唐菖蒲伯克霍尔德菌(Burkholderia gladioli)是一种革兰染色阴性的非发酵菌,属于假单胞菌属。通常情况下,它是一种条件致病菌,临床感染并不常见。本文报告近期发现的1例以发热为表现的唐菖蒲伯克霍尔德菌感染病例,临床表现与既往报道病例略有不同。并与既往文献分析对比,以期对今后临床工作提供参考。
1 资料与方法 1.1 病例资料男性,43岁,农民,湖北洪湖人。因“间断性发热伴气促、咳嗽、全身关节酸痛2月”入院。患者2月前无诱因出现发热,体温高达41.0 ℃,夜间为主,伴寒战、大汗淋漓,气促,活动后明显,伴咳嗽咳痰,为少量白黏痰,并出现全身关节酸痛,无胸痛心悸,无恶心呕吐,无腹痛腹泻,无尿频尿急尿痛;在当地给予抗感染,头孢哌酮舒巴坦钠针剂3.0 g静滴,tid,治疗5 d,体温可降至正常停药。但10 d后患者发热反复,再次给予头孢哌酮舒巴坦钠针剂3.0 g静滴,tid,治疗5 d,体温可降至正常停药,10余天再次发热,如此反复2次。遂转至我院。起病以来,患者精神、食欲、睡眠随病情进展逐日变差,大小便如常,体力下降,体重下降5 kg。既往史:既往健康。有15年吸烟史,40支/d;15年饮酒史,50 ml/d。体格检查:T 37.2 ℃,P 82次/min,呼吸20次/min,血压100/65 mmHg。神志清楚,自动体位,检查合作。皮肤、巩膜无黄染,咽无充血,扁桃体无肿大。胸骨无叩痛。双肺呼吸音清晰,无干湿性啰音。HR 82次/min,节律齐,心脏各瓣膜区未闻及杂音。腹平软,无压痛及反跳痛,肝脾未扪及肿大。双肾区无叩痛,双下肢无水肿。生理反射存在,病理反射未引出。辅助检查:血常规:WBC 11.74×109/L,NE% 7.9×109/L,NE 67.3%,Eos% 0.10×109/L,Eos 0.6%,RBC 3.97×1012/L,Hb 97.4 g/L,PLT 345×109/L。大便常规:正常。大便隐血:阴性。尿常规正常。肝肾功能、血电解质、血糖:正常值范围。血沉:75 mm/h。凝血功能、D-二聚体:正常。输血前八项:均阴性。降钙素原(PCT):0.18 ng/ml。肌酶谱:正常值范围。抗O(ASO)抗体、类风湿因子、血清抗环瓜氨酸肽抗体、风湿全套、抗中性粒细胞抗体全套、抗心磷脂抗体、血肿瘤标志物全套、抗肾小球基底膜抗体均未见异常。多次痰查抗酸染色:阴性。多次痰培养及血培养:阴性。多种寄生虫抗体检测阴性。PET-CT:右锁骨上区、纵隔及双肺门、腹腔内肝胃间隙、胰腺后、肝门区、胰头旁、肠系膜区、腹膜后腹主动脉旁、左侧髂外血管旁及双侧腹股沟区多发淋巴结,部分肿大,代谢不同程度增高,以上考虑淋巴结炎可能性大。全身骨髓弥漫性代谢增强,考虑反应性改变所致,建议结合骨髓活检。骨髓细胞学及活检未见异常。骨髓培养:唐菖蒲伯克霍尔德菌感染,美罗培南耐药,左氧氟沙星中介,头孢他啶,复方新诺明敏感。联合头孢他啶和复方新诺明治疗,第7天患者体温完全正常,第14天复查血常规、血沉及降钙素原等指标正常,予以出院。半月后患者因发热(T38.5 ℃)再次入院。腹股沟淋巴结活检:慢性炎症改变。组织病原学培养阴性。行鼻窦CT、鼻咽镜检查、支气管镜、心脏彩超、腹部B超、中段尿培养均无异常,其它实验室检查结果基本同前次(PET-CT未复查)。给予联合头孢他啶和复方新诺明治疗2周出院,并院外口服头孢地尼和复方新诺明2周。目前随访2月,患者未发热,无其他不适。
1.2 文献复习利用Pubmed和中国知网(CNKI),以“Burkholderia gladioli”和“唐菖蒲伯克霍尔德菌”为检索词,截止至2017年1月16日,检出具有全文可供分析的中文文献4篇[1-4],英文20篇[5-23]。在此,加入本例数据,综合分析所有数据如下。
2 结果 2.1 患者基本情况分析目前可查询数据统计,结合此文报道的1例患者,唐菖蒲伯克霍尔德菌感染的患病人群中男性38例,女性24例,婴儿103例。发病年龄0-76岁。62例年龄大于1岁的患者中,其中既往健康者6例;肺囊性纤维化患者40例;糖尿病患者8例;慢性肉芽肿病患者4例;其余肝移植患者、重症肌无力患者、腹膜透析患者及艾滋病患者各1例。
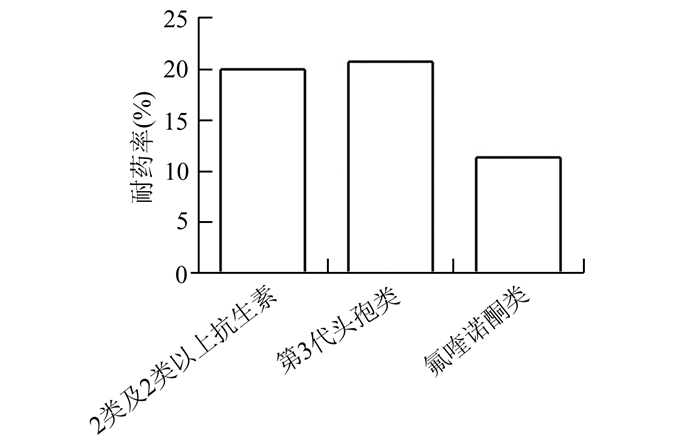
2.2 患者临床特征分析165例患者中,96例(58.18%)患者出现发热,以肺部症状为主要表现的有150例(90.91%),脓肿患者5例(3.03%),骨髓炎患者3例(1.82%),咽部炎症患者4例(2.42%),其他腹膜炎、鼻窦炎、中耳炎、淋巴结炎、颅内感染患者各1例。对致病菌检测,共检出唐菖蒲伯克霍尔德菌176例,其中血培养来源113例(64.20%),痰培养43例(24.43%),各种脓液培养8例(4.55%),胸腹水培养4例(2.27%),骨髓培养3例(1.70%),肺活检组织培养2例,淋巴结组织培养1例,支气管肺泡灌洗液培养1例。针对细菌耐药性分析(具体见图 1)在已知的139例患者中,87例(62.59%)新生儿患者药敏试验提示对所有药物敏感,虽然国内有美罗培南耐药菌株的报道[1, 3],国外尚无发现。已知预后的160例患者中,151例(94.38%)患者经治疗感染控制,但其中有13例(8.13%)患者虽然最终结局良好,治疗过程中却出现病情反复,9例(5.63%)患者死亡。
