文章信息
- 国家免疫规划技术工作组流感疫苗工作组.
- National Immunization Advisory Committee(NIAC) Technical Working Group (TWG),Influenza Vaccination TWG
- 中国流感疫苗预防接种技术指南(2020-2021)
- Technical guidelines for seasonal influenza vaccination in China (2020-2021)
- 中华流行病学杂志, 2020, 41(10): 1555-1576
- Chinese Journal of Epidemiology, 2020, 41(10): 1555-1576
- http://dx.doi.org/10.3760/cma.j.cn112338-20200904-01126
-
文章历史
收稿日期: 2020-09-04
流感是流感病毒引起的对人类健康危害较重的呼吸道传染病,流感病毒抗原性易变,传播迅速,每年可引起季节性流行,在学校、托幼机构和养老院等人群聚集的场所可发生暴发疫情。全人群对流感普遍易感,孕妇、婴幼儿、老年人和慢性病患者等高危人群感染流感后危害更为严重。尤其是今年全球新型冠状病毒肺炎(新冠)疫情严重流行态势仍将持续,今冬明春可能会出现新冠疫情与流感等呼吸道传染病叠加流行的情况。而接种流感疫苗是预防流感的最有效手段,可以减少流感相关疾病带来的危害及对医疗资源的占用。中国CDC于2018和2019年均印发了当年度的《中国流感疫苗预防接种技术指南》。一年来,新的研究证据在国内外发表,新的疫苗产品在我国上市,为更好地指导我国流感预防控制和疫苗应用工作,国家免疫规划技术工作组流感疫苗工作组综合国内外最新研究进展,在2019年版指南的基础上进行了更新和修订,形成了《中国流感疫苗预防接种技术指南(2020-2021)》。
本指南更新的内容主要包括:第一,增加了新的研究证据,尤其是我国的研究结果,包括流感疾病负担、疫苗效果、疫苗安全性监测、疫苗预防接种成本效果等;第二,更新了一年来国家卫生健康委员会流感防控有关政策和措施;第三,更新了我国2020-2021年度国内批准上市及批签发的流感疫苗种类;第四,更新了本年度三价和四价流感疫苗组份;第五,更新了2020-2021年的流感疫苗接种建议。
一、病原学基础、临床特点和实验室诊断流感病毒属于正粘病毒科,是单股、负链、分节段的RNA病毒。根据病毒核蛋白和基质蛋白,分为甲、乙、丙、丁(或A、B、C、D)型。甲型流感病毒根据病毒表面的血凝素(hemagglutinin,HA)和神经氨酸酶(neuraminidase,NA)的蛋白结构和基因特性,可分为多种亚型。目前,发现的HA和NA分别有18个(H1~18)和11个(N1~11)亚型[1]。甲型流感病毒除感染人外,在动物中广泛存在,如禽类、猪、马、海豹以及鲸鱼和水貂等。乙型流感分为Victoria系和Yamagata系,可在人群中循环,最近数据显示海豹也可被感染。丙型流感病毒感染人、狗和猪,仅导致上呼吸道感染的散发病例[2]。丁型流感病毒,主要感染猪、牛等,尚未发现感染人[3-5]。目前,引起流感季节性流行的病毒是甲型中的H1N1、H3N2亚型及乙型病毒的Victoria和Yamagata系。
流感一般表现为急性起病、发热(部分病例可出现高热,达39~40 ℃),伴畏寒、寒战、头痛、肌肉、关节酸痛、极度乏力、食欲减退等全身症状,常有咽痛、咳嗽,可有鼻塞、流涕、胸骨后不适、颜面潮红、结膜轻度充血,也可有呕吐、腹泻等症状。轻症流感常与普通感冒表现相似,但其发热和全身症状更明显。重症病例可出现病毒性肺炎、继发细菌性肺炎、急性呼吸窘迫综合征、休克、弥漫性血管内凝血、心血管和神经系统等肺外表现及多种并发症[1, 6]。流感的症状是临床常规诊断和治疗的主要依据。但由于流感的症状、体征缺乏特异性,易与普通感冒和其他上呼吸道感染相混淆[7]。流感确诊有赖于实验室诊断,检测方法包括病毒核酸检测、病毒分离培养、抗原检测和血清学检测[8]。
