study [93]. In addition, through the collection of animal or cell models in the article, it is found that most experimental results are only preliminary results, and most results lack positive control, which is a lack of reference for the clinical application of candidate drugs. Commonly used drugs, oral and intravenous injections in the formulations based on scutellarin are the mainstream of the current formulation research, among which the injectable products include breviscapine injection, Deng zhan hua Injection, breviscapine sodium chloride injection, breviscapine dextrose injection, the first two of which are more widely used in clinical applications [94].
It has been proved that scutellarin can be used in combination with other drugs to enhance therapeutic efficacy. Therefore, combining scutellarin with other drugs has a promising application prospect. Cocrystallization and nanoformulation technology occupy an important proportion in new drug development, and co-crystallization of scutellarin with other drugs for combination therapy may be a potential way of new drug development. In addition, cocrystallization and nanoformulation can also help to improve the problems of poor stability, poor water solubility, low oral bioavailability, and short in vivo half-life of scutellarin, which has a good prospect for research and development.
As a natural small molecule, scutellarin has good prospects for clinical application and is a potential therapeutic agent for tumors, atherosclerosis, cardiac and cerebral ischemic injuries, diabetic microangiopathy, hyperuricemia, and anti-Alzheimer’s disease, etc. However, the current study is not deep enough, and more pharmacological mechanisms of action need to be further explored. Network pharmacology is an interdisciplinary subject between bioinformatics and pharmacology. With the breakthrough of artificial intelligence and other fields, it can better improve the efficiency of research and provide support for the mechanism exploration of candidate natural small molecules.
Notes
Acknowledgements
The authors are thankful to National Science Foundation of China (Grant No.22278443), the Key R&D Program of Shan Dong Province (Grant No. 2021ZDSYS26), CAMS Innovation Fund for Medical Sciences (Grant No. 2022-I2M-1-015), Chinese Pharmacopoeia Commission Drug Standard Promoting Fund (Grant No. 2023Y11), Inde-pendent Innovation and Achievement Transformation Plan Project of Zaozhuang City (Grant No. 2202GH15), the Xinjiang Uygur Autonomous Region Innovation Environment Construction Special Fund and Technology Innovation Base Construction Key Laboratory Open Project (Grant No. 2022D04016), National Natural Science Foundation of China (Grant No. 882141204), and CAMS Innovation Fund for Medical Sciences (Grant No. 2022-I2M-1-005) for financial support. Fig. 2 was created with BioRender.com.
Author contributions
Conceptualization and study design: LZ, YL, GD and YX; literature review and collection: YX, GS, YT and SY; writing—original draft preparation: YX, GS, YT, WZ; figures and tables: YX, GS; review and editing: YX, WZ, LZ, YL and GD. All authors have read and agreed to the published version of the manuscript. The author(s) read and approved the final manuscript.
Funding
This funding was supported by National Science Foundation of China (22278443); the Key R&D Program of Shan Dong Province (2021ZDSYS26); Chinese Academy of Medical Sciences Initiative for Innovative Medicine (2022-I2M-1-015, 2022-I2M-1-005);Chinese Pharmacopoeia Commission Drug Standard Promoting Fund (2023Y11); Jiangsu Provincial Agricultural Science and Technology Independent Innovation Fund (2202GH15); Special Fund for Scientific Innovation Strategy-Construction of High-level Academy of Agriculture Science (2022D04016); National Natural Science Foundation of China (882141204).
Availability of data and materials
The data supporting the findings of this study are available upon reasonable request from the corresponding author.
Declarations
Competing interests
The authors declare that they have no conflict of interest.
