文章信息
- 王丹, 冯雪菲, 齐士格, 王秋童, 胡亚男, 王志会, 王宝华.
- Wang Dan, Feng Xuefei, Qi Shige, Wang Qiutong, Hu Yanan, Wang Zhihui, Wang Baohua
- 中国三省老年代谢综合征患者抑郁状况分析
- Depression status of elderly patients with metabolic syndrome in three provinces of China
- 中华流行病学杂志, 2023, 44(4): 568-574
- Chinese Journal of Epidemiology, 2023, 44(4): 568-574
- http://dx.doi.org/10.3760/cma.j.cn112338-20220926-00809
-
文章历史
收稿日期: 2022-09-26
2. 中国医科大学公共卫生学院, 沈阳 110122;
3. 中国疾病预防控制中心慢性非传染性疾病预防控制中心老年健康室, 北京 100050
2. School of Public Health, China Medical University, Shenyang 110122, China;
3. Division of Elderly Health, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing 100050, China
MS是多种代谢成分异常聚集的病理状态,是心血管疾病的主要危险因素。2015-2017年我国20岁以上居民MS患病率为31.1%,60~75岁、≥76岁人群MS患病率分别为43.9%、44.2%,随着年龄增加MS患病率呈现逐渐上升的趋势[1]。老年MS患者因异常的代谢机制、炎症过程、自主神经失调等原因容易导致其共病抑郁[2-3],且二者之间存在正相关关系[4-5]。研究发现,我国有20.1%的老年人存在抑郁症状[6],抑郁不仅增加了家庭医疗支出[7],还影响了老年人慢性疾病的愈后效果,关注老年MS患者心理健康问题有助于减缓疾病的发展。MS和抑郁均会增加老年人患心血管疾病的风险[8-9],早期对MS患者抑郁状况的识别有助于及时发现心血管疾病的高风险个体。
既往对MS与抑郁之间的关系研究多集中于韩国和欧美国家[10-12],中国的传统文化和饮食习惯与国外存在较大差异,针对中国老年人群开展相关研究,可提供中国本土化的研究证据,对预防老年MS患者抑郁以及疾病所导致的心血管并发症有重要意义。本研究利用财政部重大公共卫生专项“老年期重点疾病预防和干预”项目2019年抽取的具有代表性的大样本调查数据,了解我国社区老年MS患者的抑郁状况,同时探索不同MS异常组分患者的抑郁状况,分析老年MS患者抑郁的影响因素,为预防和减少老年MS人群抑郁风险提供科学依据。
资料与方法 (1) 数据来源来源于“老年期重点疾病预防和干预”项目,该项目采用电子化问卷的形式面对面询问收集调查对象人口统计学信息、日常生活习惯、日常生活活动能力(ADL)、主要慢性病相关信息、心理健康、认知功能等数据,身高和体重信息通过现场身体测量的方式获取。本研究以项目2019年采用多阶段分层整群随机抽样方法抽取的河南省、广东省、辽宁省16 199名≥60岁社区老年人为研究对象,剔除缺失变量1 001名,最终纳入分析的有效样本为15 198名。本研究通过中国CDC慢性非传染性疾病预防控制中心伦理委员会的审查(批准文号:201902),受试对象均签署了知情同意书。
