文章信息
- 任庆文, 杨飞飞, 韩天碧, 郭孟竹, 赵楠, 冯永亮, 杨海澜, 王素萍, 张亚玮, 邬惟为.
- Ren Qingwen, Yang Feifei, Han Tianbi, Guo Mengzhu, Zhao Nan, Feng Yongliang, Yang Hailan, Wang Suping, Zhang Yawei, Wu Weiwei
- 孕前体质指数和孕期增重与子痫前期及其临床亚型的关系
- Relationship between the pre-pregnancy BMI, gestational weight gain, and risk of preeclampsia and its subtypes
- 中华流行病学杂志, 2021, 42(11): 2037-2043
- Chinese Journal of Epidemiology, 2021, 42(11): 2037-2043
- http://dx.doi.org/10.3760/cma.j.cn112338-20210126-00072
-
文章历史
收稿日期: 2021-01-26
2. 中国医学科学院北京协和医学院北京协和医院医学科学研究中心, 北京 100730;
3. 山西医科大学第一医院妇产科, 太原 030001;
4. 国家癌症中心/国家肿瘤临床医学研究中心/中国医学科学院北京协和医学院肿瘤医院, 北京 100021
2. Medical Science Research Center, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences&Peking Union Medical College, Beijing 100730, China;
3. Department of Obstetrics and Gynecology, First Affiliated Hospital of Shanxi Medical University, Taiyuan 030001, China;
4. National Cancer Center/National Cancer Research Center/Cancer Hospital of Chinese Academy of Medical Sciences&Peking Union Medical College, Beijing 100021, China
子痫前期(preeclampsia,PE)是常见的妊娠特异性疾病,主要特征为妊娠20周后出现新发高血压和蛋白尿[1],是造成孕产妇及新生儿死亡的主要原因[2]。PE全球发病率为5%~8%[3],近年呈上升趋势[4],严重威胁孕妇和胎儿健康。作为一种多因素引起的复杂疾病,其发病机制尚不明确,已确定的一些影响因素包括孕妇年龄大、产次、孕前超重或肥胖、妊娠期间体重增加过度、妊娠期糖尿病和高血压家族史等[5]。有研究显示,孕前超重或肥胖与PE发生风险增加相关[5-12]。孕期增重与PE关系仍不明确,有研究表明孕期增重过多会增加PE发病风险[10, 12-21],也有研究显示,孕期增重与PE发生不相关或关联较弱[22-23]。目前已有研究分析早发型子痫前期(early-onset preeclampsia,EOPE)和晚发型子痫前期(late-onset preeclampsia,LOPE)的影响因素,提示我们关注孕前BMI和孕期增重[24-25]。本研究旨在评估孕前BMI和孕期增重对PE及其临床亚型发生风险的影响,为预防PE提供依据。
对象与方法1. 研究对象:以2013年3月至2016年9月于山西医科大学第一医院妇产科住院分娩的孕妇为研究对象。排除标准:死胎、死产、多胎、孕周 < 20周,除PE外的妊娠期高血压疾病(妊娠期高血压、子痫、妊娠合并慢性高血压、慢性高血压并发子痫前期)。共纳入9 274例孕妇,901例PE作为病例组,8 373例非PE作为对照组。本研究通过山西医科大学伦理委员会审查批准(批号:2014092),所有研究对象均签署知情同意书。
