2. Institute of Geriatrics, Beijing Hospital, National Center of Gerontology, Beijing 100730, China ;
3. Department of Gynecology and Obstetrics, Morin Dawa Daur Autonomous Banner Hospital, Hulunbuir 162850, Inner Mongolia Autonomous Region, China
Objective Abnormal maternal thyroid function is associated with preterm birth. However, this association stays dubious in relevant individual studies for ethnic difference reasons and lack of direct supporting data. This study aimed to evaluate the relationship between preterm birth and thyroid dysfunction or autoimmunity based on ethnic differences.
Methods Relevant studies were identified through searches of MEDLINE, Excerpta Medica, Wan Fang, China Biological Medicine disc, and China National Knowledge Infrastructure from inception to June 15, 2016. Original articles in which an incidence or prevalence of thyroid dysfunction or autoimmunity before second trimester of pregnancy could be extracted were included.
Results Thirty-two unique studies were included for the final meta-analysis. Patients involved were divided into two groups:Group 1 (G1) and Group 2 (G2) comprising of Asian and Caucasian populations, respectively. Positive thyroid antibodies were associated with the occurrence of preterm birth in both G1[odds ratio (OR):3.62, 95% confidence interval (CI):2.83-4.65] and G2 (OR:1.35, 95% CI:1.17-1.56); hypothyroidism, only in G2 (OR:1.20, CI:1.09-1.33); and subclinical hypothyroidism or hypothyroxinemia, in neither group.
Conclusion Thyroid autoimmunity may be a more favorable factor leading to preterm birth among pregnant women of different ethnicities, compared with thyroid dysfunction.
Preterm birth,occurring in 6%-12% of pregnancy,is defined as the birth of a child prior to 37 weeks of gestation[1-2]. It is the leading cause of neonatal mortality,responsible for 75% of neonatal deaths with no congenital anomalie[1-2]. Preterm birth is also associated with perinatal complications,such as congenital neurologic disability,and psychiatric,metabolic,cardiovascular,and renal diseases[1, 3]. To address this problem,numerous works have been conducted over the last decades,yet there is still no great prospect of early prediction and prevention of preterm delivery[4].
As the fetus does not yet produce its own thyroid hormones,adequate functioning of the maternal thyroid is confirmed to be particularly important for the development of the fetal brain during the first trimester[5-6]. Thyroid dysfunction and thyroid autoimmunity are relatively common in women at reproductive age,affecting 2%-3% and 5%-15% of pregnant women,respectively[6, 7]. Both thyroid dysfunction and thyroid autoimmunity are associated with adverse pregnancy outcomes[6-8]. However,over the last 20 years,conflicting results published on alteration of diagnostic criteria of thyroid function tests make the exact prevalence of thyroid diseases in pregnant women and its relationship with preterm labor even more unclear[5, 9-10].
A number of studies have shown that inter-individual differences in thyroid hormone levels may,at least partially,be explained by ethnic background[11-12]. Only a few studies analyzed the ethnic differences of thyroid function tests during pregnancy[13-14]. La'ulu et al.[14-15] and other authors[13, 16] reported that the reference range values for thyroid parameters may differ among Asians,white,black,and Hispanic Americans,and even in different subgroups of Caucasians. These ethnic differences between different populations emphasize the significance of calculating population- specific reference ranges for TSH during pregnancy,suggesting that the risk of preterm birth should be estimated in the same ethnic population. Therefore,this study aimed to conduct a meta-analysis to analyze the risk of preterm birth for pregnant women with thyroid dysfunction or thyroid autoimmunity based on ethnic variety by including data from randomized controlled trials (RCTs) and cohort studies.
Methods Search StrategyRelevant studies were identified through searches of MEDLINE,Excerpta Medica,Wan Fang,China Biological Medicine disc,and China National Knowledge Infrastructure from inception to June 15,2016. Search criteria used were related to thyroid dysfunction,thyroid autoimmunity,and preterm birth. The following search terms were used: subclinical hypothyroidism,hypothyroidism,thyroiditis,thyroid peroxidase,thyrotropin,thyrotropin receptor antibody,thyroid-stimulating immunoglobulin,thyroid microsomal antibodies,thyroid dysfunction,hypothyroxinemia,thyroid diseases,pregnancy,pregnancy outcome,immature and premature labor,premature delivery,preterm birth,cohort analysis,longitudinal study,prospective study,retrospective study,follow up,and case-control study. The language limitation for the initial search was set to include only Chinese and English. RCTs,cohort studies,and case-control studies were included.
Study SelectionThe criteria for inclusion were (1) pregnant women with overt hypothyroidism,subclinical hypothyroidism,hypothyroxinemia,and positive thyroid autoantibody; (2) preterm birth outcome; (3) assessment of thyroid function before second trimester of pregnancy; (4) articles in English or Chinese; and (5) same ethnic population being more than 80% of all patients. The criteria for exclusion were (1) poor quality studies; (2) articles from the same cohort studies (only the newest were included); and (3) subjects with cardiovascular or rheumatic diseases.
Quality EvaluationStudies were judged on scientific quality according to the CONSORT and STROBE statements[17]. Study quality assessment was performed based on the NewcastleOttawa scale for cohort studies[17] (http://www.ohri.ca/programs/clinicalepidemiology/oxford.asp).
Data ExtractionThe procedure was performed independently by two reviewers (L. M,W. FL). Articles included for full text screening were compared during a consensus meeting. In case of disagreement,a third reviewer (W. SW) was consulted for the decision on inclusion or exclusion for full-text evaluation.
Statistical AnalysisIn each study,incidence of thyroid dysfunction or thyroid autoimmunity compared to that of controls was expressed both as odds ratios (OR) with the corresponding 95% confidence intervals (CI). Review Manager software version 5.2 was used to perform the meta-analyses. Statistical heterogeneity was evaluated using the I2 test[17],with I2>50% represents moderate to substantial heterogeneity,in which case random-effects models were used to pool summary estimates[17]. Funnel plots present the publication bias. Begg’s and Egger’s tests were performed to assess publication bias quantitatively. All statistical analyses were conducted using STATA 12.0 software (Stata Corp,College Station,TX,USA). A two-sided P<0.05 was considered statistically significant.