(2) MS的判断标准根据2004年中华医学会糖尿病学分会对MS的诊断标准的建议,将具有超重/肥胖、高血糖、高血压、血脂异常4项组分中的3项或全部者定义为MS[13]。本研究以问卷调查的形式了解研究对象高血压、糖尿病、血脂异常等慢性病的相关信息,包括:是否患病、诊断单位[省级及以上医院、地(市)级医院、县(区)级医院、乡镇卫生院(社区卫生服务中心)]、诊断时间、目前服药治疗情况。根据该项目现场调查工作要求,不能明确回答诊断单位和诊断时间的均视为未患该病。通过现场测量的方式收集调查对象身高和体重数据,以18.5 kg/m2≤BMI < 24.0 kg/m2诊断为正常,BMI≥24.0 kg/m2诊断为超重,BMI≥28.0 kg/m2诊断为肥胖。
(3) 心理健康状况判断采用PHQ-9抑郁筛查量表评估调查对象近2周内的心理状况。中文版PHQ-9量表的敏感性和特异性得到广泛验证[14],其易用性和相对简洁性适用于我国老年人抑郁症状筛查[15]。量表包括9个问题,每个问题的答案为“没有、有几天、有一半时间、几乎天天”,分别对应0、1、2、3分,总分27分,≥5分即判断研究对象2周内存在抑郁症状。
(4) 质量控制项目开展了两轮现场调查员培训,参与调查工作的人员均经过统一培训且考核合格。中国CDC慢性非传染性疾病预防控制中心对各项目点进行了技术指导和督查质控。项目采用平板电脑作为问卷调查工具进行面对面询问调查且全程录音。
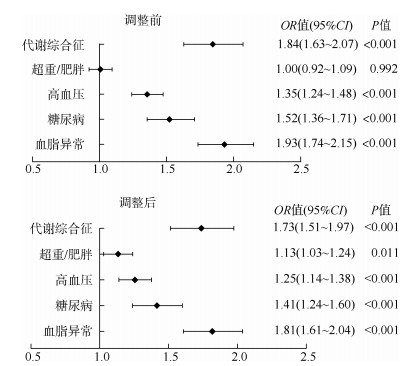
(5) 统计学分析采用SPSS 21.0软件对数据进行清理和分析,采用GraphPad Prism 9软件绘制森林图。计数资料采用率进行描述,组间比较采用χ2检验。采用二元logistic回归分析对MS各组分的混杂因素进行调整,因变量为抑郁状况(0=无,1=有),自变量分别为MS、超重/肥胖、高血压、糖尿病、血脂异常,采用森林图对调整前后MS各组分与抑郁的关系进行展示。采用多因素logistic回归分析老年MS患者抑郁的影响因素。双侧检验,检验水准α=0.05。
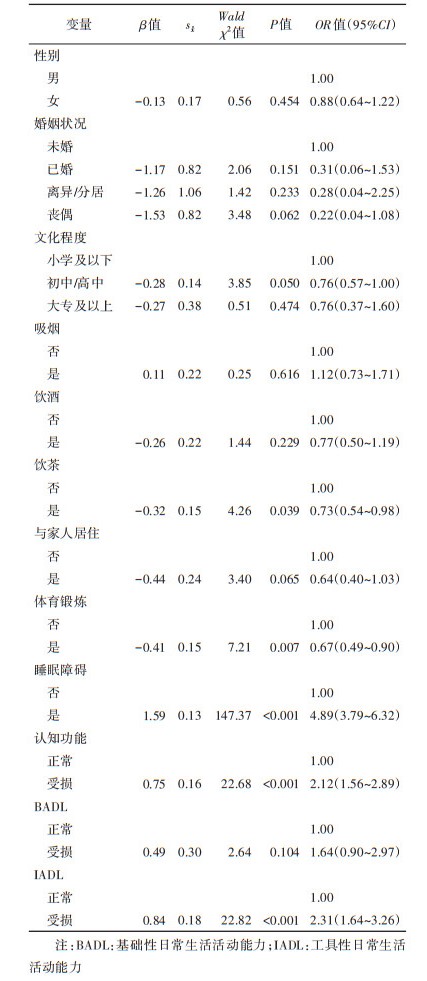
结果 (1) 抑郁状况共纳入15 198名≥60岁老年人,其中MS患者1 648名(10.84%),存在抑郁症状者2 548名(16.77%)。对MS患者抑郁状况进行分析,结果显示,男性MS患者的抑郁症状检出率和女性MS患者的抑郁症状检出率分别为20.74%、28.15%。随着年龄的增加抑郁症状检出率呈上升趋势(P=0.003);文化程度越高抑郁症状检出率越低(P < 0.001)。男性、饮酒、饮茶、与家人居住、参加体育锻炼的老年MS患者抑郁症状检出率较低,组间差异有统计学意义(P < 0.05);存在睡眠障碍、认知功能受损、基础性日常生活活动能力(BADL)受损、工具性日常生活活动能力(IADL)受损的老年MS患者抑郁症状检出率较高,组间差异有统计学意义(P < 0.05)。见表 1。
分析不同MS异常组分数目患者的抑郁状况。患有0、1、2、3、4项MS异常组分数目的患者分别有4 484、5 552、3 514、1 329、319名,抑郁症状检出人数(检出率)分别为653名(14.56%)、842名(15.17%)、633名(18.01%)、335名(25.21%)、85名(26.65%)。MS异常组分数目与抑郁症状检出率呈正相关关系,组间差异有统计学意义(P < 0.05)
(3) 不同MS异常组分患者的抑郁风险比较未调整混杂因素时,高血压、糖尿病、血脂异常患者的抑郁风险分别是正常人群的1.35倍(OR=1.35,95%CI:1.24~1.48)、1.52倍(OR=1.52,95%CI:1.36~1.71)、1.93倍(OR=1.93,95%CI:1.74~2.15)(图 1);调整性别、年龄、文化程度、婚姻状况、吸烟、饮酒、饮茶、是否与家人居住、体育锻炼、睡眠情况、认知功能、BADL、IADL混杂因素的影响,比较调整前后MS异常组分患者的抑郁状况:MS、超重/肥胖、高血压、糖尿病、血脂异常患者的抑郁风险分别是正常人群的1.73倍(OR=1.73,95%CI:1.51~1.97)、1.13倍(OR=1.13,95%CI:1.03~1.24)、1.25倍(OR=1.25,95%CI:1.14~1.38)、1.41倍(OR=1.41,95%CI:1.24~1.60)、1.81倍(OR=1.81,95%CI:1.61~2.04)(图 1)。调整前后,老年MS、高血压、糖尿病、血脂异常均与抑郁显著相关(P < 0.05),且影响程度均低于未调整前。调整后,超重/肥胖老年人群抑郁风险高于正常人群(P < 0.05)。