References
-
1.Qu J, Wang Y, Luo G. Determination of scutellarin in Erigeron breviscapus extract by liquid chromatography-tandem mass spectrometry. J Chromatogr A. 2001;919(2): 437-41. CrossRef PubMed Google Scholar
-
2.Malikov V, Yuldashev M. Phenolic compounds of plants of the Scutellaria Genus. Distribution, structure, and properties. Chem Nat Compd. 2002;38(5): 473-519. CrossRef PubMed Google Scholar
-
3.Xin C, Su Y, Guo L, et al. Phenolic constituents from Conyza sumatrensis. Biochem Syst Ecol. 2008;36(3): 216-8. CrossRef PubMed Google Scholar
-
4.Formisano C, Rigano D, et al. Flavonoids in Subtribe Centaureinae (Cass) Dumort (Tribe Cardueae, Asteraceae): distribution and13C-NMR Spectral Data. Chem Biodivers. 2012;9: 2096-158. CrossRef PubMed Google Scholar
-
5.Hua Y, Wang H. Chemical Components of Anaphalis sinica Hance. J Chin Chem Soc-Taip. 2004;51(2): 409-15. CrossRef PubMed Google Scholar
-
6.Hasibuan P, Harahap U, Sitorus P, et al. The anticancer activities of Vernonia amygdalina Delile. Leaves on 4T1 breast cancer cells through phosphoinositide 3-kinase (PI3K) pathway. Heliyon. 2020;6(7): e04449. CrossRef PubMed Google Scholar
-
7.Liu C, Gao M, Guo B. Plant regeneration of Erigeron breviscapus (vant.) Hand. Mazz. and its chromatographic fingerprint analysis for quality control. Plant Cell Rep. 2008;27(1): 39-45. CrossRef PubMed Google Scholar
-
8.Wang A, Cheng G. Determination of Scutellarin in Herba scutellariae Barbata by HPLC. Guangzhou Chem Ind. 2017;45(07): 94–5+113. PubMed Google Scholar
-
9.Hong C, Chen J, Lu M, et al. Simultaneous determination of scutellarin and baicalin in the flowers of Scutellaria Baicalensis Georgi by HPLC. Chin J Mod Appl Pharm. 2020;37(11): 1320-3. PubMed Google Scholar
-
10.Hu Y, Zhang H, Zhang Z. Determination flavonoids and scutellarin in herbs of Erigeron genu. Chin J Pharm Ana. 2005;25(01): 21-3. PubMed Google Scholar
-
11.Liu H, Liu B, Wang G, et al. Studies on the chemical constituents from Conyza canadensis. Chin Med Mat. 2011;34(05): 718-20. PubMed Google Scholar
-
12.Fan S, Sui H, Chen X, et al. Determination of phenolic parts in Thymusquinquecostatus Celak by HPLC and UV-Vis. J Beijing Univ TCM. 2019;42(10): 854-61. PubMed Google Scholar
-
13.Gaihre Y, Tsuge K, Hamajima H, et al. The contents of polyphenols in Perilla frutescens (L.) Britton var frutescens (Egoma) leaves are determined by vegetative stage, spatial leaf position, and timing of harvesting during the day. J Oleo Sci. 2021;70(6): 855-59. CrossRef PubMed Google Scholar
-
14.Cattaneo L, Cicconi R, Mignogna G, et al. Anti-proliferative effect of Rosmarinus officinalis L. extract on human melanoma A375 cells. PLoS ONE. 2015;10(7): e0132439. CrossRef PubMed Google Scholar
-
15.Pisarev D, Novikov O, Novikova M, et al. Flavonoid composition of Juniperus oblonga Bieb. Bull Exp Biol Med. 2011;150(6): 714-7. CrossRef PubMed Google Scholar
-
16.Han X, Wang S, Yang X, et al. Analysis of plasma migration components in Patrinia villosa (Thunb.) Juss. effective parts by UPLC-Q-TOF-MS. Biomed Chromatogr. 2020;34(1): e4701. CrossRef PubMed Google Scholar
-
17.Wang X, Wei L, Wang L, et al. Scutellarin potentiates vancomycin against lethal pneumonia caused by methicillin-resistant Staphylococcus aureus through dual inhibition of sortase A and caseinolytic peptidase P. Biochem Pharmacol. 2022;199: 114982. CrossRef PubMed Google Scholar