2. 研究方法:由培训合格的调查员于孕妇分娩后进行面对面问卷调查,并查阅相关病历信息。问卷内容包括一般人口学特征、孕前身高和体重、孕期生活方式、生育史和疾病史等。计算孕前BMI和孕期增重。
3. 诊断标准和定义:
(1)PE诊断标准:参照《妊娠期高血压疾病诊治指南(2015)》[26]。妊娠20周后出现SBP≥140 mmHg(1 mmHg=0.133 kPa)和(或)DBP≥90 mmHg,且伴有下列任一项:①尿蛋白≥0.3 g/24 h;②尿蛋白/肌酐比值≥0.3;③随机尿蛋白≥(+)(无法进行尿蛋白定量时的检查方法);④无蛋白尿但伴有以下任何一种器官或系统受累:心、肺、肝、肾等重要器官,或血液系统、消化系统、神经系统的异常改变,或胎盘-胎儿受到累及等。
(2)PE临床亚型:EOPE(孕周 < 34周)和LOPE(孕周≥34周)[27]。
根据疾病严重程度,PE可分为轻度子痫前期(mild preeclampsia,MPE)和重度子痫前期(severe preeclampsia,SPE)。PE孕妇出现下述任一表现即可诊断为SPE:①血压持续升高:SBP≥160 mmHg和(或)DBP≥110 mmHg;②持续性头痛、视觉障碍或其他中枢神经系统异常表现;③持续性上腹部疼痛及肝包膜下血肿或肝破裂表现;④肝酶异常:血ALT或AST水平升高;⑤肾功能受损:尿蛋白 > 2.0 g/24 h;少尿(24 h尿量 < 400 ml、或尿量 < 17 ml/h)、或血肌酐 > 106 μmol/L;⑥低蛋白血症伴腹水、胸水或心包积液;⑦血液系统异常:血小板计数呈持续性下降并低于100×109/L;微血管内溶血[表现有贫血、黄疸或血乳酸脱氢酶(LDH)水平升高];⑧心功能衰竭;⑨肺水肿;⑩胎儿生长受限或羊水过少、胎死宫内、胎盘早剥等。
(3)变量分组及定义:①孕前BMI:参照文献[28]分组:体重过低(BMI < 18.5 kg/m2);体重正常(18.5 kg/m2≤BMI < 24.0 kg/m2);超重/肥胖(BMI≥24.0 kg/m2)。②孕期增重:参照文献[29]分组:增重不足、增重适宜和增重过多。具体分组依据:孕前低体重女性孕期增重范围为12.5~18.0 kg,正常体重女性为11.5~16.0 kg,超重女性为7.0~11.5 kg,肥胖女性为5.0~9.0 kg。低于建议值范围为孕期增重不足,超过建议值范围为孕期增重过多,在范围内为孕期增重适宜。
4. 统计学分析:采用EpiData 3.1软件双录入数据,采用SAS 9.4软件清理及分析数据。采用χ2检验进行单因素分析,采用非条件logistic回归进行多因素分析。多因素分析时将单因素分析有意义的变量及现有研究已发现的PE影响因素作为调整因素。双侧检验,检验水准α=0.05。
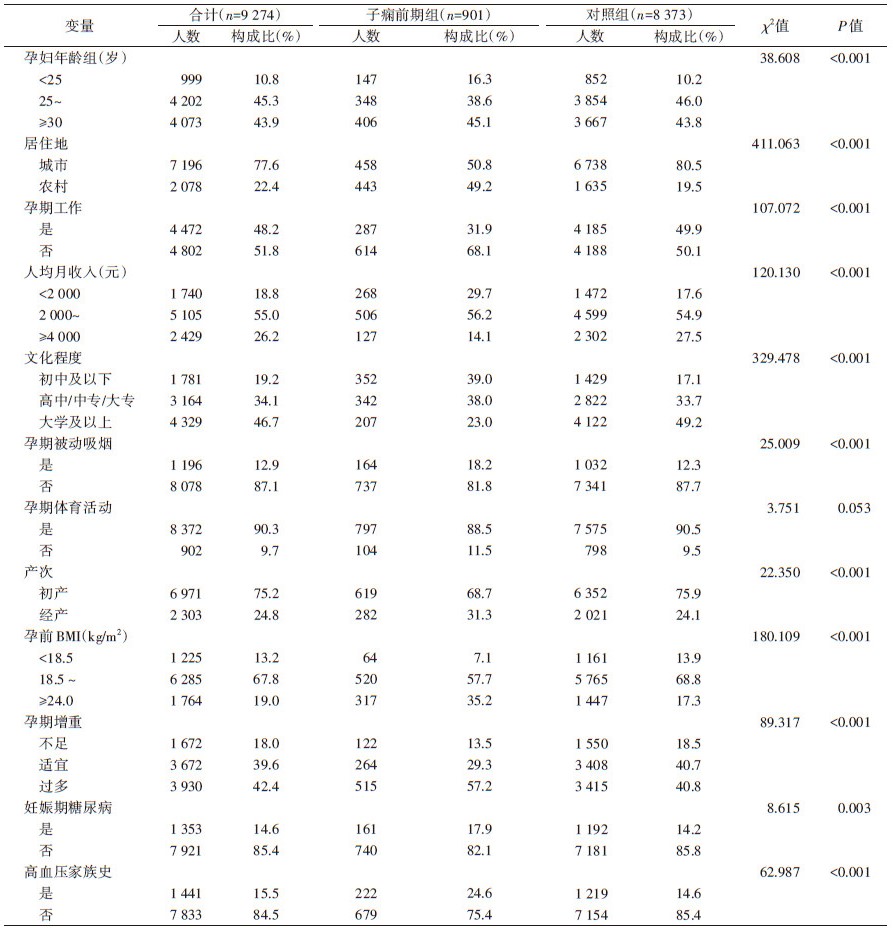
结果1. 一般人口学特征:共纳入9 274例孕妇,901例PE为病例组。孕妇年龄、居住地、孕期是否工作、人均月收入、文化程度、孕期被动吸烟、产次、妊娠期糖尿病和高血压家族史在两组间差异均有统计学意义(P < 0.05)。见表 1。
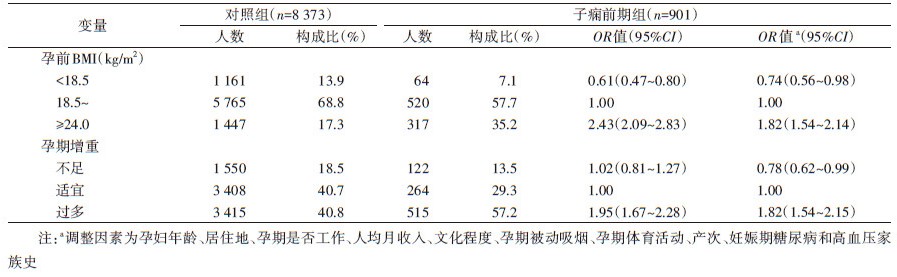
2. 孕前BMI和孕期增重与PE的关系:以孕妇是否患有PE(非PE=0,PE=1)作为因变量,调整变量后logistic回归分析结果显示,孕前BMI < 18.5 kg/m2和孕期增重不足是PE的保护因素(OR=0.74,95%CI:0.56~0.98;OR=0.78,95%CI:0.62~0.99);孕前BMI≥24.0 kg/m2和孕期增重过多是PE的危险因素(OR=1.82,95%CI:1.54~2.14;OR=1.82,95%CI:1.54~2.15)。见表 2。
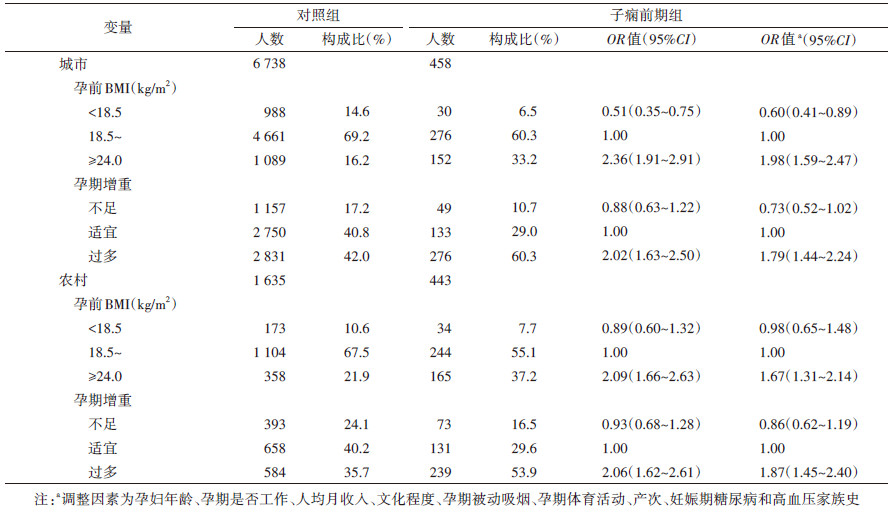