|
| 图 1 不同代谢综合征异常组分患者的抑郁风险比较 |
多因素logistic回归分析结果显示,存在睡眠障碍者抑郁症状检出率高于睡眠正常者(OR=4.89,95%CI:3.79~6.32)。认知功能受损患者抑郁症状检出率是正常者的2.12倍(OR=2.12,95%CI:1.56~2.89);IADL受损患者抑郁症状检出率是正常者的2.31倍(OR=2.31,95%CI:1.64~3.26)。饮茶(OR=0.73,95%CI:0.54~0.98)、体育锻炼(OR=0.67,95%CI:0.49~0.90)是老年MS患者抑郁的保护因素(P < 0.05)。见表 2。
本研究结果显示,我国社区1/4以上的老年MS患者存在抑郁症状,且老年人抑郁症状检出率随着MS异常组分数目的增加呈上升趋势。我国≥60岁居民患有≥1种慢性病的比例高达76.3%,近3/4的老年人在晚年患有慢性病,高血压、糖尿病、血脂异常患病率居前三位[16]。多项研究发现,老年慢性病患者的抑郁风险高于正常人群[17-18],其中代谢性疾病患者的抑郁风险处于较高水平[19-21],本研究结果显示,老年MS与抑郁存在关联。
本研究结果显示,有0、2项MS异常组分数目的患者抑郁症状检出率为14.56%、18.01%,有3、4项MS异常组分数目的患者抑郁症状检出率为25.21%、26.65%。这一研究结果提示,应重点关注有3、4项MS异常组分数目的患者,且可将这两类人群进行统一管理;同时也可将有0、1、2项MS异常组分数目的患者进行统一管理。医疗卫生保健部门可根据不同的人群采取不同力度的医疗卫生预防或干预措施,可将卫生资源效益最大化。
本研究结果显示,超重/肥胖、高血压、糖尿病、血脂异常患者的抑郁风险分均高于正常人群,其中血脂异常对抑郁影响最大。一项对全球1997-2017年老年MS患者抑郁状况进行的Meta分析结果显示,肥胖与抑郁关联性最强[4]。这与本研究结果不一致,可能是因为纳入该研究的大多数调查都是在欧美国家进行的,由于欧美国家高油、高脂的饮食习惯导致该地区老年人群的肥胖率远高于我国老年人,从而出现肥胖与抑郁症状之间关联性更强的结论。我国将TC水平≥6.19 mmol/L、LDL-C≥4.14 mmol/L、TG≥2.27 mmol/L、HDL-C < 1.04 mmol/L,符合其中的一条或者几条诊断为血脂异常[22]。有研究发现,TG在增加抑郁风险方面发挥了重要的作用[23-24],且男性风险高于女性[25]。本研究仅针对血脂异常患者进行了分析,不同类型的血脂异常与抑郁的关系还需进一步研究。研究发现,肥胖中的中心性肥胖与抑郁的关联性较强[4, 26],肥胖和抑郁并存会加重疾病的发病率和残疾率,可采用常规护理结合行为减肥的治疗从而有效减轻体重和抑郁症状[27]。Liao等[28]的研究结果显示,体重不足与抑郁症状检出率较高有关,本研究仅将调查对象分为正常与超重/肥胖2组进行分析,消瘦与抑郁之间的关系还需进一步探索。