-
18.Fang H, Zhao X, Zhang M, et al. Beneficial effects of flavonoids on cardiovascular diseases by influencing NLRP3 inflammasome. Inflammopharmacology. 2023;31: 1-15. CrossRef PubMed Google Scholar
-
19.Xu H, Wang E, Chen F, et al. Neuroprotective phytochemicals in experimental ischemic stroke: mechanisms and potential clinical applications. Oxid Med Cell Longev. 2021;2021: 1-45. PubMed Google Scholar
-
20.Bangar A, Khan H, Kaur A, et al. Understanding mechanistic aspect of the therapeutic role of herbal agents on neuroplasticity in cerebral ischemic-reperfusion injury. J Ethnopharmacol. 2023, 117153. PubMed Google Scholar
-
21.Tuli H, Bhushan S, Kumar A, et al. Autophagy Induction by Scutellaria Flavones in Cancer: Recent Advances. Pharmaceuticals. 2023;16(2): 302. CrossRef PubMed Google Scholar
-
22.Subedi L, Gaire B. Phytochemicals as regulators of microglia/macrophages activation in cerebral ischemia. Pharmacol Res. 2021;165: 105419. CrossRef PubMed Google Scholar
-
23.Chen H, Jia W, Li H, et al. Scutellarin exerts anti-inflammatory effects in activated microglia/brain macrophage in cerebral ischemia and in activated BV-2 microglia through regulation of MAPKs signaling pathway. Neuromolecular Med. 2020;22(2): 264-77. CrossRef PubMed Google Scholar
-
24.Niu R, Xiong L, Zhou H, et al. Scutellarin ameliorates neonatal hypoxic-ischemic encephalopathy associated with GAP43-dependent signaling pathway. Chin Med. 2021;16(1): 105. CrossRef PubMed Google Scholar
-
25.Hung Y, Liu Y, Wu B, et al. Cinaciguat prevents postnatal closure of ductus arteriosus by vasodilation and anti-remodeling in neonatal rats. Front Physiol. 2021;12: 661171. CrossRef PubMed Google Scholar
-
26.Lorigo M, Quintaneiro C, Maia C, et al. UV-B filter octylmethoxycinnamate impaired the main vasorelaxant mechanism of humanumbilical artery. Chemosphere. 2021;277: 130302. CrossRef PubMed Google Scholar
-
27.Abdallah H, Hassan N, El-Halawany A, et al. Major flavonoids from Psiadia punctulata produce vasodilation via activation of endothelial dependent NO signaling. J Adv Res. 2020;24: 273-9. CrossRef PubMed Google Scholar
-
28.Shen Z, Zhang Z, Wang X, et al. VEGFB-VEGFR1 ameliorates Ang II-induced cardiomyocyte hypertrophy through Ca2+-mediated PKG I pathway. J Cell Biochem. 2018;119(2): 1511-20. CrossRef PubMed Google Scholar
-
29.Chen Y, Chen C, Li M, et al. Scutellarin reduces cerebral ischemia reperfusion injury involving in vascular endothelium protection and PKG signal. Nat Prod Bioprospect. 2021;11(6): 659-70. CrossRef PubMed Google Scholar
-
30.Deng M, Sun J, Peng L, et al. Scutellarin acts on the AR-NOX axis to remediate oxidative stress injury in a mouse model of cerebral ischemia/reperfusion injury. Phytomedicine. 2022;103: 154214. CrossRef PubMed Google Scholar
-
31.Meng Z, Wu J, Zhu Y, et al. Revealing the common mechanisms of scutellarin in angina pectoris and ischemic stroke treatment via a network pharmacology Approach. Chin J Integr Med. 2021;27(1): 62-9. CrossRef PubMed Google Scholar
-
32.Jia Q, Chen H, Qi Z, et al. Network pharmacology to explore the mechanism of scutellarin in the treatment of brain ischaemia and experimental verification of JAK2/STAT3 signalling pathway. Sci Rep-Uk. 2023;13(1): 1-11. CrossRef PubMed Google Scholar
-