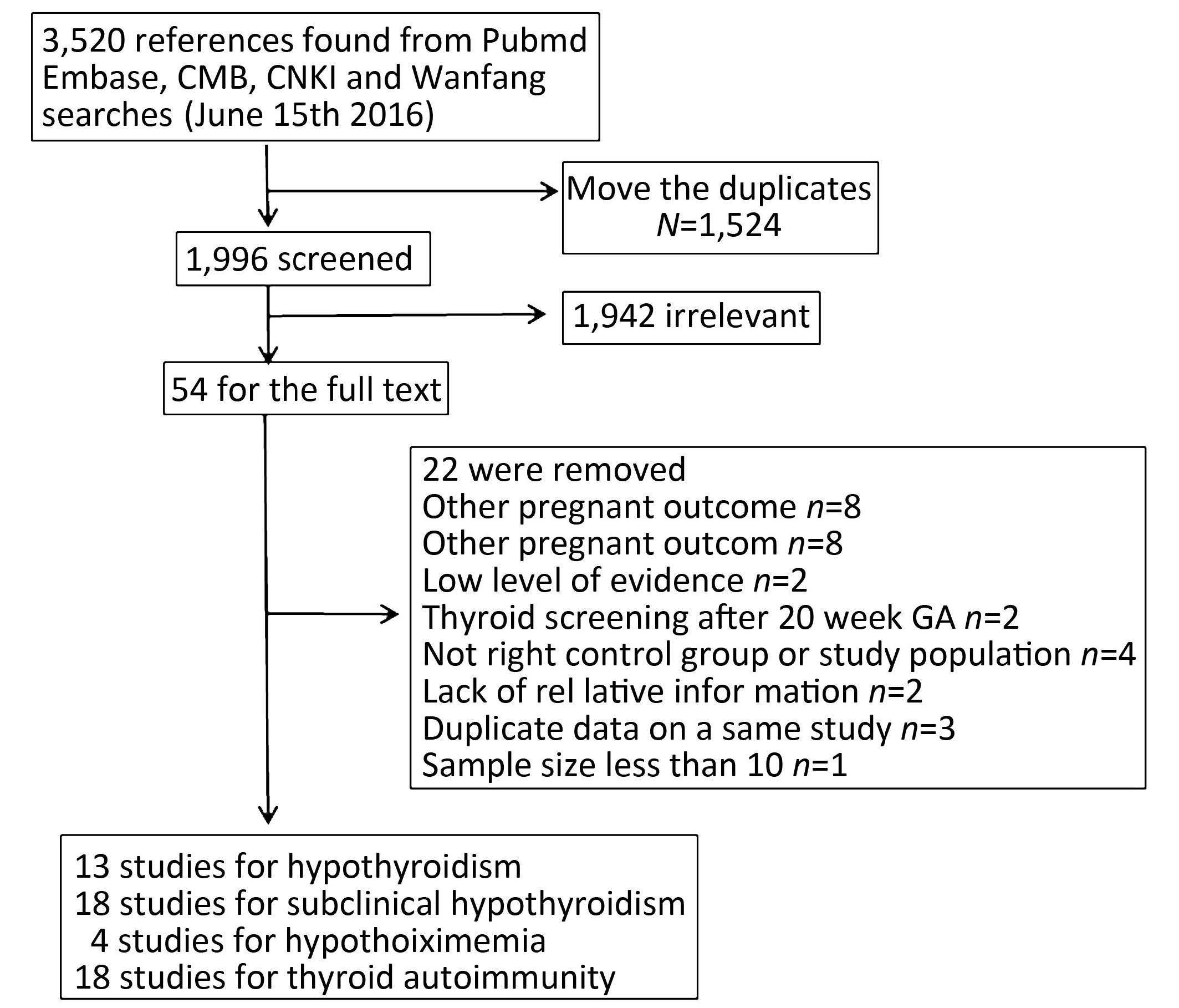
RESULTS Literature SearchA total of 3,520 articles were selected from the search results for critical appraisal. After elimination of duplicate and irrelevant studies,32 unique studies consistent with the inclusion criteria,including 4 Chinese and 28 English,were finally included (Figure 1). Of the 32 articles in this systematic review,13 reported on hypothyroidism[16, 18-26, 31, 33, 41],18 on subclinical hypothyroidism[16, 18-19, 22- 24, 26-34, 46-48],4 on hypothyroxinemia[18, 23, 27, 29],and 18 on thyroid antibodies[16, 18-19, 27, 32, 45]. All 32 cohort studies exhibited low risk of bias for selection and NOS score more than [7] Among these studies,1 article is RCT; 23,prospective cohort studies; 6,retrospective cohort studies,and 2,case-control studies.
|
Download:
|
| Figure 1 Flow chart of literature search and article selection. | |
The characteristics of the articles included are reported in Table 1. The studies were conducted in different ethnicities,such as Caucasians or white,Hispanic,African Americans,and Asians. Given that there were no studies on African American and Hispanic,patients in the involved studies were divided into two groups,namely,Group 1 (G1,Asians) and Group 2 (G2,Caucasians). The size of the cohorts ranged from 306 to 223,512 (total 579,692). There were 42,804 cumulative preterm birth cases.