3. 不同居住地孕妇孕前BMI、孕期增重与PE的关系:考虑到研究对象来自省级三甲综合医院,较多PE病例可能从农村转诊来而产生转诊偏倚,故进一步按居住地进行分层分析。分析结果显示,城市孕妇中孕前BMI < 18.5 kg/m2是PE的保护因素;孕前BMI≥24.0 kg/m2和孕期增重过多是PE的危险因素;农村孕妇中孕前BMI≥24.0 kg/m2和孕期增重过多均是PE的危险因素。见表 3。
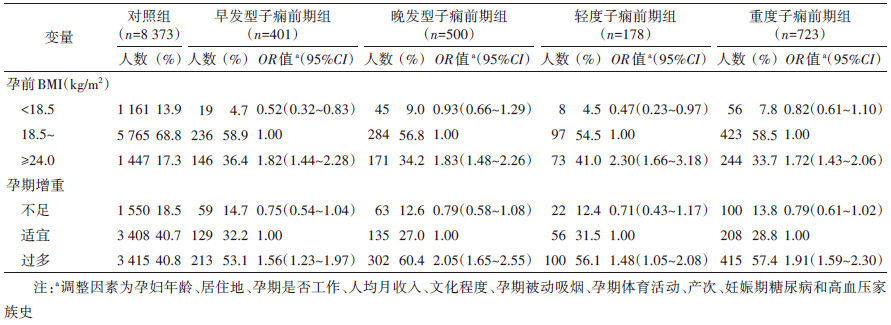
4. 孕前BMI和孕期增重与PE临床亚型的关系:根据发病时间,PE分为EOPE和LOPE。以EOPE和LOPE为病例组,调整变量后logistic回归分析结果显示,与体重正常组相比,孕前BMI < 18.5 kg/m2是EOPE的保护因素(OR=0.52,95%CI:0.32~0.83),孕前BMI≥24.0 kg/m2是EOPE和LOPE的危险因素(OR=1.82,95%CI:1.44~2.28;OR=1.83,95%CI:1.48~2.26);与孕期增重适宜相比,孕期增重过多是EOPE和LOPE的危险因素(OR=1.56,95%CI:1.23~1.97;OR=2.05,95%CI:1.65~2.55)。见表 4。
根据疾病严重程度,PE分为MPE和SPE。以MPE和SPE为病例组,调整变量后logistic回归分析结果显示,与体重正常组相比,孕前BMI < 18.5 kg/m2是MPE的保护因素(OR=0.47,95%CI:0.23~0.97),孕前BMI≥24.0 kg/m2是MPE和SPE的危险因素(OR=2.30,95%CI:1.66~3.18;OR=1.72,95%CI:1.43~2.06);与孕期增重适宜相比,孕期增重过多是MPE和SPE的危险因素(OR=1.48,95%CI:1.05~2.08;OR=1.91,95%CI:1.59~2.30)。
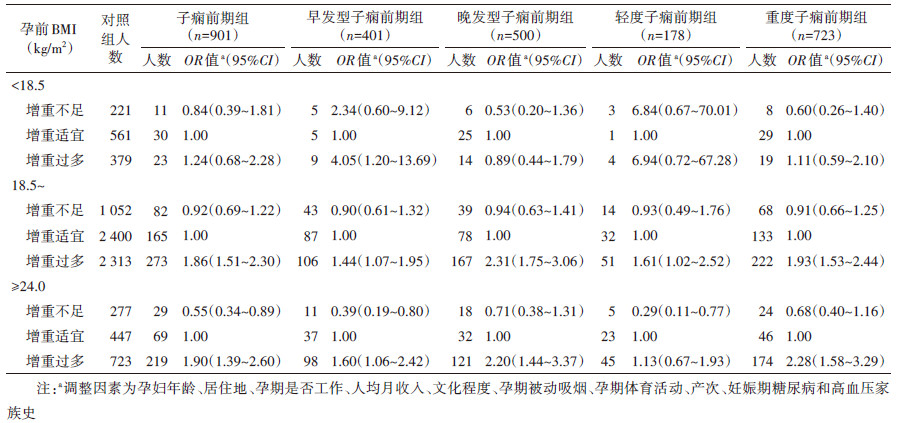
5. 不同孕前BMI分层下孕期增重与PE及其临床亚型的关系:以PE为病例组,孕前18.5 kg/m2≤BMI < 24.0 kg/m2的孕妇中孕期增重过多会增加PE发病风险;孕前BMI≥24.0 kg/m2的孕妇中孕期增重不足是PE的保护因素,孕期增重过多是PE的危险因素。进一步以PE各临床亚型分别作为病例组,结果显示:孕前BMI < 18.5 kg/m2的孕妇中孕期增重过多是EOPE的危险因素;孕前18.5 kg/m2≤BMI < 24.0 kg/m2的孕妇中孕期增重过多与4种PE临床亚型的发生风险增加均有关;孕前BMI≥24.0 kg/m2的孕妇中孕期增重不足是EOPE和MPE的保护因素,孕期增重过多是EOPE、LOPE和SPE的危险因素。见表 5。
PE是常见的妊娠特异性疾病,会导致不良妊娠结局发生,严重威胁孕妇和胎儿健康。目前研究表明PE的发生受孕妇年龄大、产次、妊娠期糖尿病和高血压家族史等多种因素影响[5],但病因及发病机制仍不明确。本研究评估了孕前BMI和孕期增重与PE及其临床亚型的关系,以期为预防PE提供依据。
国内外研究表明,孕前超重或肥胖与PE风险增加相关[5-11]。本研究结果显示,与孕前体重正常组相比,PE孕妇中孕前BMI≥24.0 kg/m2者占35.2%,PE发生风险明显增加,与既往研究结论一致;孕期增重过多是PE的危险因素,可能是孕期增重过多导致超重或肥胖,而超重或肥胖者常伴有内分泌紊乱、血脂增高、前列环素分泌减少和过氧化物酶增多等情况,可引起血管收缩、血小板聚集,诱发血压升高和PE。以往多数相关研究也表明孕期增重会增加PE发生风险[10, 14-18],而少数研究表明二者不相关[21-22]。可能是不同研究中PE临床亚型存在差异,或在考虑孕期增重对PE的影响时未能结合孕前BMI。
本研究根据发病时间和疾病严重程度分别对PE进行分型,结果表明孕前BMI≥24.0 kg/m2及孕期增重过多是PE各临床亚型的危险因素。一项意大利的研究表明分娩前BMI > 35 kg/m2和孕期体重增加过多是LOPE的危险因素[23],另一项泰国的研究中孕前BMI≥25 kg/m2和每周体重增加≥0.5 kg均是EOPE和LOPE的危险因素[24]。