33.Xie X, Wang F, Ge W, et al. Scutellarin attenuates oxidative stress and neuroinflammation in cerebral ischemia/reperfusion injury through PI3K/Akt-mediated Nrf2 signaling pathways. Eur J Pharmacol. 2023;957: 175979. CrossRef PubMed Google Scholar
-
34.Zhang Y, Zhang Z, Wang J, et al. Scutellarin alleviates cerebral ischemia/reperfusion by suppressing oxidative stress and inflammatory responses via MAPK/NF‐κB pathways in rats. Environ Toxicol. 2022;37(12): 2889-96. CrossRef PubMed Google Scholar
-
35.Wang C, Liu Y, Liu X, et al. Scutellarin alleviates ischemic brain injury in the acute phase by affecting the activity of neurotransmitters in neurons. Molecules. 2023;28(7): 3181. CrossRef PubMed Google Scholar
-
36.Chen H, Yang L, Zhang X, et al. Scutellarin acts via MAPKs pathway to promote M2 polarization of microglial cells. Mol Neurobiol. 2023;60(8): 4304-23. CrossRef PubMed Google Scholar
-
37.Zhang T, Wang K, Fan H, et al. Ameliorative effect of scutellarin on acute alcohol brain injury in mice. J Zhejiang Univ-Sc B. 2022;23(3): 258-64. CrossRef PubMed Google Scholar
-
38.Li J, Song Z , Hou X. Scutellarin ameliorates ischemia/reperfusion injury induced cardiomyocyte apoptosis and cardiac dysfunction via inhibition of the cGAS STING pathway. Exp Ther Med. 2023;25(4): 1-9. CrossRef PubMed Google Scholar
-
39.Zhou L, Han Y, Yang Q, et al. Scutellarin attenuates doxorubicin-induced oxidative stress, DNA damage, mitochondrial dysfunction, apoptosis and autophagy in H9c2 cells, cardiac fibroblasts and HUVECs. Toxicol In Vitro. 2022;82: 105366. CrossRef PubMed Google Scholar
-
40.Wang W, Liu X, Ding Y, et al. Scutellarin Protects Myocardial Ischemia-Reperfusion Injury ERK1/2-CREB Regulated Mitophagy. Pharmacogn Mag. 2023, 09731296231199860. PubMed Google Scholar
-
41.Fu Y, Sun S, Sun H, et al. Scutellarin exerts protective effects against atherosclerosis in rats by regulating the Hippo-FOXO3A and PI3K/AKT signaling pathways. J Cell Physiol. 2019;234(10): 18131-45. CrossRef PubMed Google Scholar
-
42.Su Y, Fan X, Li S, et al. Scutellarin Improves Type 2 Diabetic Cardiomyopathy by Regulating Cardiomyocyte Autophagy and Apoptosis. Dis Markers. 2022;2022: 3058354. CrossRef PubMed Google Scholar
-
43.Huo Y, Mijiti A, Cai R, et al. Scutellarin alleviates type 2 diabetes (HFD/low dose STZ)-induced cardiac injury through modulation of oxidative stress, inflammation, apoptosis and fibrosis in mice. Hum Exp Toxicol. 2021;40(12): S460-74. CrossRef PubMed Google Scholar
-
44.Qu D, Feng P, Zhang X, et al. Effects of scutellarin on acute myocardial ischemia/reperfusion injury in isolated rat heart. Eur J Inflamm. 2023;21: 1721727X231192289. CrossRef PubMed Google Scholar
-
45.Yang L, Li Z, Fang J. Scutellarin Alleviates Diabetic Retinopathy via the Suppression of Nucleotide-Binding Oligomerization Domain (NOD)-Like Receptor Pyrin Domain Containing Protein 3 Inflammasome Activation. Curr Eye Res. 2023, 1-8. PubMed Google Scholar
-
46.Zeng S, Chen L, Sun Q, et al. Scutellarin ameliorates colitis-associated colorectal cancer by suppressing Wnt/β-catenin signaling cascade. Eur J Pharmacol. 2021;906: 174253. CrossRef PubMed Google Scholar
-
47.Guo X, Li R, Cui J, et al. Induction of RIPK3/MLKL-mediated necroptosis by Erigeron breviscapus injection exhibits potent antitum or effect. Front Pharmacol. 2023;14: 1219362. CrossRef PubMed Google Scholar