|
|
Table 1 Characteristics and quality features of the 32 studies included in the systematic review of the association between thyroid dysfunction and preterm birth |
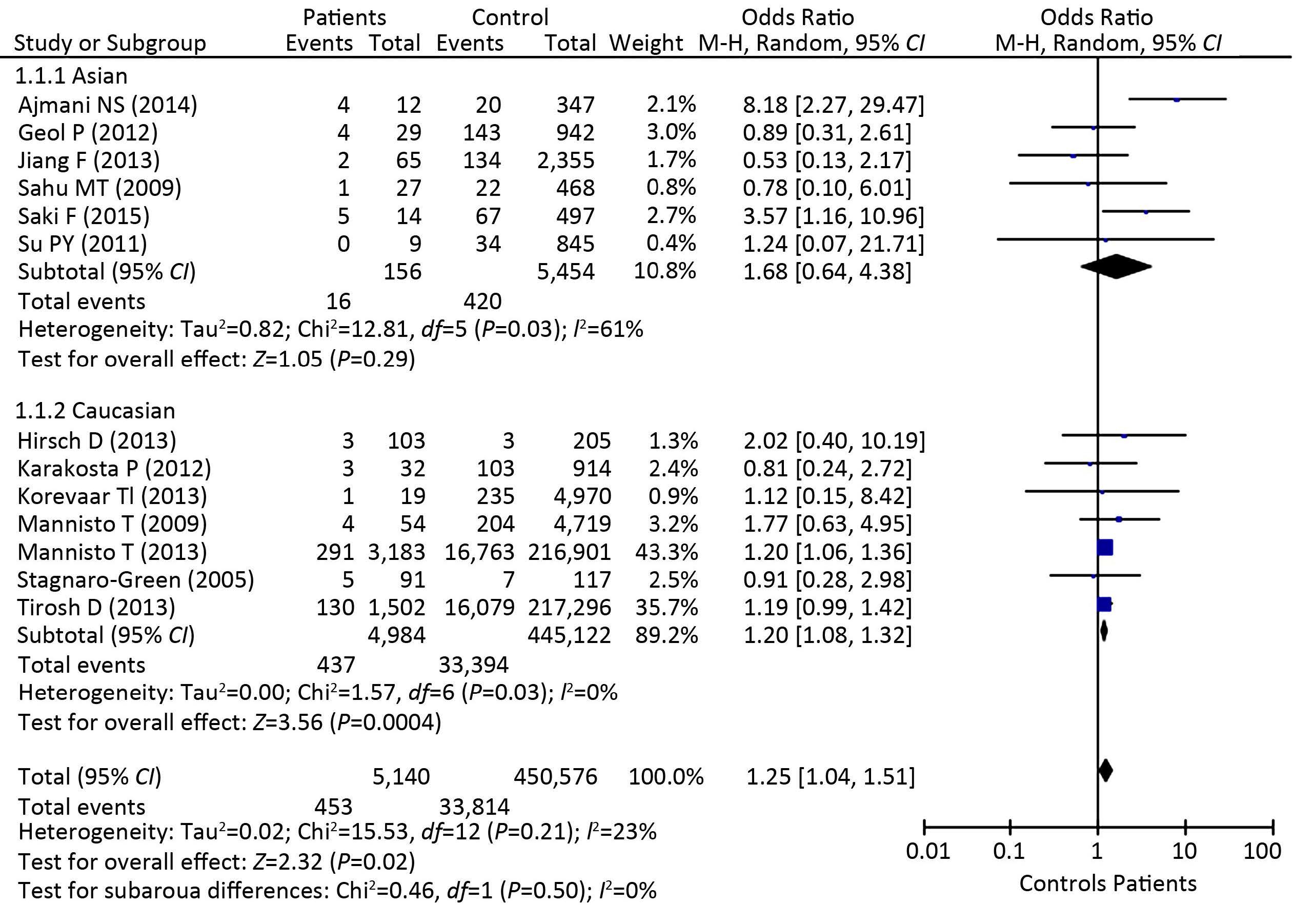
Data from 13 articles reporting 5,140 patients with overt hypothyroidism and 450,576 controls could be included in the meta-analysis and showed an increased risk of preterm delivery (OR: 1.25,95% CI: 1.04-1.51,P=0.02: Figure 2). The study in G2 showed a significant association between overt hypothyroidism and preterm birth (OR: 1.20,95% CI: 1.08-1.32,P=0.0004: Figure 2). By contrast,no significant difference was observed in G1 (OR: 1.68,95% CI: 0.64-4.38,P=0.29: Figure 2).