进一步分析不同孕前BMI下孕期增重对PE及其临床亚型的作用后结果表明不同孕前BMI下孕期增重过多均是PE临床亚型的危险因素;而孕前超重或肥胖的孕妇中,孕期增重不足是PE、EOPE和MPE的保护因素。提示应严格控制孕期体重变化,防止增长过度增加PE发病风险。一项关于妊娠期体重增加对肥胖女性妊娠期高血压发展影响的研究中表明,低于建议的妊娠体重增加并不能降低肥胖孕妇PE的发病风险[13],而另一项研究结果表明肥胖女性妊娠期体重增加不足时,其PE发生风险降低,正常或超重/肥胖女性妊娠期体重增加过多会增加PE发病风险[18],后者与我们结论一致。此外Bodnar等[30]利用医院数据库开展的一项病例对照研究中,孕前BMI正常的女性,妊娠早期体重增加过多会增加PE发病风险。
本研究通过查阅病历并参照《妊娠期高血压疾病诊治指南(2015年)》诊断PE,减少信息偏倚;其次采用标准化问卷获取相关信息并控制潜在混杂因素;本研究考虑了不同孕前BMI下孕期增重对PE的影响且进行了PE亚型分析,较为全面。
本研究存在局限性。研究对象仅来自一家医院,对PE的发生情况代表性有限,未来可采用多中心大样本的研究设计;尽管控制了混杂因素,但不排除存在残余混杂的可能,如营养素缺乏、慢性肾炎等也影响着PE的发生,但鉴于本研究未收集到相关资料,所以未能调整,今后可继续完善。
综上所述,孕妇孕前超重/肥胖及孕期增重过多均会增加PE及其临床亚型发生风险,且孕期增重多少的影响因孕前BMI而异。故建议育龄女性在孕前通过合理饮食和适宜锻炼来保持健康体重;此外应加强孕期健康教育,在保证孕妇和胎儿营养需求的前提下控制孕妇孕期体重增加幅度,以减少PE发生。
利益冲突 所有作者均声明不存在利益冲突
| [1] |
Mol BWJ, Roberts CT, Thangaratinam S, et al. Pre-eclampsia[J]. Lancet, 2016, 387(10022): 999-1011. DOI:10.1016/s0140-6736(15)00070-7 |
| [2] |
MacKay AP, Berg CJ, Atrash HK. Pregnancy-related mortality from preeclampsia and eclampsia[J]. Obstetr Gynecol, 2001, 97(4): 533-538. DOI:10.1016/S0029-7844(00)01223-0 |
| [3] |
Souza JP, Gülmezoglu AM, Vogel J, et al. Moving beyond essential interventions for reduction of maternal mortality (the WHO Multicountry Survey on Maternal and Newborn Health): a cross-sectional study[J]. Lancet, 2013, 381(9879): 1747-1755. DOI:10.1016/S0140-6736(13)60686-8 |
| [4] |
Abalos E, Cuesta C, Grosso AL, et al. Global and regional estimates of preeclampsia and eclampsia: a systematic review[J]. Eur J Obstet Gynecol Reprod Biol, 2013, 170(1): 1-7. DOI:10.1016/j.ejogrb.2013.05.005 |
| [5] |
Jeyabalan A. Epidemiology of preeclampsia: impact of obesity[J]. Nutr Rev, 2013, 71(Suppl 1): S18-25. DOI:10.1111/nure.12055 |
| [6] |
