文章信息
- 邸新博, 刘世炜, 谢慧宇, 曾新颖, 孟子达, 肖琳.
- Di Xinbo, Liu Shiwei, Xie Huiyu, Zeng Xinying, Meng Zida, Xiao Lin
- 中国15岁及以上吸烟人群复吸率及其影响因素研究
- Smoking relapse rate and influencing factors in smokers aged 15 years and above in China
- 中华流行病学杂志, 2022, 43(9): 1388-1393
- Chinese Journal of Epidemiology, 2022, 43(9): 1388-1393
- http://dx.doi.org/10.3760/cma.j.cn112338-20211130-00929
-
文章历史
收稿日期: 2021-11-30
2. 中国疾病预防控制中心控烟办公室,北京 100050
2. Tobacco Control Office, Chinese Center for Disease Control and Prevention, Beijing 100050, China
我国目前吸烟人数超过3亿[1],每年有100多万人死于烟草相关疾病,包括癌症、脑卒中、慢性阻塞性肺疾病。如果烟草流行趋势不能得到有效遏制,到2050年每年将有300万人死于烟草相关疾病[2]。为遏制烟草流行,国务院发布《“健康中国2030”规划纲要》,明确提出到2030年15岁以上人群吸烟率降至20%的目标。促进吸烟者戒烟是降低人群吸烟率的重要手段,包含增加吸烟者戒烟尝试和防止戒烟者复吸两个方面。目前我国关于戒烟尝试行为及其影响因素的相关研究较多,而针对复吸的研究较少。本研究使用2018年中国成人烟草调查数据,描述不同特征吸烟人群的复吸情况,分析影响复吸的可能因素。
对象与方法1. 研究对象:本研究数据来源于2018年中国成人烟草调查。该调查覆盖全国31个省(自治区、直辖市)的200个区/县的400个居委会/村,采用多阶段分层整群随机抽样方法抽取非集体居住的≥15岁的中国籍常住居民进行调查。共计19 376人完成调查,本研究以吸烟人群为研究对象,所有研究对象均已知情并同意参加调查。
2. 调查内容与方法:2018年中国成人烟草调查由通过培训合格的调查员采用入户形式,使用平板电脑通过面对面询问的方法进行数据采集。数据收集内容包括人口学特征、烟草使用、电子烟使用、戒烟、二手烟、烟草价格、控烟宣传、烟草广告、促销和赞助以及人们对烟草使用的知识、态度和认知等。
3. 指标定义:本研究通过询问调查对象“您现在吸烟吗?每天吸、不是每天吸、还是不吸?”来界定现在吸烟者,回答每天吸、不是每天吸则为现在吸烟者;通过对现在非吸烟者询问“您以前吸烟吗?每天吸,不是每天吸,还是从不吸烟?”来界定戒烟者,当调查对象现在不吸烟,且此题回答以前每天吸、不是每天吸,则为戒烟者;通过对现在吸烟者询问“过去您是否戒过烟?”(这里的戒烟指认真考虑过要戒烟并有所行动)来界定复吸者,回答戒过烟则为复吸者。复吸率指戒过烟的现在吸烟者在曾经吸烟者和戒过烟的现在吸烟者中所占的百分比。
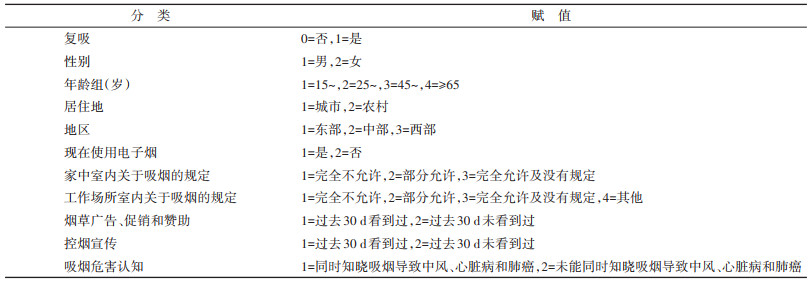
4. 统计学分析:使用SAS 9.4软件进行复杂抽样设计的数据清洗、样本加权和统计学分析。采用基于复杂抽样设计的Rao-Scott χ2检验进行数据单因素组间比较,包含性别、年龄、城乡等。采用复杂抽样设计的logistic回归模型,将戒过烟的人复吸作为因变量(是=1;否=0),以性别、年龄组、居住地、地区、现在电子烟使用情况、家中室内吸烟规定、工作场所室内吸烟规定、过去30 d看到过烟草广告、促销和赞助、过去30 d看到过控烟宣传以及对吸烟危害的认知等为自变量建立回归模型。见表 1。以双侧检验P < 0.05为差异有统计学意义。
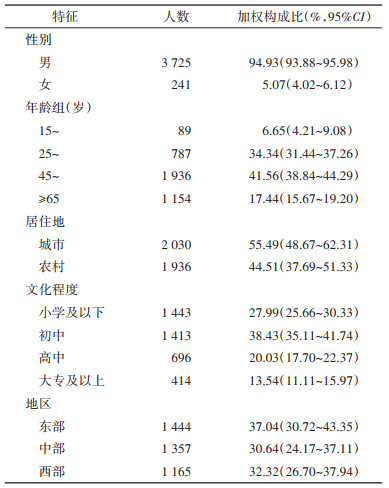
1. 基本情况:2018年中国成人烟草调查共完成19 376份个人问卷,整体应答率为91.50%。本次调查中,≥15岁戒过烟人群共3 966人,其中男性3 725人,女性241人;城市2 030人,农村1 936人。见表 2。
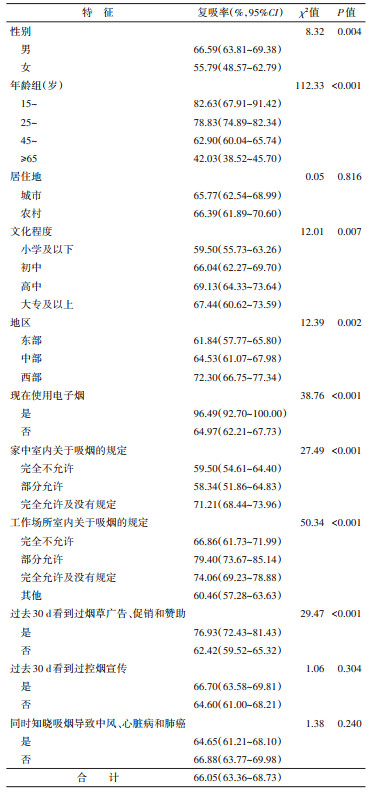