|
Download:
|
| Figure 2 Forest plot of Odds Ratio’s and 95% Confidence Interval of pooled studies comparing patients with overt hypothyroidism with eythyroid controls according to the risk of preterm birth,37 weeks gestation. Significant association between overt hypothyroidism and preterm birth was observed in Caucasians. | |
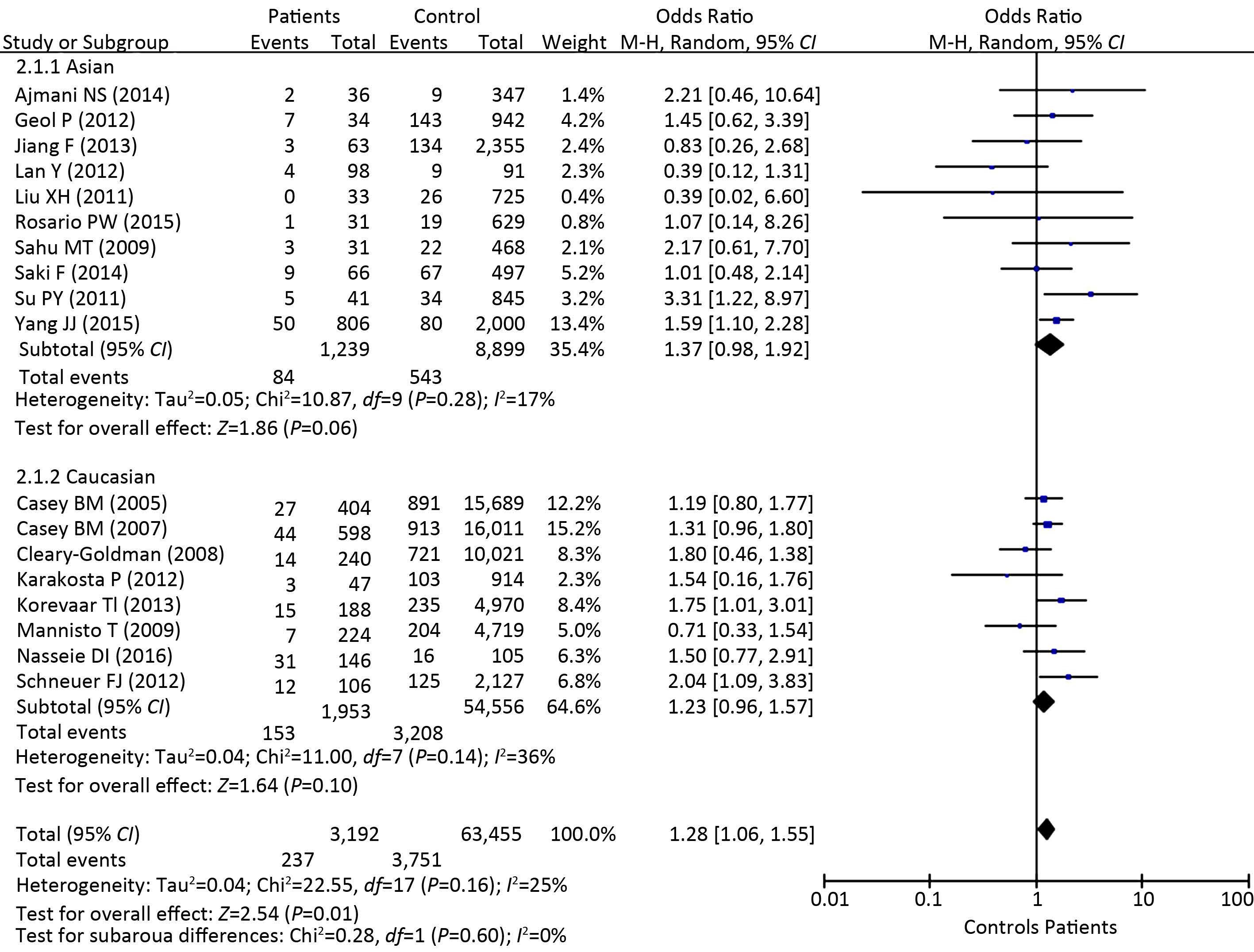
There were 66,647 individual data from 18 studies,including 3,192 pregnant women with subclinical hypothyroidism and 63,455 controls. Difference in the risk of preterm birth was not observed between patients with subclinical hypothyroidism and euthyroid controls in both ethnic groups [G1 (OR: 1.37,95% CI: 0.98-1.92,P=0.06: Figure 3); G2 (OR: 1.23,95% CI: 0.96-1.57,P=0.10: Figure 3)].
|
Download:
|
| Figure 3 Forest plot of Odds Ratio’s and 95% Confidence Interval of pooled studies comparing patients with subclinical hypothyroidism with eythyroid controls according to the risk of preterm birth. No association between subclinical hypothyroidism and preterm birth was observed. | |
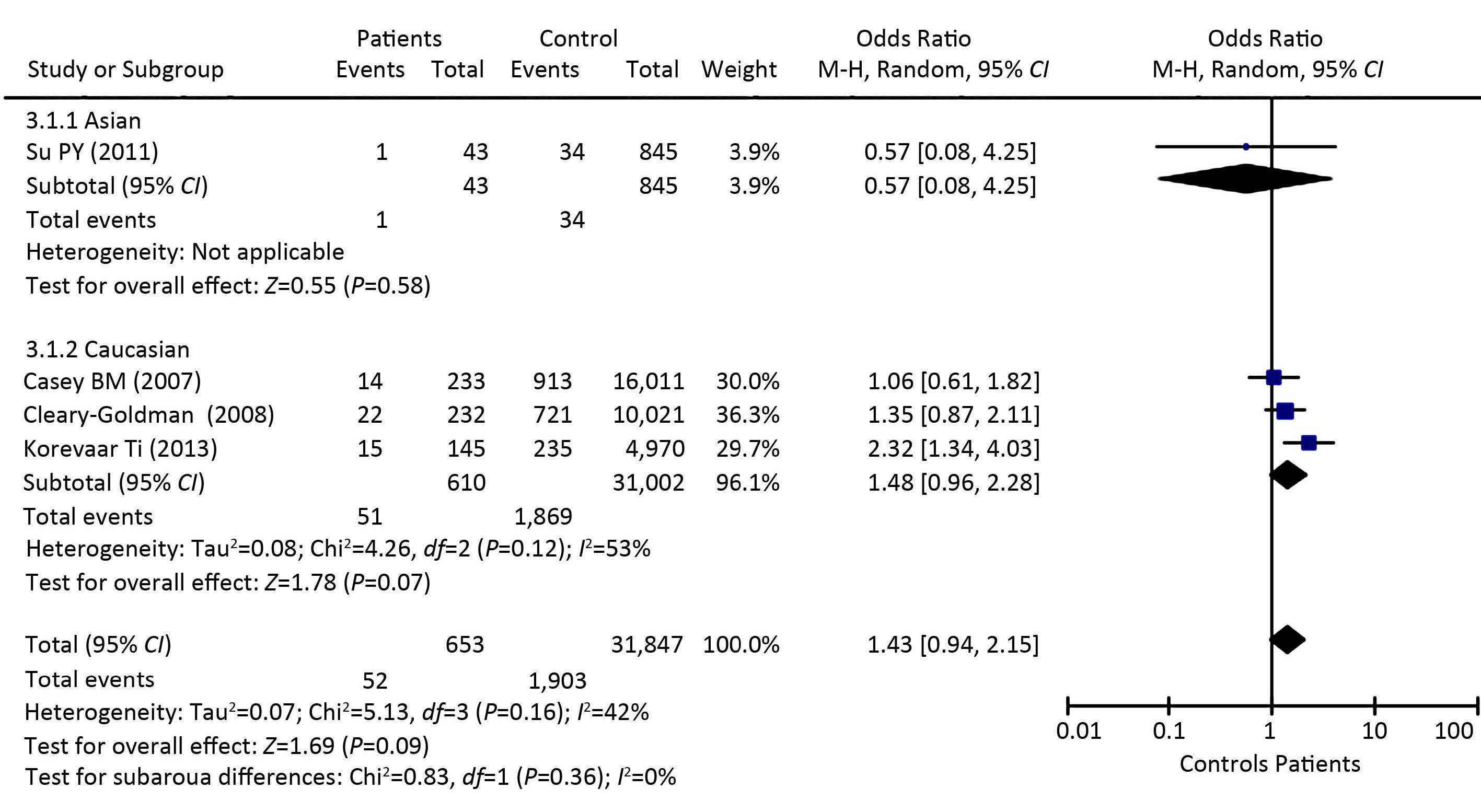
Four studies were investigated for hypothyroxinemia,including 653 pregnant women with hypothyroxinemia and 31,847 controls. The relation between hypothyroxinemia and preterm birth was investigated in one study of G1. The study reported no difference between patients and controls (G1,OR: 0.57,95% CI: 0.08-4.28,P=0.58). Meta-analysis on three studies of G2 resulted in a pooled OR of 1.48 and 95% CI of 0.96-2.28 (P=0.07: Figure 4). No association between hypothyroxinemia and preterm birth was observed in G2.