Kessing等[29]的调查结果显示,规范使用高血压药物不会增加患者的抑郁风险。由于老年人随着年龄增加记忆力不断减退的生理特性,导致老年人多服或忘服降压药的概率增加,从而产生由用药依从性降低导致的焦虑情绪的发生,这可能是老年高血压患者抑郁症状检出率较高的原因之一。糖尿病在疾病发生发展的前中后期均会出现不同程度的微血管病变,这是导致抑郁风险增加的潜在机制之一[30]。大量研究已证实了糖尿病病程与微血管并发症存在正相关关系,但是探索糖尿病病程与抑郁严重程度的相关性研究较少,了解糖尿病病程与抑郁严重程度的临界值有助于初级医疗卫生保健部门针对不同病程的糖尿病人群制定不同心理干预措施,从而使预防效益最大化。
多因素logistic回归分析结果显示,存在睡眠障碍者抑郁症状检出率高于正常者。Bishehsari等[31]的研究发现,昼夜节律系统的破坏可以改变肠道微生物群结构和功能,扰乱宿主的新陈代谢导致MS。关注老年MS患者睡眠状况,能在一定程度上降低抑郁风险。随着年龄的增加,大部分老年人会出现不同程度的认知功能损伤,老年人认知功能损伤与抑郁相关[32]。认知可因抑郁导致的神经递质含量降低、炎症因子水平升高而导致其功能下降[33]。鉴于本研究为横断面研究尚不能判定抑郁和认知功能受损的因果关系。Ning等[34]的研究发现,存在MS和抑郁症状的老年人与ADL受损显著相关,本研究将ADL分为BADL和IADL两个维度进行分析,发现IADL受损患者抑郁症状检出率高于正常者,未发现BADL受损与抑郁的相关性。这一研究结果提示,卫生保健部门应重点关注IADL受损的MS患者心理健康状况。
本研究存在局限性。①调查使用的PHQ-9抑郁筛查量表对老年人抑郁症状进行筛查,只能反映调查对象近半个月的抑郁情绪;②调查对象的高血压、糖尿病、血脂异常等相关疾病数据的收集是通过患者自报的形式获取的,可能会存在一定的回忆偏倚;③本研究未纳入可能对研究结果有影响的变量,如:经济水平、未纳入分析的慢性病、遗传因素等。
综上所述,本研究通过大规模的横断面研究发现MS及其组分均会增加老年人的抑郁风险,存在睡眠障碍、认知功能受损、IADL损伤的老年MS人群抑郁风险较高,饮茶和体育锻炼能在一定程度上降低抑郁风险。
利益冲突 所有作者声明无利益冲突
作者贡献声明 王丹:数据分析、论文撰写;冯雪菲、王秋童、胡亚男:数据分析、论文修订;齐士格、王志会:数据收集、论文修订;王宝华:研究设计、论文修订
| [1] |
Yao F, Bo YC, Zhao LY, et al. Prevalence and influencing factors of metabolic syndrome among adults in China from 2015 to 2017[J]. Nutrients, 2021, 13(12): 4475. DOI:10.3390/nu13124475 |
| [2] |
郭庆军, 黄炜, 陈晓健, 等. 代谢综合征抑郁症共病机制研究进展[J]. 中国公共卫生, 2021, 37(1): 185-188. Guo QJ, Huang W, Chen XJ, et al. Progress in researches on mechanism of comorbidity of metabolic syndrome and depression[J]. Chin J Public Health, 2021, 37(1): 185-188. DOI:10.11847/zgggws1124610 |
| [3] |
Milaneschi Y, Lamers F, Berk M, et al. Depression heterogeneity and its biological underpinnings: toward immunometabolic depression[J]. Biol Psychiatry, 2020, 88(5): 369-380. DOI:10.1016/j.biopsych.2020.01.014 |
| [4] |