-
48.Zeng S, Tan L, Sun Q, et al. Suppression of colitis-associated colorectal cancer by scutellarin through inhibiting Hedgehog signaling pathway activity. Phytomedicine. 2022;98: 153972. CrossRef PubMed Google Scholar
-
49.Deng W, Han W, Fan T, et al. Scutellarin inhibits human renal cancer cell proliferation and migration via upregulation of PTEN. Bio med Pharmacother. 2018;107: 1505-13. CrossRef PubMed Google Scholar
-
50.Derynck R, Budi E. Specificity, versatility, and control of TGF-β family signaling. Sci Signal. 2019;12(570): eaav5183. CrossRef PubMed Google Scholar
-
51.David C, Massagué J. Contextual determinants of TGFβ action in development, immunity and cancer. Nat Rev Mol Cell Biol. 2018;19(7): 419-35. CrossRef PubMed Google Scholar
-
52.Yao Y, Yuan Y, Lu Z, et al. Effects of Nervilia fordii Extract on Pulmonary Fibrosis Through TGF-β/Smad Signaling Pathway. Front Pharmacol. 2021;12: 659627. CrossRef PubMed Google Scholar
-
53.Zhang G, Chen W, Li X, et al. Scutellarin-induced A549 cell apoptosis depends on activation of the transforming growth factor-β1/smad2/ROS/caspase-3 pathway. Open Life Sci. 2021;16(1): 961-8. CrossRef PubMed Google Scholar
-
54.He G, Xing D, Jin D, et al. Scutellarin improves the radiosensitivity of non-small cell lung cancer cells to iodine-125 seeds via downregulating the AKT/mTOR pathway. Thorac Cancer. 2021;12(17): 2352-9. CrossRef PubMed Google Scholar
-
55.Sun C, Zhu Y, Li X, et al. Scutellarin Increases Cisplatin-Induced Apoptosis and Autophagy to Overcome Cisplatin Resistance in Non-small Cell Lung Cancer via ERK/p53 and c-met/AKT Signaling Pathways. Front Pharmacol. 2018;9: 92. CrossRef PubMed Google Scholar
-
56.Wang F, Bao M, Xu J, et al. Scutellarin inhibits the glioma cell proliferation by downregulating BIRC5 to promote cell apoptosis. J Cell Mol Med. 2023;27(14): 1975-87. CrossRef PubMed Google Scholar
-
57.Du J, Li J, Tan J, et al. Scutellarin inhibits glioma cell proliferation by up-regulating miR-15a expression. Am J Transl Res. 2023;15(3): 2156. PubMed Google Scholar
-
58.Chen Y, Li W. Scutellarin inhibits glioblastoma growth in a dose-dependent manner by suppressing the p63 signaling pathway. Dose-Response. 2023;21(3): 15593258231197101. CrossRef PubMed Google Scholar
-
59.Mei X, Ouyang H, Zhang H, et al. Scutellarin suppresses the metastasis of triple-negative breast cancer via targeting TNFα/TNFR2-RUNX1-triggered G-CSF expression in endothelial cells. Biochem Pharmacol. 2023;217: 115808. CrossRef PubMed Google Scholar
-
60.Mei X, Zhang J, Jia W, et al. Scutellarin suppresses triple-negative breast cancer metastasis by inhibiting TNFα-induced vascular end othelial barrier breakdown. Acta Pharmacol Sin. 2022;43(10): 2666-77. CrossRef PubMed Google Scholar
-
61.Liu F, Zu X, Xie X, et al. Scutellarin Suppresses Patient-Derived Xenograft Tumor Growth by Directly Targeting AKT in Esophageal Squamous Cell Carcinoma. Cancer Prev Res (Phila). 2019;12(12): 849-60. CrossRef PubMed Google Scholar
-
62.Hayashi Y, Maysuo Y, Denda Y, et al. Girdin regulates both migration and angiogenesis in pancreatic cancer cell lines. Oncol Rep. 2023;50(3): 1-14. CrossRef PubMed Google Scholar
-
63.Li L, Zou Y, Wang L, et al. Nanodelivery of scutellarin induces immunogenic cell death for treating hepatocellular carcinoma. Int J Pharmaceut. 2023, 123114. PubMed Google Scholar