|
Download:
|
| Figure 4 Forest plot of Odds Ratio’s and 95% Confidence Interval of pooled studies comparing patients with hypothyroxinemia with eythyroid controls according to the risk of preterm birth. No association between hypothyroxinemia and preterm birth was observed. | |
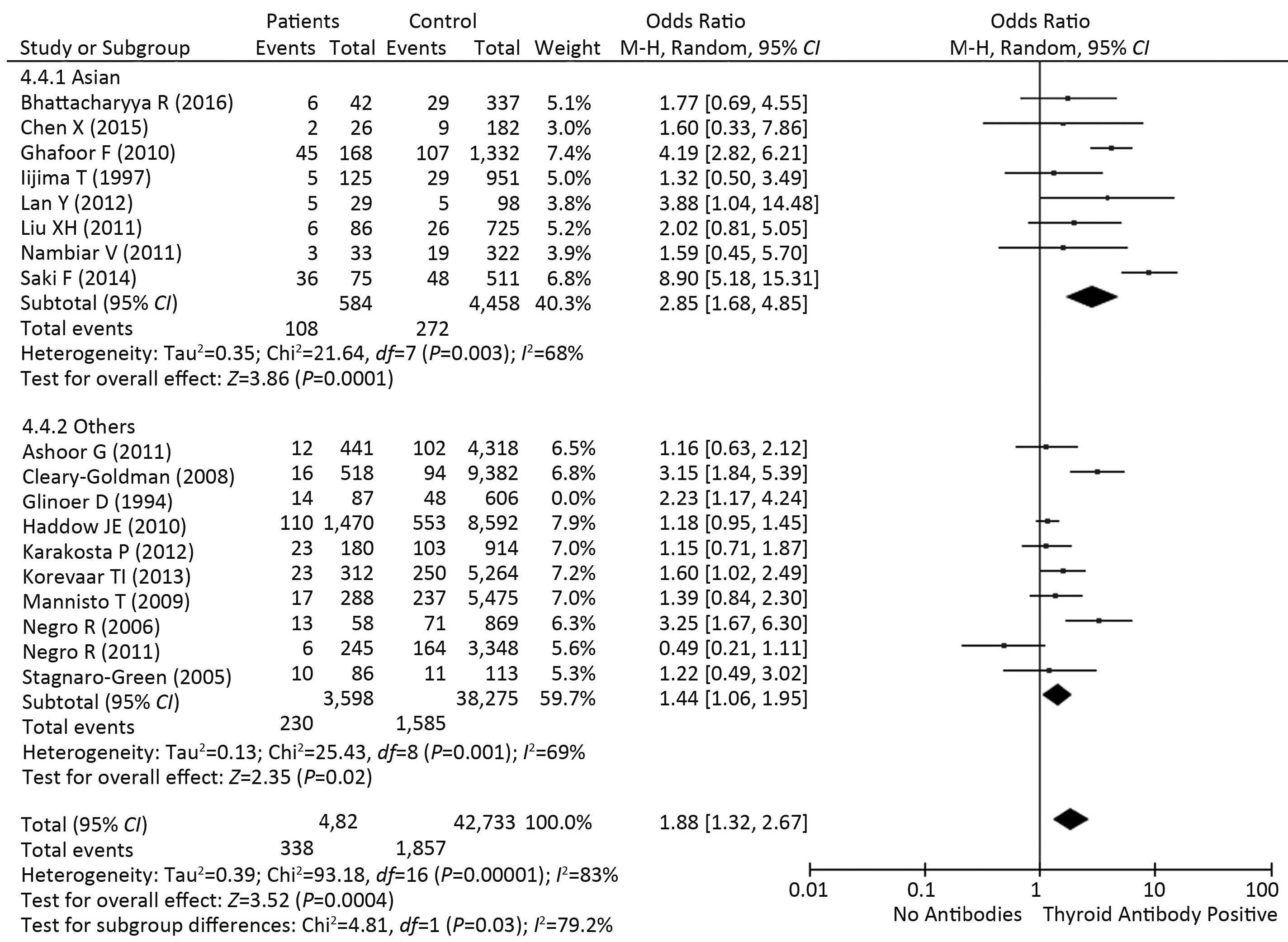
Eighteen studies,including 4,182 pregnant women with positive antibodies and 42,733 healthy controls,were investigated for thyroid autoimmunity. Meta- analysis revealed an increased risk of preterm birth in patients,with positive thyroid antibodies,of both G1 (OR: 2.85,95% CI: 1.68-4.85,P=0.0001: Figure 5) and G2 (OR: 1.44,95% CI: 1.06-1.95,P=0.02: Figure 5).