Villamor E, Cnattingius S. Interpregnancy weight change and risk of adverse pregnancy outcomes: a population-based study[J]. Lancet, 2006, 368(9542): 1164-1170. DOI:10.1016/s0140-6736(06)69473-7 |
| [7] |
Wei YM, Yang HX, Zhu WW, et al. Risk of adverse pregnancy outcomes stratified for pre-pregnancy body mass index[J]. J Matern Fetal Neonatal Med, 2016, 29(13): 2205-2209. DOI:10.3109/14767058.2015.1081167 |
| [8] |
Vinturache A, Moledina N, McDonald S, et al. Pre-pregnancy Body Mass Index (BMI) and delivery outcomes in a Canadian population[J]. BMC Pregnancy Childbirth, 2014, 14: 422. DOI:10.1186/s12884-014-0422-y |
| [9] |
Liu XM, Du J, Wang GX, et al. Effect of pre-pregnancy body mass index on adverse pregnancy outcome in north of China[J]. Arch Gynecol Obstet, 2011, 283(1): 65-70. DOI:10.1007/s00404-009-1288-5 |
| [10] |
Liu L, Hong ZX, Zhang LH. Associations of prepregnancy body mass index and gestational weight gain with pregnancy outcomes in nulliparous women delivering single live babies[J]. Sci Rep, 2015, 5: 12863. DOI:10.1038/srep12863 |
| [11] |
Paré E, Parry S, McElrath TF, et al. Clinical risk factors for preeclampsia in the 21st century[J]. Obstet Gynecol, 2014, 124(4): 763-770. DOI:10.1097/aog.0000000000000451 |
| [12] |
Tabatabaei M. Gestational weight gain, prepregnancy body mass index related to pregnancy outcomes in KAZERUN, FARS, IRAN[J]. J Prenat Med, 2011, 5(2): 35-40. |
| [13] |
Barton JR, Joy SD, Rhea DJ, et al. The influence of gestational weight gain on the development of gestational hypertension in obese women[J]. Am J Perinatol, 2015, 32(7): 615-620. DOI:10.1055/s-0034-1386634 |
| [14] |
Baker AM, Haeri S. Estimating risk factors for development of preeclampsia in teen mothers[J]. Arch Gynecol Obstet, 2012, 286(5): 1093-1096. DOI:10.1007/s00404-012-2418-z |
