文章信息
- 俞海亮, 杨跃诚, 赵燕, 曹东冬, 金聪, 叶润华, 曹艳芬, 刘雪娇, 姚仕堂, 陈晨, 段松, 吴尊友.
- Yu Hailiang, Yang Yuecheng, Zhao Yan, Cao Dongdong, Jin Cong, Ye Runhua, Cao Yanfen, Liu Xuejiao, Yao Shitang, Chen Chen, Duan Song, Wu Zunyou
- 德宏傣族景颇族自治州成年人HIV/AIDS抗病毒治疗后CD4+T淋巴细胞免疫重建及影响因素分析
- Prevalence and related factors of CD4+T lymphocytes immune recovery among adult HIV/AIDS on antiretroviral therapy in Dehong Dai and Jingpo Autonomous Prefecture
- 中华流行病学杂志, 2021, 42(6): 1050-1055
- Chinese Journal of Epidemiology, 2021, 42(6): 1050-1055
- http://dx.doi.org/10.3760/cma.j.cn112338-20210326-00250
-
文章历史
收稿日期: 2021-03-26
2. 德宏傣族景颇族自治州疾病预防控制中心, 芒市 678400;
3. 德宏傣族景颇族自治州人民医院公共卫生科, 芒市 678400;
4. 中国疾病预防控制中心环境与健康相关产品安全所环境流行病学室, 北京 100021
2. Dehong Dai and Jingpo Autonomous Prefecture Center for Disease Control and Prevention, Mangshi 678400, China;
3. Department of Public Health, Dehong Dai and Jingpo Autonomous Prefecture People's Hospital, Mangshi 678400, China;
4. Department of Environmental Epidemiology, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing 100021, China
HIV感染人体后主要引起CD4+T淋巴细胞(CD4)进行性减少、黏膜屏障功能受损和异常的免疫激活。抗病毒治疗(ART)通过抑制HIV复制重建HIV/AIDS的免疫系统,显著提高CD4水平[1-3]。不同HIV/AIDS的CD4随ART时间恢复程度并不一致,呈现不同变化规律[4],有些可恢复或接近至正常值水平(> 500个/μl)[5]。HIV/AIDS中约10%~40%虽然病毒载量抑制成功,但却一直未能恢复至CD4正常值水平[6-7]。有研究发现,CD4免疫重建不良与HIV/AIDS死亡等结局相关[8-10]。已有研究发现,HIV/AIDS性别、感染途径、开始ART时年龄、CD4、CD4/CD8比值等是CD4免疫重建的影响因素[8, 11-15]。ART后HIV/AIDS的CD4恢复情况呈现不同的变化规律[11, 16]。本研究分析德宏傣族景颇族自治州(德宏州)ART后成年人HIV/AIDS的CD4免疫重建及其影响因素,为改善ART效果和提高HIV/AIDS生存质量提供参考依据。
对象与方法1. 研究对象:来源于艾滋病防治工作信息系统德宏州2007年1月1日至2018年12月31日数据库,包括ART基线和随访数据库。德宏州2007-2016年开始ART的HIV/AIDS,随访至2018年12月31日。①入选标准:开始ART时年龄≥18岁,随访≥1次;②排除标准:基线CD4资料缺失,或CD4检测 < 2次,或民族、职业、文化程度等信息缺失。ART基线库共10 900例,排除不符合研究者,纳入7 605例HIV/AIDS。
2. 研究方法与内容:
(1)基本信息:开始ART时年龄、性别、民族、文化程度、感染途径、机会性感染、WHO临床分期、确诊时间、ART方案、开始ART时间、基线与随访CD4、CD4/CD8比值、血红蛋白水平、最终随访状态等。
(2)相关定义:免疫重建良好[5]为HIV/AIDS经ART后CD4恢复至基本正常(> 500个/μl)。