二、流行病学 (一) 传染源、传播方式及潜伏期流感患者和隐性感染者是季节性流感的主要传染源,主要通过其呼吸道分泌物的飞沫传播,也可以通过口腔、鼻腔、眼睛等黏膜直接或间接接触传播[1, 9]。常见潜伏期为1~4 d(平均2 d),从潜伏期末到发病的急性期都有传染性。一般感染者在临床症状出现前24~48 h即可排出病毒,排毒量在感染后0.5~1.0 d显著增加,在发病后24 h内达到高峰[10]。成人和较大年龄儿童一般持续排毒3~8 d(平均5 d),患者感染不同毒株的排毒时间也会有差异。住院成人患者可在发病后持续1周或更长的时间排毒,排毒量也更大[2]。低龄儿童发病时的排毒量与成人相同,但排毒量下降更慢,排毒时间更长[11]。与成人相比,婴幼儿病例中,长期排毒很常见(1~3周)。老年人和HIV感染者等免疫功能低下或缺陷人群的病毒清除能力更差,排毒时间更长[10, 12]。
(二) 流感在我国的流行特点和季节性流感在温带地区表现为每年冬、春季的季节性流行和高发[13-15]。热带地区尤其在亚洲,流感的季节性呈高度多样化,既有半年或全年周期性流行,也有全年循环[14-17]。
2013年,一项针对我国不同区域流感季节性的研究显示[18],我国A型流感的年度周期性随纬度增加而增强,且呈多样化的空间模式和季节性特征:北纬33°以北的北方省份,呈冬季流行模式,每年1-2月份单一年度高峰;北纬27°以南的最南方省份,每年4-6月份单一年度高峰;两者之间的中纬度地区,每年1-2月份和6-8月份的双周期高峰;而B型流感在我国大部分地区呈单一冬季高发。2018年一项研究对我国2005-2016年度B型流感流行特征进行了系统分析[19],总体而言,我国乙型流感的流行强度低于甲型;但在部分地区和部分年份,乙型流感的流行强度高于甲型,且B/Yamagata系和B/Victoria系交替占优势,以冬春季流行为主,不同系的流行强度在各年间存在差异。
(三) 疾病负担1.健康负担:
(1)全人群:全人群对流感普遍易感。根据一项对全球32个流感疫苗接种随机对照队列中未接种疫苗人群的流感罹患率统计,有症状流感在成年人中的罹患率为4.4%(95%CI:3.0%~6.3%),>65岁人群为7.2%(95%CI:4.3%~12.0%);所有流感(包括无症状感染)在成年人中的罹患率为10.7%(95%CI:4.5%~23.2%)[20]。中国最新一项基于全国流感样病例(influenza like illness,ILI)和流感病原学监测数据的模型研究估计了流感相关门诊就诊疾病负担,结果显示[21]:在2006-2015年,中国平均每年流感相关ILI超额门诊就诊负担为2.5人次/千人,最高为2009年流感大流行时的7.8人次/千人,最低为2006年的0.7人次/千人;其中<15岁儿童ILI门诊就诊负担最重,为4.5人次/千人,显著高于15~59岁成人(2.3人次/千人)和≥60岁老年人(1.1人次/千人)。北京市基于ILI和住院严重急性呼吸道感染病例(severe acute respiratory infection,SARI)监测的研究提示[22]:2017-2018流行季节,北京市流感感染人数约为227.1万人,总感染率为10.5%,有症状发病率为6.9%;其中15~24岁组感染率和发病率分别为13.4%和8.8%,25~59岁组分别为6.4%和4.2%,≥60岁组为5.6%和3.7%。