2. 不同特征人群的复吸情况:在戒过烟的≥15岁人群中,复吸的比例为66.05%,其中男性(66.59%)高于女性(55.79%);低年龄组复吸率远高于高年龄组,15~、25~、45~和≥65岁年龄组的复吸率分别为82.63%、78.83%、62.90%和42.03%;高中文化程度复吸率最高为69.13%;不同地区之间复吸率存在差异,西部地区最高,为72.30%,差异均有统计学意义(均P < 0.05)。城市和农村之间复吸率差异无统计学意义,分别为65.77%和66.39%(P=0.816)。见表 3。
3. 影响复吸率的单因素分析:现在使用电子烟者(96.49%)远高于现在不使用电子烟者(64.97%);家中室内完全允许吸烟及没有规定者(71.21%)高于完全不允许吸烟者(59.50%)和部分允许吸烟者(58.34%);工作场所室内部分允许吸烟(79.40%)和完全允许及没有规定(74.06%)高于完全不允许吸烟(66.86%);过去30 d内看到过烟草广告、促销和赞助(76.93%)高于未看到(62.42%),差异均有统计学意义(P < 0.001)。过去30 d内看到过控烟宣传与未看到过控烟宣传之间差异无统计学意义(P=0.304),复吸率分别为66.70%和64.60%。是否同时知晓吸烟导致中风、心脏病和肺癌之间差异无统计学意义(P=0.240),复吸率分别为64.65%和66.88%。见表 3。
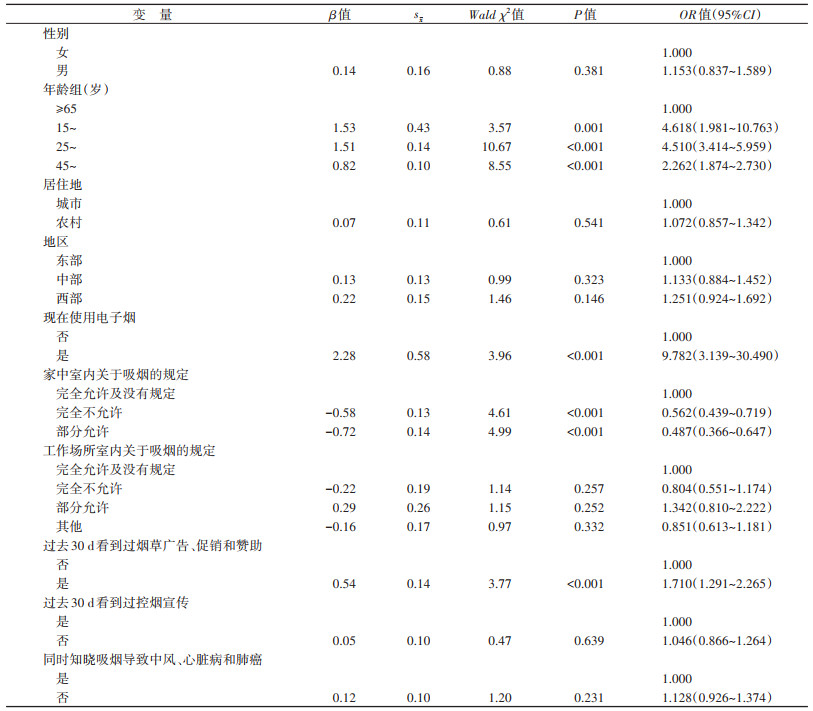
4. 影响复吸率的多因素分析:复杂抽样的多因素logistic回归模型分析结果显示,15~、25~及45~岁年龄组吸烟人群的复吸率分别是≥65岁年龄组的4.618(95%CI:1.981~10.763)倍、4.510(95%CI:3.414~5.959)倍和2.262(95%CI:1.874~2.730)倍。现在使用电子烟者复吸率是未使用电子烟者的9.782(95%CI:3.139~30.490)倍。家中室内完全不允许吸烟和部分允许吸烟的复吸率分别为完全允许吸烟及没有规定的0.562(95%CI:0.439~0.719)倍和0.487(95%CI:0.366~0.647)倍。过去30 d看到过烟草广告、促销和赞助者的复吸率是未看到者的1.710(95%CI:1.291~2.265)倍。不同性别、居住地、地区、工作场所室内有无禁烟规定、过去30 d是否看到过控烟宣传以及是否同时知晓吸烟导致中风、心脏病和肺癌之间复吸率差异无统计学意义(P > 0.05)。见表 4。
多项研究显示,减少与烟草有关的发病率和死亡率的主要困难是说服吸烟者戒烟并维持其戒烟状态,相当数量吸烟者戒烟尝试后复吸[3-5]。既往研究显示,性别[6-7]、年龄[8]、烟草依赖性[9]、戒烟持续时长[10]、专业人员给予的戒烟建议和指导[11]、无烟的家庭环境和工作环境[12-13]、电子烟或其他烟草制品的使用[14-16]等因素会影响吸烟者复吸。本研究显示,年龄、电子烟的使用、家庭和工作场所室内的无烟环境及烟草广告、促销和赞助的暴露情况会影响复吸率。
有研究显示,年轻的吸烟者可能低估了吸烟的健康危害,从而削弱他们戒烟的决心[17];年轻人在聚会、节日和庆祝活动中有更多的机会结伴吸烟[18],更容易受到同龄人的压力,这使他们在戒烟后更容易复吸[19];随着年龄增长,吸烟者的身体状况日益下降,其就医行为及接受医生的戒烟建议的比例增高[1],可能导致复吸的比例有所降低,因此复吸率随年龄增加而降低。与本研究的发现一致。
目前我国≥15岁人群的戒烟率为18.7%[1],而其他高、中等收入国家戒烟率通常超过50%[20]。尽管某些研究表明电子烟可能有助于吸烟者戒烟,但电子烟作为戒烟辅助工具的有效性的科学证据尚存在争议[21-23]。2021年WHO全球烟草报告中指出使用电子烟会对健康产生危害,建议各国加强电子烟管控[24]。本研究中,基于复杂抽样的多因素logistic回归模型分析结果显示,在戒过烟的人群中,现在使用电子烟者复吸的比例远高于不使用电子烟者(OR=9.782,95%CI:3.139~30.490),提示电子烟的使用可能会增加复吸的概率。McMillen等[16]也得到相同研究结果。
既往研究显示,家庭、工作场所的无烟环境有利于增加吸烟者尝试戒烟的同时降低复吸率[12-13]。本研究结果显示,在戒过烟的人群中,家中室内完全不允许吸烟和部分允许吸烟的复吸率低于完全允许吸烟及没有规定,提示应大力提倡无烟家庭建设,从而降低尝试戒烟者的复吸率。此外,本研究还显示过去30 d看到过烟草广告、促销和赞助的吸烟者的复吸率较未看到者高,建议严格执行《中华人民共和国广告法》,加强对烟草广告的管控,尽快出台相应的法律禁止烟草促销和赞助。