|
图 1 唐菖蒲伯克霍尔德菌耐药率分析(n=139) |
既往认为唐菖蒲伯克霍尔德菌是一种植物致病菌,导致剑兰、鸢尾花、水稻等植物致病。1989年Christenson等人[24]发现其亦可引起肺囊性纤维化患者呼吸道感染。唐菖蒲伯克霍尔德菌是一种需氧革兰阴性杆菌,它通过产生呼吸道毒素米酵菌酸致病。
既往关于唐菖蒲伯克霍尔德菌感染的病例主要来源于中国、美国、土耳其、新西兰等国家。23篇中18篇均为散发例数报道。
通过文献复习,唐菖蒲伯克霍尔德菌感染有如下特点:几乎是全年龄段感染,但新生儿在感染的年龄段中占一半以上比重(62.80%)。男女比例约为1.65:1。唐菖蒲伯克霍尔德菌作为条件致病菌,主要感染新生儿、肺囊性纤维化病、免疫力低下或受抑制的患者,平时身体健康者极少患病(6例,3.64%)。成人患者中,国外易感人群肺囊性纤维化患者最多见(40/61),而国内艾彪[1]统计34例有基础疾病患者,肾病患者占61.74%(21/34)。国内肺囊性纤维化病发病率低,并且推论主要来自一家医院儿科血培养标本的资料,因此还有待更多病例统计。无论国内外文献报道,感染患者临床表现最常见的均是发热和肺部症状。血培养的检出(64.20%)高于痰培养的检出(24.43%)。这可能还是与患者多为免疫力不全(新生儿)或低下(有基础疾病),致病菌感染后易播散有关。临床多来源的样本检测,如同时查痰、血、分泌物可提高细菌的检出率。虽然感染者多为新生儿或有基础疾病的患者,且多有血行感染,但统计表明预后多较佳,94.38%的患者经治疗感染控制,仅5.63%的患者死亡。细菌耐药率不高,仅20.14%的病株对2类或以上抗生素耐药。而临床常是联合用药,这可能是预后较好的原因。
在我科报道的病例中,还有如下特点值得注意。①患者没有基础疾病,感染唐菖蒲伯克霍尔德菌后,虽然使用了敏感抗生素,但病情反复。既往也有病情迁延的报道[14, 17],但这些病情迁延患者存在基础疾病糖尿病或肺囊性纤维化病。我科病例骨髓感染,可能是病情迁延的原因。这在今后临床工作中值得警惕。②病菌对美罗培南耐药,国内文献报道[1]美罗培南耐药率(1.9%),亚胺培南3.8%。依据药敏结果合理选择抗生素,警惕细菌耐药范围增宽。
| [1] |
艾彪, 周莉, 艾明华, 等. 唐菖蒲伯克霍尔德菌血流感染的诊断与治疗[J].
中华医院感染学杂志, 2015, 25(17): 3856-3858.
Ai B, Zhou L, Ai MH, et al. Laboratory diagnosis and treatment of blood infections caused by Burkholderia gladioli[J]. Chinese Journal of Nosocomiology, 2015, 25(17): 3856-3858. |
| [2] |
肖倩茹, 侯伟伟, 江涟, 等. 胸水中分离唐菖蒲伯克霍尔德菌1株[J].
临床检验杂志, 2013, 31(7): 498.
Xiao QR, Hou WW, Jian L, et al. A case of Burkholderia gladioli from pleural effusion[J]. Chinese Journal of Clinical Laboratory Science, 2013, 31(7): 498. |
| [3] |
黄锐, 王佳. 新生儿病房不常见非发酵菌检出及药物敏感性分析[J].
临床医药实践, 2016, 25(5): 356-358.
Huang R, Wang J. Analysis of the detection and drug sensitivity of the uncommon nonfermenting bacilli in neonatal ward[J]. Proceeding of Clinical Medicine, 2016, 25(5): 356-358. |
| [4] |
陈如寿, 钟佳芳. 唐菖蒲伯克霍尔德菌引起败血症及全身多发脓肿1例[J].
中国保健营养, 2013, 3: 659-660.
Chen RS, Zhong JF. A case report of sepsis and abscess inducing by Burkholderia gladioli[J]. Journal of Chinese Health Care Nutrition, 2013, 3: 659-660. |