流感在全球每年可导致29万~65万呼吸道疾病相关死亡[23]。中国最新一项基于全国流感监测和死因监测数据的模型研究,估计了流感相关超额呼吸系统疾病死亡,结果显示[24]:2010-2011至2014-2015流行季节,全国平均每年有8.8万(95%CI:8.4万~9.2万)例流感相关呼吸系统疾病超额死亡,占呼吸系统疾病死亡的8.2%(95%CI:7.8%~9.6%);全年龄组的超额死亡率平均为6.5/10万人年(95%CI:6.3/10万人年~6.8/10万人年),年龄标化率为5.9/10万人年(95%CI:5.5/10万人年~6.3/10万人年);≥60岁老年人的流感相关超额死数占全人群的80%,其超额死亡率显著高于60岁以下人群(38.5/10万人年vs. 1.5/10万人年)。另一项对中国流感相关死亡负担研究的系统综述提示[25]:老年人流感相关呼吸及循环系统疾病超额死亡率为30.8/10万~170.2/10万;非老年组为0.32/10万~2.6/10万;不同流行季节、不同病毒亚型导致的死亡也存在差异。
(2)慢性基础性疾病患者:与同龄健康成年人相比,慢性基础性疾病患者感染流感病毒后,更易出现严重疾病或死亡,其流感相关住院率和超额死亡率更高。近期一项研究基于全球流感住院监测网络分析发现,2013-2014北半球流感流行季,40%的流感相关住院病例患有慢性基础性疾病;对于大多慢性基础性疾病而言,A(H3N2)、A(H1N1)pdm09亚型和B/Yamagata系所致重症流感的风险无显著差异[26]。2017-2018年度,中国浙江省开展的一项多中心、回顾性观察性研究发现,>14岁甲型流感住院患者中,患有慢性肺部疾病(chronic lung diseases,CLD)(OR=2.581,95%CI:1.447~4.603)和糖尿病(OR=2.042,95%CI:1.135~3.673)的患者出现重症肺炎的风险更高[27]。澳大利亚一项对患有CLD儿童开展的10年队列研究提示[28],CLD患儿和非CLD儿童流感相关住院率分别为3.9(95%CI:2.6~5.2)/千人年和0.7(95%CI:0.5~0.9)/千人年。与健康人群相比,慢性基础性疾病患者流感相关死亡率明显增高。一项综述性研究发现,流感流行季节慢性阻塞性肺疾病(chronic obstructive pulmonary diseases,COPD)患者甲型流感相关超额病死率超过30%,明显高于健康人群(≤0.1%)[29]。中国台湾地区一项研究回顾了2016-2018年某医疗机构的实验室确诊流感重症患者,发现患有肝硬化(校正后HR=3.94,95%CI:1.07~14.45)或风湿性疾病(校正后HR=7.45,95%CI:2.34~23.69)是流感相关死亡的危险因素[30]。
(3)孕妇:流感对孕妇的健康危害比较严重。由于妊娠后机体免疫和生理上的变化[31-32],孕妇感染流感病毒后的住院、严重疾病和死亡风险较未孕育龄女性更高[33-34]。日本一项研究表明,2010-2014年的4个流感流行季中,孕妇比未妊娠的育龄妇女更容易发生呼吸系统疾病相关的住院(RR=4.3,95%CI:1.96~9.41)[35]。美国流感住院监测网络2010-2018年数据的分析也发现,尽管育龄女性平均每年仅9%妊娠,但育龄女性流感相关住院中24%~34%为孕妇[36]。2019年发表的一项队列和病例对照研究的Meta分析,对33项研究中的36 498例实验室确诊流感的育龄女性门诊或住院病例个案的分析发现,孕妇住院风险是非孕妇的6.80倍(95%CI:6.02~7.68)[37]。美国一项1998-2005年孕妇流感死亡负担研究显示,研究期间孕妇流感相关死亡率平均为3.1/100万活产[38],孕晚期孕妇流感相关死亡率最高。西班牙一项回顾性队列研究纳入了约20万孕妇,结果表明孕晚期因流感住院风险显著增加(RR=1.9,95%CI:1.0~3.4)[39]。我国一项关于2009年大流行期间A(H1N1)pdm09住院病例的研究发现,孕妇仅占育龄妇女人口数的3%,但A(H1N1)pdm09死亡病例中20%为孕妇,其中仅7%患有慢性基础性疾病;与未妊娠的健康育龄妇女相比,孕妇出现严重疾病的风险增加3.3倍(95%CI:2.7~4.0),孕中期(OR=6.1)和孕晚期(OR=7.6)出现严重疾病的风险进一步增加[40]。研究还显示,孕妇患流感可对胎儿和新生儿产生影响,出现死产、婴儿死亡、早产和出生低体重等[41-43]。