利益冲突 所有作者声明无利益冲突
作者贡献声明 邸新博:数据分析、论文撰写;谢慧宇、曾新颖、孟子达:数据分析;刘世炜、肖琳:论文修改
| [1] |
梁晓峰. 2015中国成人烟草调查报告[M]. 北京: 人民卫生出版社, 2016. Liang XF. 2015 China adult tobacco survey report[M]. Beijing: People's Health Publishing House, 2016. |
| [2] |
中华人民共和国国家卫生健康委员会. 中国吸烟危害健康报告2020[M]. 北京: 人民卫生出版社, 2021. State Health Commission of the People's Republic of China. China's report on health hazards of smoking 2020[M]. Beijing: People's Health Publishing House, 2021. |
| [3] |
Heffner JL, Lee TC, Arteaga C, et al. Predictors of post-treatment relapse to smoking in successful quitters: pooled data from two phase Ⅲ varenicline trials[J]. Drug Alcohol Depend, 2010, 109(1/3): 120-125. DOI:10.1016/j.drugalcdep.2009.12.022 |
| [4] |
Yong HH, Borland R, Cooper J, et al. Postquitting experiences and expectations of adult smokers and their association with subsequent relapse: findings from the International Tobacco Control (ITC) Four Country Survey[J]. Nicotine Tob Res, 2010, 12 Suppl(Suppl 1): S12-19. DOI:10.1093/ntr/ntq127 |
| [5] |
Hajek P, Stead LF, West R, et al. Relapse prevention interventions for smoking cessation[J]. Cochrane Database Syst Rev, 2013(8): CD003999. DOI:10.1002/14651858.CD003999.pub4 |
| [6] |
Borrelli B, Papandonatos G, Spring B, et al. Experimenter-defined quit dates for smoking cessation: adherence improves outcomes for women but not for men[J]. Addiction, 2004, 99(3): 378-385. DOI:10.1111/j.1360-0443.2004.00648.x |
| [7] |
Wetter DW, Kenford SL, Smith SS, et al. Gender differences in smoking cessation[J]. J Consult Clin Psychol, 1999, 67(4): 555-562. DOI:10.1037/0022-006x.67.4.555 |
| [8] |
Yi ZN, Mayorga ME, Lich KH, et al. Changes in cigarette smoking initiation, cessation, and relapse among U.S. adults: a comparison of two longitudinal samples[J]. Tob Induc Dis, 2017, 15: 17. DOI:10.1186/s12971-017-0121-3 |