(3)CD4变化组:①CD4未恢复正常组:ART第5年时或随访时间 < 5年时,最近1次CD4≤500个/μl;②CD4基本恢复正常组:ART第3~5年后CD4 > 500个/μl;③CD4恢复正常组:ART后第1~2年时CD4 > 500个/μl;④CD4维持正常组:ART基线及随访时CD4 > 500个/μl。
3. 统计学分析:采用SAS 9.4软件进行统计学分析。
(1)基本情况:计数资料采用例数和构成比(%)描述,计量资料符合正态分布采用x±s描述,符合偏态分布的采用M(P25,P75)描述。采用χ2检验、非参数检验等方法比较不同CD4分组的人口学特征、ART基线、CD4增加值和随访结局等情况。绘制各组CD4中位数随访时间变化趋势图。
(2)ART后CD4免疫重建情况:采用轨迹分析模型(group-based trajectory model,GBTM)分析随访数据的基本思路是假定多次测量的变量存在异质性(即总体中存在多个不同发展轨迹的分组),不同组间具有不同的变化轨迹,但同一组内个体具有相同变化轨迹,利用最大似然估计方法确定分组数[17-21]。当HIV/AIDS在某个随访年内有多次CD4值时,纳入分析最后1次数值。对CD4拟合删截正态分布,以贝叶斯信息准则(BIC)作为评价模型拟合效果的参考。比较不同组数模型间的BIC值,BIC越接近0,表示该模型的拟合效果越好[22]。
(3)ART后CD4变化轨迹分组的影响因素分析:采用无序多分类logistic回归模型,以CD4分组作为应变量,将开始ART时年龄、性别、民族、文化程度、感染途径、ART基线是否有机会性感染、WHO临床分期、CD4、CD4/CD8比值、血红蛋白水平、ART方案、开始ART时间、HIV确诊至ART时间等分类变量为自变量,进行单因素和多因素logistic回归分析,多因素分析时采用逐步法和专业知识筛选变量。双侧检验,检验水准α=0.05(如做多组比较,检验水准则调整为α/比较次数)。
结果1. 基本情况:共7 605例HIV/AIDS,开始ART年龄M(P25,P75)为36(30,43)岁,男性4 641例(61.0%),汉族3 232例(42.5%),小学及以下文化程度4 624例(60.8%),随访时间M(P25,P75)为6.1(4.1,8.1)年。最长随访12年。最终随访状态为在治者5 977例(78.6%),2012年及以后开始ART者4 028例(53.0%)。见表 1。
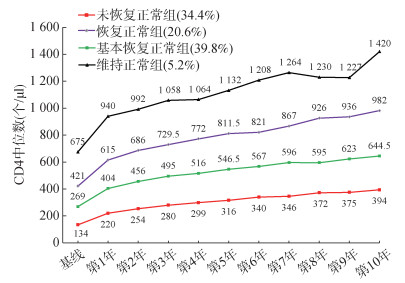
2. ART后CD4分组:CD4未恢复正常组、CD4基本恢复正常组、CD4恢复正常组和CD4维持正常组的构成比分别为34.4%(2 617)、39.8%(3 030)、20.6%(1 562)和5.2%(396)。CD4未恢复正常组的M在ART第10年时为394个/μl;CD4基本恢复正常组的M在ART第5年 > 500个/μl;CD4恢复正常组的M在第1年 > 500个/μl;CD4维持正常组的基线及随访CD4均 > 500个/μl。
总体上,4个组HIV/AIDS的CD4值随ART时间延长而增加,其中,ART第1年的增长速度最快,之后逐渐降低。与基线CD4的M相比,CD4未恢复正常组、CD4基本恢复正常组、CD4恢复正常组和CD4维持正常组在ART第1年CD4的M分别增加了86、135、194和265个/μl,ART第3年CD4的M分别增加了146、226、308.5和383个/μl。CD4未恢复正常组与其他3个组比较,基线和随访CD4的M增加值均相对较低。见图 1。
|
| 图 1 2007-2016年德宏傣族景颇族自治州开始抗病毒治疗HIV/AIDS CD4+T淋巴细胞纵向变化分组 |
与CD4未恢复正常组相比,CD4基本恢复正常组、CD4恢复正常组和CD4维持正常组的年龄 < 35岁(48.6%、51.7%和59.3%)、女性(41.8%、47.1%和41.7%)、注射吸毒传播途径(71.2%、78.0%和73.0%)、基线无机会性感染(85.9%、93.7%和96.5%)、WHO临床分期为Ⅰ和Ⅱ期(57.1%、72.1%和75.0%)、CD4水平≥350个/μl(23.3%、66.4%和90.7%)、CD4/CD8比值≥1.0(1.5%、2.9%和6.3%)、血红蛋白≥110 g/L(83.1%、88.0%和90.7%)、ART方案[替诺福韦(TDF)+拉米夫定(3TC)+依非韦伦(EFV)/奈韦拉平(NVP)](32.2%、50.0%和55.8%)的比例相对较多。见表 1。