(4)儿童:每年流感流行季节,儿童流感罹患率约为20%~30%,在某些高流行季节[44],儿童流感年感染率高达50%左右[45-46]。一项关于流感罹患率(包括有症状和无症状的感染)的综述研究提示[20],<18岁儿童流感罹患率约为22.5%(95%CI:9.0%~46.0%),而成人流感罹患率约为10.7%(95%CI:4.5%~23.2%)。北京市2017-2018流行季节流感感染率和发病率研究提示,0~4岁组和5~14岁组发病率最高,分别为33.0%(95%CI:26.4%~43.1%)和21.7%(95%CI:17.4%~28.4%)[22]。苏州市2011-2017流行季节<5岁儿童确诊流感导致的ILI就诊率为6.4/100人年,其中2011-2012流行季节最高(20.5/100人年),2012-2013流行季节最低(2.4/100人年)[47]。
<5岁儿童感染流感后出现重症的风险较高。一项对全球<5岁儿童开展的流感相关呼吸系统感染疾病负担系统综述模型研究提示[48],2018年,全球<5岁儿童约有10 950万[不确定区间(uncertainty range,UR):6 310万~19 060万]感染流感病毒,1 010万(UR:680万~1 510万)流感相关急性下呼吸道感染(acute lower respiratory infection,ALRI),87万(UR:54.3万~141.5万)流感相关ALRI住院病例,1.53万(UR:0.58万~4.38万)流感相关ALRI住院病例死亡,3.48万(UR:1.32万~9.72万)流感相关ALRI病例死亡。湖北省荆州市一项基于人群的研究表明,流感导致的SARI住院患者中69%为<5岁儿童,该年龄组流感相关SARI住院率达2 021/10万人年~2 349/10万人年,其中6~11月龄婴儿住院率最高(3 603/10万人年~3 805/10万人年)[49]。苏州市开展的2011-2016流行季节<5岁儿童流感确诊住院率研究提示[50],研究期间<5岁儿童流感确诊SARI住院率范围是4(95%CI:2~5)人次/千人(2012-2013流行季节)至16(95%CI:14~19)人次/千人(2011-2012流行季)。儿童感染流感可导致死亡,患基础性疾病的儿童的死亡风险显著高于健康儿童,但也有将近半数的死亡病例发生在健康儿童[44]。一项对全球流感相关死亡的模型研究估计,纳入的92个国家每年约有9 243~105 690名<5岁儿童死于流感相关呼吸系统疾病[23]。
(5)学生:学校作为封闭的人群密集场所,容易造成流感病毒的传播[51-52]。我国每年报告的流感暴发疫情中,>90%发生在学校和托幼机构。与其他人群相比,学龄儿童的流感感染率最高[53]。经估算,北京市2015-2016流行季节5~14岁儿童流感感染率为18.7%(95%CI:12.9%~24.5%),明显高于青壮年和老年人群[54]。学龄儿童在学校、家庭和社区的流感传播中发挥重要的作用,流感流行可引起大量学龄儿童缺课和父母缺勤[55-56]。