| [15] |
Truong YN, Yee LM, Caughey AB, et al. Weight gain in pregnancy: Does the Institute of Medicine have it right?[J]. Am J Obstet Gynecol, 2015, 212(3): 362. DOI:10.1016/j.ajog.2015.01.027 |
| [16] |
Flick AA, Brookfield KF, de La Torre L, et al. Excessive weight gain among obese women and pregnancy outcomes[J]. Am J Perinatol, 2010, 27(4): 333-338. DOI:10.1055/s-0029-1243304 |
| [17] |
Langford A, Joshu C, Chang JJ, et al. Does gestational weight gain affect the risk of adverse maternal and infant outcomes in overweight women?[J]. Matern Child Health J, 2011, 15(7): 860-865. DOI:10.1007/s10995-008-0318-4 |
| [18] |
Cedergren M. Effects of gestational weight gain and body mass index on obstetric outcome in Sweden[J]. Int J Gynecol Obstet, 2006, 93(3): 269-274. DOI:10.1016/j.ijgo.2006.03.002 |
| [19] |
Haugen M, Brantsæter AL, Winkvist A, et al. Associations of pre-pregnancy body mass index and gestational weight gain with pregnancy outcome and postpartum weight retention: a prospective observational cohort study[J]. BMC Pregnancy Childbirth, 2014, 14: 201. DOI:10.1186/1471-2393-14-201 |
| [20] |
deVader SR, Neeley HL, Myles TD, et al. Evaluation of gestational weight gain guidelines for women with normal prepregnancy body mass index[J]. Obstetr Gynecol, 2007, 110(4): 745-751. DOI:10.1097/01.Aog.0000284451.37882.85 |
| [21] |
O'Dwyer V, O'Toole F, Darcy S, et al. Maternal obesity and gestational weight gain[J]. J Obstet Gynaecol, 2013, 33(7): 671-674. DOI:10.3109/01443615.2013.821461 |
| [22] |
Gaillard R, Durmuş B, Hofman A, et al. Risk factors and outcomes of maternal obesity and excessive weight gain during pregnancy[J]. Obesity (Silver Spring, Md), 2013, 21(5): 1046-1055. DOI:10.1002/oby.20088 |
| [23] |