|
Download:
|
| Figure 5 Forest plot of Odds Ratio’s and 95% Confidence Interval of pooled studies comparing patients euthyroid thyroid antibody positive patients with euthyroid antibody negative controls according to the risk of preterm birth. Positive thyroid antibodies increased the risk of preterm birth in both subgroups. | |
Funnel plots present the publication bias (data not shown). Begg’s and Egger’s tests were performed to assess publication bias quantitatively. No evidence of publication bias was found in the sensitivity testing of every subgroup analysis (Table 2).
|
|
Table 2 Publication bias of Each Subgroup |
The present meta-analysis provides clear evidence for a relationship between the presence of thyroid dysfunction or autoimmunity and preterm birth in different ethnic groups.
The presence of thyroid antibodies was significantly related to the occurrence of preterm birth,compared with the absence of antibodies.
Association between preterm birth and patients with subclinical hypothyroidism or hypothyroixinemia was not observed in both ethnic groups. High TSH level or low free T4 level alone seemed to not necessarily increase the risk of preterm birth. An increased risk of preterm birth was only observed in the other ethnic group with hypothyroidism. No evidence was found for a relationship between hypothyroidism and preterm birth in Asians. Asians were less susceptible to high TSH level,compared with Caucasians. Considering limited data available on preterm birth in Asians with hypothyroxinemia,the role of hypothyroxinemia in preterm delivery needs further investigation.
Positive thyroid antibodies were associated with an increased risk of preterm birth in both ethnic groups. Moreover,preterm delivery may occur more frequently in Asians with positive thyroid antibodies,with a 2.85 fold higher risk. These results showed that thyroid autoimmunity may be a key factor for increased risk of preterm delivery among different ethnicities. Although not all individual studies involved reported this association,meta-analysis was conclusive on this point,showing the additional value of pooled studies compared with individual studies. Several hypotheses exist on the causality between thyroid autoimmunity and obstetric complications. First,thyroid antibodies could be associated with a subtle decrease of thyroid function or might reflect a generalized activation of the immune system and specifically a deregulated activity of the immune system at the fetal-maternal interface[9, 49]. Because pregnancy represents an inflammatory process with a shift in the regulation of cytokine networks within the local placental- decidual environment,a deregulation of the local inflammatory processes can be associated with miscarriage and premature delivery[5, 9, 50]. Supporting our results,a recent meta-analysis showed that maternal thyroid autoimmunity increases by twofold the risk of preterm delivery for women with biochemically normal thyroi d function[49]. Second,the autoimmunity increases the risk of hypothyroidism,owing to the chronic lymphocytic thyroiditis that is associated with the presence of thyroid antibodies. The thyroid then may fail to respond adequately to the increased demand for thyroid hormone during pregnancy. Thus,a high prevalence of thyroid antibodies is reasonable among women with overt or subclinical hypothyroidism (e.g.,25% in Stagnaro-Green et al.[41],32% in Korevaar et al.[18],and 50% in Mannisto[19].
This meta-analysis has several limitations. As previously mentioned,the studies used different inclusion criteria for the patients and different cutoff levels for TSH,fT4,and antibodies (Table 1). This limitation should be considered when using the results for clinical application. Meanwhile,the fact that the diagnoses are made based on ICD-9 coding instead of the specific criteria of blood test results is a limitation of some studies with large sample size[23-24]. Moreover,the differences of the first-time collection of maternal serum samples may partially contribute to the limitations. Although we used random-effects models to perform the meta-analyses of the pooled data in case of heterogeneity while the majority of data showed a very similar trend,some degree of population heterogeneity cannot be excluded. In addition,the affected subjects had a large difference (10.8% vs. 89.2% in weight,and the ORs are 1.68 in Asians and 1.20 in Caucasians); therefore,these differences may be caused by statistical power (Figure 2).
We conclude that pregnant women with hypothyroidism and thyroid autoimmunity may have an increased risk of preterm birth in different ethnic groups. Thyroid autoimmunity may be a more favorable factor leading to preterm birth among pregnant women of different ethnicities,compared with thyroid dysfunction. The association of subgroups of thyroid antibodies with preterm birth should be further investigated in the future studies.
Acknowledgments
The authors thank Prof. LI Hua Tian for her critical revisions during manuscript drafting.