Repousi N, Masana MF, Sanchez-Niubo A, et al. Depression and metabolic syndrome in the older population: a review of evidence[J]. J Affect Disord, 2018, 237: 56-64. DOI:10.1016/j.jad.2018.04.102 |
| [5] |
Wiltink J, Michal M, Jünger C, et al. Associations between degree and sub-dimensions of depression and metabolic syndrome (MetS) in the community: results from the Gutenberg Health Study (GHS)[J]. BMC Psychiatry, 2018, 18(1): 114. DOI:10.1186/s12888-018-1691-1 |
| [6] |
Luo YT, Li Y, Xie JF, et al. Symptoms of depression are related to sedentary behavior and sleep duration in elderly individuals: a cross-sectional study of 49, 317 older Chinese adults[J]. J Affect Disord, 2022, 308: 407-412. DOI:10.1016/j.jad.2022.04.102 |
| [7] |
Lu SY, Liu TY, Wong GHY, et al. Health and social care service utilisation and associated expenditure among community-dwelling older adults with depressive symptoms[J]. Epidemiol Psychiatr Sci, 2021, 30: e10. DOI:10.1017/S2045796020001122 |
| [8] |
Yu LS, Chen Y, Wang N, et al. Association between depression and risk of incident cardiovascular diseases and its sex and age modifications: a prospective cohort study in southwest China[J]. Front Public Health, 2022, 10: 765183. DOI:10.3389/fpubh.2022.765183 |
| [9] |
Fahed G, Aoun L, Zerdan MB, et al. Metabolic syndrome: updates on pathophysiology and management in 2021[J]. Int J Mol Sci, 2022, 23(2): 786. DOI:10.3390/ijms23020786 |
| [10] |
Godin O, Bennabi D, Yrondi A, et al. Prevalence of metabolic syndrome and associated factors in a cohort of individuals with treatment-resistant depression: results from the FACE-DR study[J/OL]. J Clin Psychiatry, 2019, 80(6): 19 m12755. DOI: 10.4088/JCP.19m12755.