CD4未恢复正常组、CD4基本恢复正常组、CD4恢复正常组和CD4维持正常组最终随访状态为死亡的比例分别为20.7%、9.5%、6.1%和6.1%(χ2=267.4,P < 0.000 1),而艾滋病相关死亡的比例分别为9.4%、2.8%、1.4%和1.5%,差异均有统计学意义(χ2=200.7,P < 0.000 1)。
3. ART后CD4变化轨迹分组的影响因素分析:无序多分类logistic回归模型分析结果显示,以CD4未恢复正常组作为对照组相比,开始ART年龄 < 35岁、女性、中学及以上文化程度、性传播感染途径、基线无机会性感染、开始ART时CD4≥200个/μl、含TDF标准的ART方案、确诊到开始ART时间 < 1年是促进HIV/AIDS的CD4免疫重建良好的影响因素。CD4基本恢复正常组、CD4恢复正常组和CD4维持正常组这3个组中,相比于基线CD4 < 200个/μl者,基线CD4为200~个/μl、≥350个/μl者分别是其CD4恢复正常水平的4.66和45.33倍、12.86和579.72倍、18.21和 > 999.9倍。见表 1。
讨论本研究发现,德宏州7 605例ART后HIV/AIDS,开始ART年龄M=36岁,男性、汉族、小学及以下文化程度分别占61.0%、42.5%、60.8%,随访时间M=6.1年。ART后HIV/AIDS的CD4分4个组描述其免疫重建情况,CD4未恢复正常组、CD4基本恢复正常组、CD4恢复正常组和CD4维持正常组分别占34.4%、39.8%、20.6%和5.2%。
总体上,4个组的CD4值随ART时间延长而增加,且ART第1年的增长速度最快,之后逐渐降低,这与其他相关研究结果基本一致[15, 23-24]。说明ART对提高HIV/AIDS的CD4水平非常重要,且不论其基线CD4水平或病程阶段,均可提高CD4水平,这为HIV/AIDS的ART依从性教育提供了参考依据。
本研究采用GBTM方法,相比于常规方法未考虑多次随访CD4水平,更稳定、更全面地反映CD4水平纵向变化的特征[21, 25-26],在一些MSM毒品使用、HIV/AIDS随访、病毒载量变化等研究中均有运用[27-31],GBTM比混合效应模型更加直观[15, 24]。运用GBTM探索纵向队列研究指标的聚类分析,可降低CD4离散值随时间变化的影响。
本研究发现,研究对象中CD4未恢复正常组占34.4%,这与法国、日本的相关研究结果类似[13-14],但低于中国香港地区的研究结果[12],这可能和观察时长及基线CD4水平相关。CD4未恢复正常组与其他3个组比较,基线和随访CD4的M增加值均相对较低。也说明ART后HIV/AIDS的CD4水平和增加趋势与其免疫重建有相对一致性。
多因素logistic回归分析结果显示,基线CD4水平是重要的影响因素。CD4基本恢复正常组、CD4恢复正常组和CD4维持正常组这3个组中,相比于基线CD4 < 200个/μl者,基线CD4为200~个/μl和≥350个/μl者的CD4免疫重建可能性是其4.66倍及以上,这与相关研究发现的基线CD4水平较高者其预后效果较好的研究结论相一致[15, 24, 32-33]。本研究发现,CD4恢复正常组和CD4维持正常组的最终随访状态为死亡及艾滋病相关死亡的比例均较低,可能是这两组基线CD4水平较高,容易接近普通健康人的预期寿命[34-36],也可能是本研究随访时间较短。
本研究发现,与CD4未恢复正常组相比(37.4%),年龄 < 35岁者在CD4基本恢复正常组、CD4恢复正常组和CD4维持正常组的比例较多(48.6%、51.7%和59.3%)。这可能是免疫功能随年龄增长而逐渐衰退、进展阶段CD4异常化等因素有关[7]。而CD4未恢复正常组中,男性(69.6%)、其他民族(55.3%)、小学及以下文化程度(60.8%)的比例较多,提示需关注ART的HIV/AIDS的男性、文化程度较低者的随访CD4水平。另外,CD4未恢复正常组中,ART方案为AZT+3TC+EFV/NVP比TDF+3TC+EFV/NVP的比例较多(44.2%比27.2%),提示含AZT比含TDF的一线标准ART方案的CD4免疫重建可能性更小,可能与不同ART方案效果或不良反应有关。