(6)医务人员:医务人员在日常诊疗活动中接触流感患者的机会较多,因而感染流感病毒的风险高于普通人群。一项对1957-2009年全球29项研究的Meta分析显示,未接种流感疫苗的医务人员每流行季节实验室确诊的流感发病率平均为18.7%(95%CI:15.8%~22.1%),是健康成年人的3.4倍(95%CI:1.2~5.7)[57]。2016年发表的一项系统综述显示,在甲型H1N1流感大流行期间,与普通人群相比,医务人员感染风险较高(OR=2.08,95%CI:1.73~2.51),而临床医生的风险更高(OR=6.03,95%CI:2.11~17.8)[58]。2019年WHO进行的一项快速证据评估的结果也提示,与普通人群相比,医务人员感染流感病毒的风险更高[59]。医务人员感染流感病毒可增加院内感染的风险。研究显示,在感染流感病毒的医务人员中,35%为无症状感染[60],>75%出现流感样症状后仍继续工作[61-62]。虽然难以量化传播风险,感染流感病毒的医务人员即便是无症状感染仍有可能在医护环境中传播流感病毒给高危人群,从而导致重症和死亡的发生[63]。
(7)老年人:流感感染是老年人的重要死因。一项关于全球流感超额死亡率的模型研究表明,<65岁人群中因流感相关呼吸道超额死亡率为0.1/10万~6.4/10万,65~74岁组中超额死亡率为2.9/10万~44.0/10万,>75岁组为17.9/10万~223.5/10万[23]。2017-2018流行季节(以乙型流感为主)欧洲地区一项超额死亡研究提示,≥65岁老年人流感相关全死因超额死亡率为154.1(95%CI:149.4~158.9)/10万,与A(H3N2)亚型为优势毒株的2016-2017流行季节类似,提示乙型流感疾病负担不容小觑[64]。
我国全国范围及广州市、中国香港地区等的流感超额死亡研究显示,≥65岁老年人流感相关的呼吸和循环系统疾病、全死因超额死亡率分别为64/10万~147/10万、75/10万~186/10万[65-67],与新加坡[66, 68]、葡萄牙[69]、美国[70]等发达国家接近。与其他年龄组相比,流感相关死亡风险在老年人中最高。≥65岁老年人流感相关超额死亡率远高于0~64岁组,80%~95%的流感相关超额死亡发生在≥65岁老年人[24, 65-67, 71]。
流感也可导致老年人出现相当高的住院负担。2010-2012年湖北省荆州市基于人群的研究发现,≥65岁老年人中确诊流感导致的SARI病例住院率为89/10万~141/10万[72]。此外,养老院、疗养院等老年人集体居住的机构容易出现流感暴发疫情。
2.经济负担和健康效用:我国现有流感相关经济负担研究大多集中在广东省[73-75]、山东省[76]、江苏省[77-79]、上海市[79-83]、浙江省[84]、天津市[85-87]和北京市[88]等地区。流感门诊病例直接医疗费用在195~804元之间,直接非医疗费用在46~212元之间,间接费用在139~963元之间,总经济负担在464~1 320元之间[88-89];流感住院病例直接医疗费用在2 625~20 712元之间,直接非医疗费用为1 200~1 809元之间,间接费用在204~2 408元之间,总经济负担在9 832~25 768元之间[88-89],住院病例经济负担显著高于门诊病例。各人群亚组间经济负担差异具有显著性,儿童和18~60岁人群因具有较高的误工成本成为经济负担较重的亚人群[90];高危人群的经济负担普遍高于低危人群[83, 90-91],确诊流感病例的经济负担显著高于非流感的ILI[80]。2013年我国一项研究显示[91],患有慢性基础性疾病的流感患者其门诊和住院费均高于无基础性疾病的流感患者(门诊:186美元vs. 146美元;住院:1 800美元vs. 1 189美元),对于生存质量的研究也显示,基础性疾病患者的健康相关生存质量显著低于无基础性疾病者[92]。
另外,流感感染还可明显影响患者的生命质量,超过60%的流感门诊和住院病例报告具有疼痛、不适和焦虑、沮丧。患流感期间,门诊和住院病例的健康效用值(health utility)分别为0.61和0.59,损失的质量调整生命天(quality adjusted life days,QALD)为1.62和3.51 d[92]。流感同样会造成人群生产力的下降,如工作缺勤。中国香港地区一项针对医务工作者的回顾性队列研究显示,2005年未接种流感疫苗的医务人员平均每人因ILI而缺勤1.75 d[93]。苏州市一项研究显示,儿童流感病例的缺课天数和家长缺勤天数分别为1.3和1.4 d[94]。流感患者或患者家属陪护的误工天数在1.3~8.0 d之间[80, 86]。