-
64.Luan H, Huo Z, Zhao Z, et al. Scutellarin, a modulator of mTOR, attenuates hepatic insulin resistance by regulating hepatocyte lipid metabolism via SREBP‐1c suppression. Phytotherapy research. 2020;34(6): 1455-66. CrossRef PubMed Google Scholar
-
65.Gao L, Tang H, Zeng Q, et al. The anti-insulin resistance effect of scutellarin may be related to antioxidant stress and AMPKα activation in diabetic mice. Obes Res Clin Pract. 2020;14(4): 368-74. CrossRef PubMed Google Scholar
-
66.Xi J, Rong Y, Zhao Z, et al. Scutellarin ameliorates high glucose-induced vascular endothelial cells injury by activating PINK1/Parkin-mediated mitophagy. J Ethnopharmacol. 2021;271: 113855. CrossRef PubMed Google Scholar
-
67.Li N, Guo XL, Xu M, et al. Network pharmacology mechanism of Scutellarin to inhibit RGC pyroptosis in diabetic retinopathy. Sci Rep-Uk. 2023;13(1): 6504. CrossRef PubMed Google Scholar
-
68.Fan X, Wang Y, Li X, et al. Scutellarin alleviates liver injury in type 2 diabetic mellitus by suppressing hepatocyte apoptosis in vitro and in vivo. Chin Herb Med. 2023;15: 542-8. PubMed Google Scholar
-
69.Huang B, Han R, Tan H, et al. Scutellarin ameliorates diabetic nephropathy via TGF-β1 signaling pathway. Biol Pharm Bull. 2023. CrossRef PubMed Google Scholar
-
70.Hu X, Teng S, He J, et al. Pharmacological basis for application of scutellarin in Alzheimer’s disease: antioxidation and antiapoptosis. Mol Med Rep. 2018;18(5): 4289-96. PubMed Google Scholar
-
71.Zeng Y, Cui Y, Gu J, et al. Scutellarin mitigates Aβ-induced neurotoxicity and improves behavior impairments in AD mice. Molecules. 2018;23(4): 869. CrossRef PubMed Google Scholar
-
72.Huang X, Xu Y, Sui X, et al. Scutellarein suppresses Aβ-induced memory impairment via inhibition of the NF-κB pathway in vivo and in vitro. Oncol Lett. 2019;17(6): 5581-9. PubMed Google Scholar
-
73.Shin J, Kweon K, Kim D, et al. Scutellarin ameliorates learning and memory deficit via suppressing β-amyloid formation and microglial activation in rats with chronic cerebral hypoperfusion. Am J Chin Med. 2018;46(6): 1203-23. CrossRef PubMed Google Scholar
-
74.Sheng N, Zhang Z, Zheng H, et al. Scutellarin rescued mitochondrial damage through ameliorating mitochondrial glucose oxidation via the Pdk-Pdc axis. Adv Sci. 2023;10: 2303584. CrossRef PubMed Google Scholar
-
75.Peng L, Wen L, Shi QF, et al. Scutellarin ameliorates pulmonary fibrosis through inhibiting NF-κB/NLRP3-mediated epithelial-mesenchymal transition and inflammation. Cell Death Dis. 2020;11(11): 978. CrossRef PubMed Google Scholar
-
76.Bian H, Wang G, Huang J, et al. Scutellarin protects against lipopolysaccharide-induced behavioral deficits by inhibiting neuroinflammation and microglia activation in rats. Int Immunopharmacol. 2020;88: 106943. CrossRef PubMed Google Scholar
-
77.Ye J, Zeng B, Zhong M, et al. Scutellarin inhibits caspase-11 activation and pyroptosis in macrophages via regulating PKA signaling. Acta Pharm Sin B. 2021;11(1): 112-26. CrossRef PubMed Google Scholar
-
78.Luo Z, Hu Z, Bian Y, et al. Scutellarin attenuates the IL-1β-induced inflammation in mouse chondrocytes and prevents osteoarthritic progression. Front Pharmacol. 2020;11: 107. CrossRef PubMed Google Scholar
-