|
| [11] |
Jeon SW, Lim SW, Shin DW, et al. Metabolic syndrome and incident depressive symptoms in young and middle-aged adults: a cohort study[J]. J Affect Disord, 2019, 246: 643-651. DOI:10.1016/j.jad.2018.12.073 |
| [12] |
Dekker IP, Marijnissen RM, Giltay EJ, et al. The role of metabolic syndrome in late-life depression over 6 years: the NESDO study[J]. J Affect Disord, 2019, 257: 735-740. DOI:10.1016/j.jad.2019.07.060 |
| [13] |
中华医学会糖尿病学分会代谢综合征研究协作组. 中华医学会糖尿病学分会关于代谢综合征的建议[J]. 中华糖尿病杂志, 2004, 12(3): 156-161. Metabolic Syndrome Research Collaboration Group of Diabetes Branch of Chinese Medical Association. Recommendations of the diabetes branch of the Chinese medical association on metabolic syndrome[J]. Chin J Diabetes, 2004, 12(3): 156-161. DOI:10.3321/j.issn:1006-6187.2004.03.002 |
| [14] |
Yu XN, Tam WWS, Wong PTK, et al. The patient health questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong[J]. Compr Psychiatry, 2012, 53(1): 95-102. DOI:10.1016/j.comppsych.2010.11.002 |
| [15] |
Zhang H, Wang SM, Wang LJ, et al. Comparison of the Geriatric Depression Scale-15 and the Patient Health Questionnaire-9 for screening depression in older adults[J]. Geriatr Gerontol Int, 2020, 20(2): 138-143. DOI:10.1111/ggi.13840 |
| [16] |
王丽敏, 陈志华, 张梅, 等. 中国老年人群慢性病患病状况和疾病负担研究[J]. 中华流行病学杂志, 2019, 40(3): 277-283. Wang LM, Chen ZH, Zhang M, et al. Study of the prevalence and disease burden of chronic disease in the elderly in China[J]. Chin J Epidemiol, 2019, 40(3): 277-283. DOI:10.3760/cma.j.issn.0254-6450.2019.03.005 |
| [17] |
Cui LY, Ding D, Chen JF, et al. Factors affecting the evolution of Chinese elderly depression: a cross-sectional study[J/OL]. BMC Geriatr, 2022, 22(1): 109. DOI: 10.1186/s12877-021-02675-z.
|
| [18] |
Meher T, Muhammad T, Gharge S. The association between single and multiple chronic conditions and depression among older population in India: a comparative study between men and women[J]. Int J Geriatr Psychiatry, 2022, 37(1): 1-12. DOI:10.1002/gps.5639 |
| [19] |
Jiang C, Yin H, Liu AB, et al. Dietary inflammatory index and depression risk in patients with chronic diseases and comorbidity[J]. J Affect Disord, 2022, 301: 307-314. DOI:10.1016/j.jad.2022.01.008 |
| [20] |
Hu JY, Zheng XY, Shi GDJ, et al. Associations of multiple chronic disease and depressive symptoms with incident stroke among Chinese middle-aged and elderly adults: a nationwide population-based cohort study[J]. BMC Geriatr, 2022, 22(1): 660. DOI:10.1186/s12877-022-03329-4 |
| [21] |
Boima V, Tetteh J, Yorke E, et al. Older adults with hypertension have increased risk of depression compared to their younger counterparts: evidence from the World Health Organization study of Global Ageing and Adult Health Wave 2 in Ghana[J]. J Affect Disord, 2020, 277: 329-336. DOI:10.1016/j.jad.2020.08.033 |
| [22] |
中国成人血脂异常防治指南制订联合委员会. 中国成人血脂异常防治指南[J]. 中华心血管病杂志, 2007, 35(5): 390-419. Joint Committee for the Formulation of Guidelines for the Prevention and Treatment of Adult Blood Lipid Disorders in China. Chinese guidelines on prevention and treatment of dyslipidemia in adults[J]. Chin J Cardiol, 2007, 35(5): 390-419. DOI:10.3760/j.issn:0253-3758.2007.05.003 |