| [9] |
Vangeli E, Stapleton J, Smit ES, et al. Predictors of attempts to stop smoking and their success in adult general population samples: a systematic review[J]. Addiction, 2011, 106(12): 2110-2121. DOI:10.1111/j.1360-0443.2011.03565.x |
| [10] |
Georgiadou C, Lavdaniti M, Psychogiou M, et al. Factors affecting the decision to quit smoking of the participants of a hospital-based smoking cessation program in Greece[J]. J Caring Sci, 2015, 4(1): 1-11. DOI:10.5681/jcs.2015.001 |
| [11] |
Song FJ, Maskrey V, Blyth A, et al. Differences in longer-term smoking abstinence after treatment by specialist or Nonspecialist advisors: secondary analysis of data from a relapse prevention trial[J]. Nicotine Tob Res, 2016, 18(5): 1061-1066. DOI:10.1093/ntr/ntv148 |
| [12] |
Hyland A, Higbee C, Travers MJ, et al. Smoke-Free homes and smoking cessation and relapse in a longitudinal population of adults[J]. Nicotine Tob Res, 2009, 11(6): 614-618. DOI:10.1093/ntr/ntp022 |
| [13] |
Alboksmaty A, Agaku IT, Odani S, et al. Prevalence and determinants of cigarette smoking relapse among US adult smokers: a longitudinal study[J]. BMJ Open, 2019, 9(11): e031676. DOI:10.1136/bmjopen-2019-031676 |
| [14] |
Verplaetse TL, Moore KE, Pittman BP, et al. Intersection of E-cigarette use and gender on transitions in cigarette smoking status: Findings across waves 1 and 2 of the population assessment of tobacco and health study[J]. Nicotine Tob Res, 2019, 21(10): 1423-1428. DOI:10.1093/ntr/nty187 |
| [15] |
Messer K, Vijayaraghavan M, White MM, et al. Cigarette smoking cessation attempts among current US smokers who also use smokeless tobacco[J]. Addict Behav, 2015, 51: 113-119. DOI:10.1016/j.addbeh.2015.06.045 |
| [16] |
McMillen R, Klein JD, Wilson K, et al. E-cigarette use and future cigarette initiation among never smokers and relapse among former smokers in the PATH study[J]. Public Health Rep, 2019, 134(5): 528-536. DOI:10.1177/0033354919864369 |