| [5] | Zhou F, Ning H, Chen F, et al. Burkholderia gladioli infection isolated from the blood cultures of newborns in the neonatal intensive care unit[J]. Eur J Clin Microbiol Infect Dis, 2015, 34(8): 1533-1537. DOI: 10.1007/s10096-015-2382-1. |
| [6] | Imataki O, Kita N, Nakayama-Imaohji H, et al. Bronchiolitis and bacteraemia caused by Burkholderia gladioli in a non-lung transplantation patient[J]. New Microbes New Infect, 2014, 2(6): 175-176. DOI: 10.1002/nmi2.64. |
| [7] | Tong Y, Dou L, Wang C. Peritonitis due to Burkholderia gladioli[J]. Diagn Microbiol Infect Dis, 2013, 77(2): 174-175. DOI: 10.1016/j.diagmicrobio.2013.06.010. |
| [8] | Dursun A, Zenciroglu A, Karagol BS, et al. Burkholderia gladioli sepsis in newborns[J]. Eur J Pediatr, 2012, 171(10): 1503-1509. DOI: 10.1007/s00431-012-1756-y. |
| [9] | Karagöl BS, Okumuş N, Karada N, et al. Isolated congenital pleural effusion in two neonates[J]. Tuberk Toraks, 2012, 60(1): 52-55. DOI: 10.5578/tt.2984. |
| [10] | Quon BS, Reid JD, Wong P, et al. Burkholderia gladioli-a predictor of poor outcome in cystic fibrosis patients who receive lung transplants? A case of locally invasive rhinosinusitis and persistent bacteremia in a 36-year-old lung transplant recipient with cystic fibrosis[J]. Can Respir J, 2011, 18(4): e64-e65. DOI: 10.1155/2011/304179. |
| [11] | Waseem M, Al-Sherbeeni S, Al-Malki MH, et al. Burkholderia gladioli associated abscess in a type 1 diabetic patient[J]. Saudi Med J, 2008, 29(7): 1048-1050. |
| [12] | Church AC, Sivasothy P, Parmer J, et al. Mediastinal abscess after lung transplantation secondary to Burkholderia gladioli infection[J]. J Heart Lung Transplant, 2009, 28(5): 511-514. DOI: 10.1016/j.healun.2009.01.019. |
| [13] | Lestin F, Kraak R, Podbielski A. Two cases of keratitis and corneal ulcers caused by Burkholderia gladioli[J]. J Clin Microbiol, 2008, 46(7): 2445-2449. DOI: 10.1128/JCM.02442-07. |
| [14] | Kennedy MP, Coakley RD, Donaldson SH, et al. Burkholderia gladioli: five year experience in a cystic fibrosis and lung transplantation center[J]. J Cyst Fibros, 2007, 6(4): 267-273. DOI: 10.1016/j.jcf.2006.10.007. |