(四) 流感的预防治疗措施每年接种流感疫苗是预防流感最有效的手段,可以显著降低接种者罹患流感和发生严重并发症的风险。奥司他韦、扎那米韦、帕拉米韦等神经氨酸酶抑制剂是甲型和乙型流感的有效治疗药物,早期尤其是发病48 h之内应用抗流感病毒药物能显著降低流感重症和死亡的发生率。抗病毒药物应在医生的指导下使用。药物预防不能代替疫苗接种,只能作为没有接种疫苗或接种疫苗后尚未获得免疫能力的重症流感高危人群的紧急临时预防措施,可使用奥司他韦、扎那米韦等。
采取日常防护措施也可以有效减少流感的感染和传播,包括:保持良好的呼吸道卫生习惯,咳嗽或打喷嚏时,用纸巾、毛巾等遮住口鼻;勤洗手,尽量避免触摸眼睛、鼻或口;均衡饮食,适量运动,充足休息等。避免近距离接触流感样症状患者,流感流行季节,尽量避免去人群聚集场所;出现流感样症状后,患者应居家隔离观察,不带病上班、上课,接触家庭成员时戴口罩,减少疾病传播;流感样症状患者去医院就诊时,患者及陪护人员要戴口罩,避免交叉感染。
三、流感疫苗 (一) 国内外上市的流感疫苗全球已上市的流感疫苗分为流感灭活疫苗(inactivated influenza vaccine,IIV)、流感减毒活疫苗(live attenuated influenza vaccine,LAIV)和重组流感疫苗(recombinant influenza vaccines,RIV)。按照疫苗所含组份,流感疫苗包括三价和四价,三价疫苗组份含有A(H3N2)亚型、A(H1N1)亚型和乙型毒株的1个系,四价疫苗组份含A(H3N2)亚型、A(H1N1)亚型和乙型Victoria系、Yamagata系。根据生产工艺,又可分为基于鸡胚、基于细胞培养和重组流感疫苗。国外还上市了针对特定人群的高抗原含量灭活流感疫苗、佐剂疫苗以及皮内接种疫苗等。
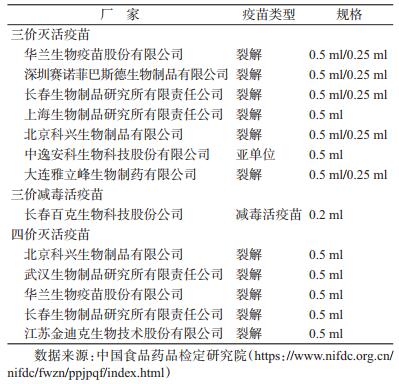
我国现已批准上市的流感疫苗有三价灭活流感疫苗(IIV3)、四价灭活流感疫苗(IIV4)和三价减毒活疫苗(LAIV3),IIV3包括裂解疫苗和亚单位疫苗,IIV4为裂解疫苗,LAIV3为减毒疫苗。根据国家药监局网站和疫苗批签发信息,2020-2021流行季节有10家厂家供应流感疫苗。本季节供应流感疫苗的厂家及其产品信息见表 1。
免疫原性是指抗原能够刺激机体形成特异抗体或致敏淋巴细胞的能力,评价指标主要为病毒株特异性HI抗体水平和血清抗体阳转率,评价结果会受接种者年龄、免疫功能和接种前抗体水平的影响。疫苗的效力通常是指其在上市前随机对照试验(RCT)中理想条件下的有效性;疫苗的效果则指其在人群中实际应用的有效性。评价流感疫苗效力和效果的结局指标主要包括血清抗体水平和阳转率、实验室确诊流感、SARI或ILI就诊、流感和肺炎相关住院或死亡等。
目前,我国供应的流感IIV,其接种后A(H3N2)、A(H1N1)亚型和B/Yamagata、B/Victoria系的HI抗体阳转率、HI抗体GMT平均增长倍数和血清抗体保护率均达到有关标准,具有较好的免疫原性[95-97]。此外,我国还批准上市了1种鼻喷LAIV3。根据研究发表数据,LAIV在婴幼儿、学龄儿童的免疫反应较成年人好[98-100],具有良好免疫原性[101-102]。