79.Yang H, Wang Z, Wang L, et al. Scutellarin ameliorates osteoarthritis by protecting chondrocytes and subchondral bone microstructure by inactivating NF-κB/MAPK signal transduction. Biomed Pharmacother. 2022;155: 113781. CrossRef PubMed Google Scholar
-
80.Li J, Wang Q, Zhang X. Scutellarin alleviates complete freund’s adjuvant-induced rheumatoid arthritis in mice by regulating the Keap1/Nrf2/HO-1 pathway. Biocell. 2023;47(6): 1307-16. CrossRef PubMed Google Scholar
-
81.Aksit H, Aksit D, Altun E. Protective effects of scutellarin in experimental colitis in rats. Biotech Histochem. 2023;6(98): 432-44. CrossRef PubMed Google Scholar
-
82.Liu Q, Li X, Ouyang X, et al. Dual effect of glucuronidation of a pyrogallol-type phytophenol antioxidant: a comparison between scutellarein and scutellarin. Molecules. 2018;23(12): 3225. CrossRef PubMed Google Scholar
-
83.Hu X, Wu X, Zhao B, et al. Scutellarin protects human retinal pigment epithelial cells against hydrogen peroxide (H2O2)-induced oxidative damage. Cell Biosci. 2019;9: 12. CrossRef PubMed Google Scholar
-
84.Wang L, Song J, Liu A, et al. Research progress of the antiviral bioactivities of natural flavonoids. Nat Prod Bioprospect. 2020;10: 271-83. CrossRef PubMed Google Scholar
-
85.Wang X, Wei L, Wang L, et al. Scutellarin potentiates vancomycin against lethal pneumonia caused by methicillin-resistant Staphylococcus aureus through dual inhibition of sortase A and caseinolytic peptidase P. Biochem Pharmacol. 2022;199: 114982. CrossRef PubMed Google Scholar
-
86.Miao Z, Lai Y, Zhao Y, et al. Protective property of scutellarin against liver injury induced by carbon tetrachloride in mice. Front Pharmacol. 2021;12: 710692. CrossRef PubMed Google Scholar
-
87.Dai J, Li C, Zhao L, et al. Scutellarin protects the kidney from ischemia/reperfusion injury by targeting Nrf2. Nephrology. 2022;27(8): 690-700. CrossRef PubMed Google Scholar
-
88.Yang Q, Wang Y, Chen H, et al. Protective activities of scutellarin against alcohol-induced acute kidney injury. Chem Biodivers. 2022;19(11): e202200254. CrossRef PubMed Google Scholar
-
89.Shahmohammadi A, Golchoobian R, Mirahmadi S, et al. Scutellarin alleviates lipopolysaccharide-provoked septic nephrotoxicity via attenuation of inflammatory and oxidative events and mitochondrial dysfunction. Immunopharm Immunot. 2023;45(3): 295-303. CrossRef PubMed Google Scholar
-
90.Zhu J, Sainulabdeen A, Akers K, et al. Oral scutellarin treatment ameliorates retinal thinning and visual deficits in experimental glaucoma. Front Med (Lausanne). 2021;8: 681169. CrossRef PubMed Google Scholar
-
91.Li G, Guan C, Xu L, et al. Scutellarin ameliorates renal injury via increasing CCN1 expression and suppressing NLRP3 inflammasome activation in hyperuricemic mice. Front Pharmacol. 2020;11: 584942. CrossRef PubMed Google Scholar
-
92.Duan J, Wang J, Zhao Q, et al. Anti-convulsant effects of scutellarein in a PTZ kindling model in mice. Pharmacogn Mag. 2023. CrossRef PubMed Google Scholar
-
93.Wang L, Ma Q. Clinical benefits and pharmacology of scutellarin: a comprehensive review. Pharmacol Therapeut. 2018;190: 105-27. CrossRef PubMed Google Scholar
-
94.Li X, Sun S, Jiang G. Research progress on quality control of breviscapine in injection form. Mod Chin Med. 2020;22(06): 971-8. PubMed Google Scholar
Copyright information
© The Author(s) 2024
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.