| [15] | Boyanton BL Jr, Noroski LM, et al. Burkholderia gladioli osteomyelitis in association with chronic gra- nulomatous disease: case report and review[J]. Pediatr Infect Dis J, 2005, 24(9): 837-839. DOI: 10.1097/01.inf.0000177285.44374.dc. |
| [16] | Ritterband D, Shah M, Cohen K, et al. Burkholderia gladioli keratitis associated with consecutive recurrent endophthalmitis[J]. Cornea, 2002, 21(6): 602-603. DOI: 10.1097/00003226-200208000-00014. |
| [17] | Shin JH, Kim SH, Shin MG, et al. Bacteremia due to Burkholderia gladioli: case report[J]. Clin Infect Dis, 1997, 25(5): 1264-1265. DOI: 10.1086/cid.1997.25.issue-5. |
| [18] | Graves M, Robin T, Chipman AM, et al. Four additional cases of Burkholderia gladioli infection with microbiological correlates and review[J]. Clin Infect Dis, 1997, 25(4): 838-842. DOI: 10.1086/cid.1997.25.issue-4. |
| [19] | Kanj SS, Tapson V, Davis RD, et al. Infections in patients with cystic fibrosis following lung transplantation[J]. Chest, 1997, 112(4): 924-930. DOI: 10.1378/chest.112.4.924. |
| [20] | Wilsher ML, Kolbe J, Morris AJ, et al. Nosocomial acquisition of Burkholderia gladioli in patients with cystic fibrosis[J]. Am J Respir Crit Care Med, 1997, 155(4): 1436-1440. DOI: 10.1164/ajrccm.155.4.9105090. |
| [21] | Hoare S, Cant AJ. Chronic granulomatous disease presenting as severe sepsis due to Burkholderia gla- dioli[J]. Clin Infect Dis, 1996, 23(2): 411. DOI: 10.1093/clinids/23.2.411. |
| [22] | Ross JP, Holland SM, Gill VJ, et al. Severe Burkholderia (Pseudomonas) gladioli infection in chronic granulo- matous disease: report of two successfully treated cases[J]. Clin Infect Dis, 1995, 21(5): 1291-1293. DOI: 10.1093/clinids/21.5.1291. |
| [23] | Khan SU, Gordon SM, Stillwell PC, et al. Empyema and bloodstream infection caused by Burkholderia gladioli in a patient with cystic fibrosis after lung transplantation[J]. Pediatr Infect Dis J, 1996, 15(7): 637-639. DOI: 10.1097/00006454-199607000-00020. |
| [24] | Christenson JC, Welch DF, Mukwaya G, et al. Reco- very of Pseudomonas gladioli from respiratory tract specimens of patients with cystic fibrosis[J]. J Clin Microbiol, 1989, 27(2): 270-273. |
 2018, Vol. 39
2018, Vol. 39