Ornaghi S, Tyurmorezova A, Algeri P, et al. Influencing factors for late-onset preeclampsia[J]. J Matern Fetal Neonatal Med, 2013, 26(13): 1299-1302. DOI:10.3109/14767058.2013.783807 |
| [24] |
Aksornphusitaphong A, Phupong V. Risk factors of early and late onset pre-eclampsia[J]. J Obstet Gynaecol Res, 2013, 39(3): 627-631. DOI:10.1111/j.1447-0756.2012.02010.x |
| [25] |
Mbah AK, Kornosky JL, Kristensen S, et al. Super-obesity and risk for early and late pre-eclampsia[J]. BJOG, 2010, 117(8): 997-1004. DOI:10.1111/j.1471-0528.2010.02593.x |
| [26] |
杨孜, 张为远. 妊娠期高血压疾病诊治指南(2015)解读[J]. 中国实用妇科与产科杂志, 2015, 31(10): 886-893. Yang Z, Zhang WY. Understanding Society of obstetrics and gynecology of Chinese medical association guideline for the management of hypertensive disorders of pregnancy[J]. Chin J Pract Gynecol Obstetr, 2015, 31(10): 886-893. DOI:10.7504/fk2015090102 |
| [27] |
Lindheimer MD, Taler SJ, Cunningham FG. Hypertension in pregnancy[J]. J Am Soc Hypertens, 2010, 4(2): 68-78. DOI:10.1016/j.jash.2010.03.002 |
| [28] |
中国肥胖问题工作组数据汇总分析协作组. 我国成人体重指数和腰围对相关疾病危险因素异常的预测价值: 适宜体重指数和腰围切点的研究[J]. 中华流行病学杂志, 2002, 23(1): 5-10. Collaborative Group for Data Collection and Analysis of China Obesity Working Group. Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population[J]. Chin J Epidemiol, 2002, 23(1): 5-10. DOI:10.3760/j.issn:0254-6450.2002.01.003 |
| [29] |
Rasmussen KM, Yaktine AL. Weight gain during pregnancy: reexamining the guidelines[M]. Washington DC: National Academies Press, 2009.
|
| [30] |
Bodnar LM, Himes KP, Abrams B, et al. Early-pregnancy weight gain and the risk of preeclampsia: A case-cohort study[J]. Pregnancy Hypertens, 2018, 14: 205-212. DOI:10.1016/j.preghy.2018.10.005 |
 2021, Vol. 42
2021, Vol. 42