本研究存在不足。①存在信息偏倚,不同时间的CD4水平受不同检测仪器、人员等影响,对CD4检测异常值进行复核,可减少这方面偏倚。②未考虑随访出现脱失、随访时间对CD4分组的影响。③未考虑我国免费ART指南及标准的发展和变化。④未考虑病毒载量对CD4水平的影响,未排除病毒载量抑制失败者,有可能高估CD4未恢复正常者的比例。⑤未考虑HIV基因亚型分子水平的影响。
综上所述,德宏州ART后HIV/AIDS的CD4免疫重建情况呈多种状况,在基线CD4较高水平时开始ART有助于CD4恢复至正常水平。建议尽早开始ART,注意随访和关注CD4水平变化。
利益冲突 所有作者均声明不存在利益冲突
志谢 感谢德宏州及市(县)相关工作人员和研究对象的支持
| [1] |
杨跃诚, 段松, 项丽芬, 等. 云南省德宏州1989-2011年HIV感染者死亡率及其影响因素研究[J]. 中华流行病学杂志, 2012, 33(10): 1026-1030. Yang YC, Duan S, Xiang LF, et al. Study on the mortality and risk factors among HIV-infected individuals during 1989-2011 in Dehong prefecture, Yunnan province[J]. Chin J Epidemiol, 2012, 33(10): 1026-1030. DOI:10.3760/cma.j.issn.0254-6450.2012.10.007 |
| [2] |
姚仕堂, 项丽芬, 李艳玲, 等. 云南省德宏州1039例成人艾滋病患者抗病毒治疗效果评价[J]. 中华传染病杂志, 2010, 28(9): 551-554. Yao ST, Xiang LF, Li YL, et al. Assessment of the effectiveness of highly active antiretroviral therapy in 1039 adult acquired immune deficiency syndrome patients in Dehong area, Yunnan Province[J]. Chin J Infect Dis, 2010, 28(9): 551-554. DOI:10.3760/cma.j.issn.1000-6680.2010.09.010 |
| [3] |
Zhang FJ, Dou ZH, Ma Y, et al. Five-year outcomes of the China national free antiretroviral treatment program[J]. Ann Intern Med, 2009, 151(4): I-42. DOI:10.7326/0003-4819-151-4-200908180-00003 |
| [4] |
The Opportunistic Infections Project Team of the Collaboration of Observational HIV Epidemiological Research in Europe (COHERE) in Euro Coord. CD4 cell count and the risk of AIDS or death in HIV-Infected adults on combination antiretroviral therapy with a suppressed viral load: a longitudinal cohort study from COHERE[J]. PLoS Med, 2012, 9(3): e1001194. DOI:10.1371/journal.pmed.1001194 |
| [5] |
Department of Health and Human Services Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV[DB/OL]. [2020-09-20]. https://clinicalinfo.hiv.gov/sites/default/files/inline-files/AdultandAdolescentGL.pdf.