| [23] |
Huang YH, Xu P, Fu XY, et al. The effect of triglycerides in the associations between physical activity, sedentary behavior and depression: an interaction and mediation analysis[J]. J Affect Disord, 2021, 295: 1377-1385. DOI:10.1016/j.jad.2021.09.005 |
| [24] |
Dregan A, Rayner L, Davis KAS, et al. Associations between depression, arterial stiffness, and metabolic syndrome among adults in the UK biobank population study: a mediation analysis[J]. JAMA Psychiatry, 2020, 77(6): 598-606. DOI:10.1001/jamapsychiatry.2019.4712 |
| [25] |
Xu L, Wang K, Wang SF, et al. Sex differences in the association between serum lipids and depressive symptoms: a longitudinal population-based study[J]. J Affect Disord, 2021, 291: 154-162. DOI:10.1016/j.jad.2021.05.011 |
| [26] |
Cho SJ, Lee HJ, Rhee SJ, et al. The relationship between visceral adiposity and depressive symptoms in the general Korean population[J]. J Affect Disord, 2019, 244: 54-59. DOI:10.1016/j.jad.2018.09.046 |
| [27] |
Ma J, Rosas LG, Lv N, et al. Effect of integrated behavioral weight loss treatment and problem-solving therapy on body mass index and depressive symptoms among patients with obesity and depression: the RAINBOW randomized clinical trial[J]. JAMA, 2019, 321(9): 869-879. DOI:10.1001/jama.2019.0557 |
| [28] |
Liao W, Luo ZC, Hou YT, et al. Age and gender specific association between obesity and depressive symptoms: a large-scale cross-sectional study[J/OL]. BMC Public Health, 2020, 20(1): 1565. DOI: 10.1186/s12889-020-09664-8.
|
| [29] |
Kessing LV, Rytgaard HC, Ekstrøm CT, et al. Antihypertensive drugs and risk of depression: a nationwide population-based study[J]. Hypertension, 2020, 76(4): 1263-1279. DOI:10.1161/HYPERTENSIONAHA.120.15605 |
| [30] |
van Sloten TT, Sedaghat S, Carnethon MR, et al. Cerebral microvascular complications of type 2 diabetes: stroke, cognitive dysfunction, and depression[J]. Lancet Diabetes Endocrinol, 2020, 8(4): 325-336. DOI:10.1016/S2213-8587(19)30405-X |
| [31] |
Bishehsari F, Voigt RM, Keshavarzian A. Circadian rhythms and the gut microbiota: from the metabolic syndrome to cancer[J]. Nat Rev Endocrinol, 2020, 16(12): 731-739. DOI:10.1038/s41574-020-00427-4 |
| [32] |
Li N, Chen G, Zeng P, et al. Prevalence and factors associated with mild cognitive impairment among Chinese older adults with depression[J]. Geriatr Gerontol Int, 2018, 18(2): 263-268. DOI:10.1111/ggi.13171 |
| [33] |
胡楠楠, 孙继军. 老年抑郁症患者神经递质、炎症因子水平与认知功能的关系[J]. 中国老年学杂志, 2020, 40(12): 2604-2606. Hu NN, Sun JJ. Relationship between levels of neurotransmitters and inflammatory factors and cognitive function in elderly patients with depression[J]. Chin J Gerontol, 2020, 40(12): 2604-2606. DOI:10.3969/j.issn.1005-9202.2020.12.044 |
| [34] |
Ning HT, Du Y, Zhao YN, et al. Longitudinal impact of metabolic syndrome and depressive symptoms on subsequent functional disability among middle-aged and older adults in China[J]. J Affect Disord, 2022, 296: 216-223. DOI:10.1016/j.jad.2021.09.061 |
 2023, Vol. 44
2023, Vol. 44