| 1. | Simhan HN, Caritis SN. Prevention of preterm delivery[J]. N Engl J Med , 2007, 57 :477–87. |
| 2. | Muglia LJ, Katz M. The enigma of spontaneous preterm birth[J]. N Engl J Med , 2010, 362 :529–35. doi:10.1056/NEJMra0904308 |
| 3. | Nosarti C, Reichenberg A, Murray RM, et al. Preterm birth and psychiatric disorders in young adult life[J]. Archives of general psychiatry , 2012, 69 :E1–8. |
| 4. | Markham KB, Klebanoff M. Prevention of preterm birth in modern obstetrics[J]. Clinics in perinatology , 2014, 41 :773–85. doi:10.1016/j.clp.2014.08.003 |
| 5. | Stagnaro-Green A. Maternal thyroid disease and preterm delivery[J]. J Clin Endocrinol Metab , 2009, 94 :21–5. doi:10.1210/jc.2008-1288 |
| 6. | van den Boogaard E, Vissenberg R, Land JA, et al. Significance of (sub)clinical thyroid dysfunction and thyroid autoimmunity before conception and in early pregnancy:a systematic review[J]. Human reproduction update , 2011, 17 :605–19. doi:10.1093/humupd/dmr024 |
| 7. | Jouyandeh Z, Hasani-Ranjbar S, Qorbani M, et al. Universal screening versus selective case-based screening for thyroid disorders in pregnancy[J]. Endocrine , 2015, 48 :116–23. doi:10.1007/s12020-014-0385-9 |
| 8. | Abalovich M, Amino N, Barbour LA, et al. Management of thyroid dysfunction during pregnancy and postpartum:an Endocrine Society Clinical Practice Guideline[J]. J Clin Endocrinol Metab , 2007, 92 :S1–47. doi:10.1210/jc.2007-0141 |
| 9. | Stagnaro-Green A, Abalovich M, Alexander E, et al. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum[J]. Thyroid:official journal of the American Thyroid Association , 2011, 21 :1081–125. doi:10.1089/thy.2011.0087 |
| 10. | De Groot L, Abalovich M, Alexander EK, et al. Management of thyroid dysfunction during pregnancy and postpartum:an Endocrine Society clinical practice guideline[J]. The Journal of clinical endocrinology and metabolism , 2012, 97 :2543–65. doi:10.1210/jc.2011-2803 |
| 11. | Boucai L, Surks MI. Reference limits of serum TSH and free T4 are significantly influenced by race and age in an urban outpatient medical practice[J]. Clinical endocrinology , 2009, 70 :788–93. doi:10.1111/cen.2009.70.issue-5 |
| 12. | Price A, Obel O, Cresswell J, et al. Comparison of thyroid function in pregnant and non-pregnant Asian and western Caucasian women[J]. Clinica chimica acta; international journal of clinical chemistry , 2001, 308 :91–8. doi:10.1016/S0009-8981(01)00470-3 |
| 13. | Walker JA, Illions EH, Huddleston JF, et al. Racial comparisons of thyroid function and autoimmunity during pregnancy and the postpartum period[J]. Obstetrics and gynecology , 2005, 106 :1365–71. doi:10.1097/01.AOG.0000185475.61612.ea |
| 14. | La'ulu SL, Roberts WL. Ethnic differences in first-trimester thyroid reference intervals[J]. Clinical chemistry , 2011, 57 :913–5. doi:10.1373/clinchem.2010.161240 |
| 15. | La'ulu SL, Roberts WL. Second-trimester reference intervals for thyroid tests:the role of ethnicity[J]. Clin Chem , 2007, 53 :1658–64. doi:10.1373/clinchem.2007.089680 |
| 16. | Karakosta P, Alegakis D, Georgiou V, et al. Thyroid dysfunction and autoantibodies in early pregnancy are associated with increased risk of gestational diabetes and adverse birth outcomes[J]. J Clin Endocrinol Metab , 2012, 97 :4464–72. doi:10.1210/jc.2012-2540 |
| 17. | Lau J, Joannidis JP, Schimid CH. Quantitative synthesis in systematic reviews[J]. Ann Intern Med , 2009, 127 :820–6. |
| 18. | Korevaar TI, Schalekamp-Timmermans S, de Rijke YB, et al. Hypothyroxinemia and TPO-antibody positivity are risk factors for premature delivery:the generation R study[J]. J Clin Endocrinol Metab , 2013, 98 :4382–90. doi:10.1210/jc.2013-2855 |
| 19. | Mannisto T, Vaarasmaki M, Pouta A, et al. Perinatal outcome of children born to mothers with thyroid dysfunction or antibodies:a prospective population-based cohort study[J]. J Clin Endocrinol Metab , 2009, 94 :772–9. doi:10.1210/jc.2008-1520 |
| 20. | Mannisto T, Mendola P, Grewal J, et al. Thyroid diseases and adverse pregnancy outcomes in a contemporary US cohort[J]. J Clin Endocrinol Metab , 2013, 98 :2725–33. doi:10.1210/jc.2012-4233 |
| 21. | Tirosh D, Benshalom-Tirosh N, Novack L, et al. Hypothyroidism and diabetes mellitus-a risky dual gestational endocrinopathy[J]. Peer J , 2013, 1 :e52. doi:10.7717/peerj.52 |
| 22. | Goel P, Kaur J, Saha PK, et al. Prevalence, associated risk factors and effects of hypothyroidism in pregnancy:a study from north India[J]. Gynecol Obstet Invest , 2012, 74 :89–94. doi:10.1159/000337715 |
| 23. | Su PY, Huang K, Hao JH, et al. Maternal thyroid function in the first twenty weeks of pregnancy and subsequent fetal and infant development:a prospective population-based cohort study in China[J]. J Clin Endocrinol Metab , 2011, 96 :3234–41. doi:10.1210/jc.2011-0274 |
| 24. | Sahu MT, Das V, Mittal S, et al. Overt and subclinical thyroid dysfunction among Indian pregnant women and its effect on maternal and fetal outcome[J]. Arch Gynecol Obstet , 2010, 281 :215–20. doi:10.1007/s00404-009-1105-1 |
| 25. | Hirsch D, Levy S, Nadler V, et al. regnancy outcomes in women with severe hypothyroidism[J]. Eur J Endocrinol , 2013, 169 :313–20. doi:10.1530/EJE-13-0228 |