|
| [6] |
Yang XD, Su B, Zhang X, et al. Incomplete immune reconstitution in HIV/AIDS patients on antiretroviral therapy: Challenges of immunological non-responders[J]. J Leukoc Biol, 2020, 107(4): 597-612. DOI:10.1002/JLB.4MR1019-189R |
| [7] |
杨小东, 粟斌, 张彤. HIV-1感染者免疫重建不良研究进展[J]. 国际病毒学杂志, 2020, 27(1): 82-85. Yang XD, Su B, Zhang T. Review of studies on HIV-1 immunological non-responders[J]. Int J Virol, 2020, 27(1): 82-85. DOI:10.3760/cma.j.issn.1673-4092.2020.01.020 |
| [8] |
Engsig FN, Zangerle R, Katsarou O, et al. Long-term mortality in HIV-positive individuals virally suppressed for >3 years with incomplete CD4 recovery[J]. Clin Infect Dis, 2014, 58(9): 1312-1321. DOI:10.1093/cid/ciu038 |
| [9] |
Brennan AT, Maskew M, Sanne I, et al. The interplay between CD4 cell count, viral load suppression and duration of antiretroviral therapy on mortality in a resource-limited setting[J]. Trop Med Int Health, 2013, 18(5): 619-631. DOI:10.1111/tmi.12079 |
| [10] |
Ingle SM, May MT, Gill MJ, et al. Impact of risk factors for specific causes of death in the first and subsequent years of antiretroviral therapy among HIV-infected patients[J]. Clin Infect Dis, 2014, 59(2): 287-297. DOI:10.1093/cid/ciu261 |
| [11] |
Kufa T, Shubber Z, MacLeod W, et al. CD4 count recovery and associated factors among individuals enrolled in the South African antiretroviral therapy programme: An analysis of national laboratory based data[J]. PLoS One, 2019, 14(5): e0217742. DOI:10.1371/journal.pone.0217742 |
| [12] |
Lee SS, Wong NS, Wong BCK, et al. Combining CD4 recovery and CD4:CD8 ratio restoration as an indicator for evaluating the outcome of continued antiretroviral therapy: an observational cohort study[J]. BMJ Open, 2017, 7(9): e016886. DOI:10.1136/bmjopen-2017-016886 |
| [13] |
Roul H, Mary-Krause M, Ghosn J, et al. CD4+ cell count recovery after combined antiretroviral therapy in the modern combined antiretroviral therapy era[J]. AIDS, 2018, 32(17): 2605-2614. DOI:10.1097/QAD.0000000000002010 |
| [14] |
Li CX, Li YY, He LP, et al. The predictive role of CD4+ cell count and CD4/CD8 ratio in immune reconstitution outcome among HIV/AIDS patients receiving antiretroviral therapy: an eight-year observation in China[J]. BMC Immunol, 2019, 20(1): 31. DOI:10.1186/s12865-019-0311-2 |
| [15] |
Pantazis N, Papastamopoulos V, Paparizos V, et al. Long-term evolution of CD4+ cell count in patients under combined antiretroviral therapy[J]. AIDS, 2019, 33(10): 1645-1655. DOI:10.1097/QAD.0000000000002248 |
| [16] |
Gezie LD. Predictors of CD4 count over time among HIV patients initiated ART in Felege Hiwot Referral Hospital, northwest Ethiopia: multilevel analysis[J]. BMC Res Notes, 2016, 9: 377. DOI:10.1186/s13104-016-2182-4 |
| [17] |
Nagin DS, Jones BL, Passos VL, et al. Group-based multi-trajectory modeling[J]. Stat Methods Med Res, 2018, 27(7): 2015-2023. DOI:10.1177/0962280216673085 |
| [18] |
Jones BL, Nagin DS, Roeder K. A SAS Procedure based on mixture models for estimating developmental trajectories[J]. Sociol Methods Res, 2001, 29(3): 374-393. DOI:10.1177/0049124101029003005 |
| [19] |
Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them[J]. Sociol Methods Res, 2007, 35(4): 542-571. DOI:10.1177/0049124106292364 |
| [20] |
冯国双, 于石成, 刘世炜. 轨迹分析模型在追踪数据分析中的应用[J]. 中国预防医学杂志, 2014, 15(3): 292-295. Feng GS, Yu SC, Liu SW. The application of trajectory model in longitudinal data analysis[J]. Chin Prev Med, 2014, 15(3): 292-295. DOI:10.16506/j.1009-6639.2014.03.009 |
| [21] |
冯国双, 于石成, 胡跃华. 轨迹分析模型在流行病学研究中的应用[J]. 中华流行病学杂志, 2014, 35(7): 865-867. Feng GS, Yu SC, Hu YH. The application of trajectory model in epidemiological research[J]. Chin J Epidemiol, 2014, 35(7): 865-867. DOI:10.3760/cma.j.issn.0254-6450.2014.07.024 |