| [17] |
Velasco-Mondragon E, Jimenez A, Palladino-Davis AG, et al. Hispanic health in the USA: a scoping review of the literature[J]. Public Health Rev, 2016, 37: 31. DOI:10.1186/s40985-016-0043-2 |
| [18] |
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Social, environmental, cognitive, and genetic influences on the use of tobacco among youth[M]. Atlanta (GA): Centers for Disease Control and Prevention (US), 2012.
|
| [19] |
Collins SE, Witkiewitz K, Kirouac M, et al. Preventing relapse following smoking cessation[J]. Curr Cardio Risk Rep, 2010, 4(6): 421-428. DOI:10.1007/s12170-010-0124-6 |
| [20] |
Giovino GA, Mirza SA, Samet JM, et al. Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys[J]. Lancet, 2012, 380(9842): 668-679. DOI:10.1016/S0140-6736(12)61085-X |
| [21] |
Malas M, van der Tempel J, Schwartz R, et al. Electronic cigarettes for smoking cessation: a systematic review[J]. Nicotine Tob Res, 2016, 18(10): 1926-1936. DOI:10.1093/ntr/ntw119 |
| [22] |
Khoudigian S, Devji T, Lytvyn L, et al. The efficacy and short-term effects of electronic cigarettes as a method for smoking cessation: a systematic review and a meta-analysis[J]. Int J Public Health, 2016, 61(2): 257-267. DOI:10.1007/s00038-016-0786-z |
| [23] |
El Dib R, Suzumura EA, Akl EA, et al. Electronic nicotine delivery systems and/or electronic non-nicotine delivery systems for tobacco smoking cessation or reduction: a systematic review and meta-analysis[J]. BMJ Open, 2017, 7(2): e012680. DOI:10.1136/bmjopen-2016-012680 |
| [24] |
World Health Organization. WHO report on the global tobacco epidemic, 2021: addressing new and emerging products: executive summary[M/OL]. (2021-08-17)[2022-04-16]. https://www.who.int/publications/i/item/9789240032842.
|
 2022, Vol. 43
2022, Vol. 43