| 26. | Jiang F, Gao JS, Ma LK, et al. Pregnant outcome of patients with hypothyroidism after thyroxine replacement therapy[J]. Reproductive Medicine , 2013, 22 :836–40. |
| 27. | Cleary-Goldman J, Malone FD, Lamber-Messer lian, et al. Maternal thyroid hypofunction and pregnancy outcome[J]. Obstet Gynecol , 2008, 112 :85–92. doi:10.1097/AOG.0b013e3181788dd7 |
| 28. | Casey BM, Dashe JS, Wells CE, et al. Subclinical hypothyroidism and pregnancy outcomes[J]. Obstet Gynecol , 2005, 105 :239–45. doi:10.1097/01.AOG.0000152345.99421.22 |
| 29. | Casey BM, Dashe JS, Spong CY, et al. Perinatal significance of isolated maternal hypothyroxinemia identified in the first half of pregnancy[J]. Obstet Gynecol , 2007, 109 :1129–35. doi:10.1097/01.AOG.0000262054.03531.24 |
| 30. | Schneuer FJ, Nassar N, Tasevski V, et al. Association and predictive accuracy of high TSH serum levels in first trimester and adverse pregnancy outcomes[J]. J Clin Endocrinol Metab , 2012, 97 :3115–22. doi:10.1210/jc.2012-1193 |
| 31. | Ajmani NS, Aggarwal D, Bhatia P, et al. Prevalence of overt and subclinical thyroid dysfunction among pregnant women and its effect on maternal and fetal outcome[J]. Journal of obstetrics and gynaecology of India , 2014, 64 :105–10. |
| 32. | Lan Y, Zhao YC, Ren X. Pregnant outcomes of patients with subclinical hypothyroidism[J]. Guangdong Medical Journal , 2012, 33 :2321–4. |
| 33. | Saki F, Dabbaghmanesh MH, Ghaemi SZ. Thyroid Function in Pregnancy and Its Influences on Maternal and Fetal Outcomes[J]. Int J Endocrinol Metab , 2014, 12 :e19378. |
| 34. | Liu XH, Gao SH, Wang JM, et al. Pregnant outcome of patients with subclinical hypothyroidism[J]. Chinese Journal of Perinatal Medicine , 2012, 15 :696–700. |
| 35. | Ashoor G, Maiz N, Rotas M, et al. Maternal thyroid function at 11-13 weeks of gestation and spontaneous preterm delivery[J]. Obstet Gynecol , 2011, 117 :293–8. doi:10.1097/AOG.0b013e318205152c |
| 36. | Haddow JE, Cleary-Goldman J, McClain MR, et al. Thyroperoxidase and thyroglobulin antibodies in early pregnancy and preterm delivery[J]. Obstet Gynecol , 2010, 116 :58–62. doi:10.1097/AOG.0b013e3181e10b30 |
| 37. | Negro R, Formoso G, Mangieri T, et al. Levothyroxine treatment in euthyroid pregnant women with autoimmune thyroid disease:effects on obstetrical complications[J]. J Clin Endocrinol Metab , 2006, 91 :2587–91. doi:10.1210/jc.2005-1603 |
| 38. | Ghafoor F, Mansoor M, Malik T, et al. Role of thyroid peroxidase antibodies in the outcome of pregnancy[J]. Journal of the College of Physicians and Surgeons-Pakistan:JCPSP , 2006, 16 :4698–71. |
| 39. | Iijima T, Tada H, Hidaka Y, et al. Effects of autoantibodies on the course of pregnancy and fetal growth[J]. Obstetrics and gynecology , 1997, 90 :364–9. doi:10.1016/S0029-7844(97)00283-4 |
| 40. | Nambiar V, Jagtap VS, Sarathi V, et al. Prevalence and impact of thyroid disorders on maternal outcome in asian-Indian pregnant women. J Thyroid Res, 2011: 429097. |
| 41. | Stagnaro-Green A, Chen X, Bogden JD, et al. The thyroid and pregnancy:a novel risk factor for very preterm delivery[J]. Thyroid:official journal of the American Thyroid Association , 2005, 15 :351–7. doi:10.1089/thy.2005.15.351 |
| 42. | Negro R, Schwartz A, Gismondi R, et al. Thyroid antibody positivity in the first trimester of pregnancy is associated with negative pregnancy outcomes[J]. J Clin Endocrinol Metab , 2011, 96 :E920–4. doi:10.1210/jc.2011-0026 |
| 43. | Glinoer D, Riahi M, Grün JP, et al. Risk of subclinical hypothyroidism in pregnant women with asymptomatic autoimmune thyroid disorders[J]. J Clin Endocrinol Metab , 1994, 79 :197–204. |
| 44. | Bhattacharyya R, Mukherjee K, Das A, et al. Anti-thyroid peroxidase antibody positivity during early pregnancy is associated with pregnancy complications and maternal morbidity in later life[J]. J Nat Sci Biol Med , 2015, 6 :402–405. doi:10.4103/0976-9668.160021 |
| 45. | Chen X, B Jin, Xia J, et al. Effects of Thyroid Peroxidase Antibody on Maternal and Neonatal Outcomes in Pregnant Women in an Iodine-Sufficient Area in China. Int J Endocrinol, 2016: doi:10.1155/2016/6461380. |
| 46. | Yang J, Guo H, Ding S, et al. Effect of the treatment acceptance on the perinatal outcomes in women with subclinical hypothyroidism, positive thyroid gland peroxidase antibody in early pregnancy[J]. Zhonghua Fu Chan Ke Za Zhi , 2015, 50 :652–7. |
| 47. | Rosario PW, Carvalho M, Calsolari MR. TSH reference values in the first trimester of gestation and correlation between maternal TSH and obstetric and neonatal outcomes:a prospective Brazilian study. Arch Endocrinol Metab, 2016: doi:10.1590/2359-3997000000132. |
| 48. | Daniel I. Nassie, Eran Ashwal, et al. Is there an association between subclinical hypothyroidism and preterm uterine contractions? A prospective observational study. J Matern Fetal Neonatal Med, 2016: doi:10.1080/14767058.20161191065. |
| 49. | Thangaratinam S, Tan A, Knox E, et al. Association between thyroid autoantibodies and miscarriage and preterm birth:meta-analysis of evidence[J]. BMJ , 2011, 342 :d261. |
| 50. | Challis JR, Lockwood CJ, Myatt L, et al. Inflammation and pregnancy[J]. Reprod Sci , 2009, 16 :206–15. doi:10.1177/1933719108329095 |
 2016, Vol. 29
2016, Vol. 29