| [22] |
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research[J]. Annu Rev Clin Psychol, 2010, 6: 109-138. DOI:10.1146/annurev.clinpsy.121208.131413 |
| [23] |
Lok JJ, Bosch RJ, Benson CA, et al. Long-term increase in CD4+ T-cell counts during combination antiretroviral therapy for HIV-1 infection[J]. AIDS, 2010, 24(12): 1867-1876. DOI:10.1097/QAD.0b013e32833adbcf |
| [24] |
Means AR, Risher KA, Ujeneza EL, et al. Impact of age and sex on CD4+ cell count trajectories following Treatment Initiation: an analysis of the Tanzanian HIV treatment database[J]. PLoS One, 2016, 11(11): e0164148. DOI:10.1371/journal.pone.0164148 |
| [25] |
Nakanjako D, Kiragga AN, Musick BS, et al. Frequency and impact of suboptimal immune recovery on first-line antiretroviral therapy within the international epidemiologic databases to Evaluate AIDS in East Africa[J]. AIDS, 2016, 30(12): 1913-1922. DOI:10.1097/QAD.0000000000001085 |
| [26] |
Kroeze S, Ondoa P, Kityo CM, et al. Suboptimal immune recovery during antiretroviral therapy with sustained HIV suppression in sub-Saharan Africa[J]. AIDS, 2018, 32(8): 1043-1051. DOI:10.1097/QAD.0000000000001801 |
| [27] |
Okafor CN, Cook RL, Chen XG, et al. Trajectories of marijuana use among HIV-seropositive and HIV-seronegative MSM in the Multicenter AIDS Cohort Study (MACS), 1984-2013[J]. AIDS Behav, 2017, 21(4): 1091-1104. DOI:10.1007/s10461-016-1445-3 |
| [28] |
Kassaye SG, Wang CW, Ocampo JMF, et al. Viremia trajectories of HIV in HIV-positive women in the United States, 1994-2017[J]. JAMA Netw Open, 2019, 2(5): e193822. DOI:10.1001/jamanetworkopen.2019.3822 |
| [29] |
Franklin JM, Shrank WH, Pakes J, et al. Group-based trajectory models: a new approach to classifying and predicting long-term medication adherence[J]. Med Care, 2013, 51(9): 789-796. DOI:10.1097/MLR.0b013e3182984c1f |
| [30] |
Armstrong NM, Surkan PJ, Treisman GJ, et al. Association of long-term patterns of depressive symptoms and attention/executive function among older men with and without human immunodeficiency virus[J]. J Neurovirol, 2017, 23(4): 558-567. DOI:10.1007/s13365-017-0527-y |
| [31] |
Yuen T, Brouillette MJ, Fellows LK, et al. Personalized risk index for neurocognitive decline among people with Well-Controlled HIV Infection[J]. J Acquir Immune Defic Syndr, 2017, 76(1): 48-54. DOI:10.1097/QAI.0000000000001466 |
| [32] |
Mutoh Y, Nishijima T, Inaba Y, et al. Incomplete recovery of CD4 cell count, CD4 percentage, and CD4/CD8 ratio in patients with human immunodeficiency virus infection and suppressed viremia during long-term antiretroviral therapy[J]. Clin Infect Dis, 2018, 67(6): 927-933. DOI:10.1093/cid/ciy176 |
| [33] |
Ding Y, Duan S, Wu Z, et al. Timing of antiretroviral therapy initiation after diagnosis of recent human immunodeficiency virus infection and CD4+ T-cell recovery[J]. Clin Microbiol Infect, 2016, 22(3): 290.e5-290.e8. DOI:10.1016/j.cmi.2015.11.007 |
| [34] |
Mangal TD, Meireles MV, Pascom ARP, et al. Determinants of survival of people living with HIV/AIDS on antiretroviral therapy in Brazil 2006-2015[J]. BMC Infect Dis, 2019, 19(1): 206. DOI:10.1186/s12879-019-3844-3 |
| [35] |
Limmade Y, Fransisca L, Rodriguez-Fernandez R, et al. HIV treatment outcomes following antiretroviral therapy initiation and monitoring: A workplace program in Papua, Indonesia[J]. PLoS One, 2019, 14(2): e0212432. DOI:10.1371/journal.pone.0212432 |
| [36] |
Hughes RA, May MT, Tilling K, et al. Long terms trends in CD4+ cell counts, CD8+ cell counts, and the CD4+: CD8+ ratio[J]. AIDS, 2018, 32(10): 1361-1367. DOI:10.1097/QAD.0000000000001848 |
 2021, Vol. 42
2021, Vol. 42