1.全人群:灭活流感疫苗在健康成人中免疫原性良好。在健康成人中,根据RCT的系统综述估计,接种灭活流感疫苗可预防59%(95%CI:51%~66%)的实验室确诊流感[103-104];当疫苗株和循环株匹配时,接种灭活流感疫苗可减少42%(95%CI:9%~63%)的ILI就诊[104]。一项纳入了1998-2008年国内文献中的2项RCT和11项队列研究的系统综述[105],显示流感疫苗对我国18~59岁ILI的预防效果为47%(95%CI:25%~63%)。在全年龄组人群中,检测阴性病例对照研究的系统综述(包含2004-2015年的56项研究)发现流感疫苗对不同型别和亚型的流感的预防效果有明显差异,其中乙型为54%(95%CI:46%~61%),A(H1N1)pdm09亚型(2009年及以后)为61%(95%CI:57%~65%),H1N1亚型(2009年之前)为67%(95%CI:29%~85%),H3N2亚型为33%(95%CI:26%~39%)[106]。
国外RCT试验的Meta分析显示,在≥18岁成人中,IIV4与IIV3在相同疫苗株的血清保护率和抗体阳转率方面无显著性差异,IIV4中增加的乙型流感系的抗体保护率和抗体阳转率明显高于IIV3[107-108]。2018-2019年度我国开展的一项IIV4接种后免疫原性研究也提示,IIV3或IIV4接种1个月后血清抗体滴度均达到较高水平,接种IIV3或IIV4对甲型H1N1和A(H3N2)亚型流感的血清阳转率差异无统计学意义,但接种IIV4后对B(Victoria)系流感的血清阳转率高于IIV3[109]。
2.孕妇:国外多项研究提示妊娠期接种流感疫苗,具有良好免疫原性[110-112]。妊娠期接种流感疫苗,既可保护孕妇,降低孕期患流感、孕期发热、子痫前期、胎盘早破的风险,也可通过胎传抗体保护<6月龄无法接种流感疫苗的新生儿免于罹患流感[113-116]。在4项RCT和3项观察性研究的Meta分析中,孕期接种流感疫苗对<6月龄婴儿实验室确诊的流感的保护率为48%(95%CI:33%~59%);在4项观察性研究的Meta分析中,孕期接种流感疫苗对<6月龄婴儿实验室确诊的流感相关住院的保护率为72%(95%CI:39%~87%)[117]。2019年一项Meta分析指出[118],相较于孕早期接种流感疫苗,孕晚期接种流感疫苗的孕妇及其新生儿体内HI滴度上升倍数更高,且孕晚期接种流感疫苗更有利于抗体传递给胎儿。英国研究者对孕妇接种流感疫苗的时间与婴儿出生时抗体水平的观察性研究也发现,与孕早期相比,孕妇在孕中期或孕晚期接种流感疫苗其婴儿体内的抗体滴度会更高[119]。
3.儿童:
(1)IIV:>6月龄儿童按推荐的免疫程序接种IIV3后对流感病毒感染有保护作用。2012年一项IIV3效力和效果的Meta分析显示,6~23月龄儿童的疫苗效果为40%(95%CI:6%~61%),24~59月龄儿童为60%(95%CI:30%~78%)[103]。国内研究显示,2011-2012年度IIV3对36~59月龄及6~35月龄的保护效果分别为58.2%和49.5%[120]。
国外研究提示,<9岁儿童首次接种IIV3时,接种2剂次比1剂次能提供更好的保护作用,如5~8岁儿童接种2剂IIV3后,针对A(H1N1)、A(H3N2)和乙型流感病毒产生的抗体滴度显著高于接种1剂次[121]。日本对2013-2018年度6月龄~12岁儿童的研究提示:无论接种1剂次还是2剂次流感IIV,均对儿童感染流感具有保护效果,但接种2剂次疫苗在部分年度对乙型流感的保护效果更好[122]。中国香港地区对2011-2019年度因急性呼吸道感染住院的6月龄~9岁儿童开展了接种2剂次和1剂次流感疫苗效果研究[123],发现首次接种流感疫苗完成2剂次程序和仅接种1剂次对流感确诊住院病例的保护效果分别为73%(95%CI:69%~77%)和31%(95%CI:8%~48%)。因此,低龄儿童首次接种流感疫苗应接种2剂,才能获得最大程度的保护。
研究提示,IIV4对乙型流感的免疫原性优于IIV3。一项2013-2014流行季节在部分国家的3~8岁儿童开展的随机、双盲、接种IIV3为对照的临床试验提示,接种IIV4后对IIV3未含的乙型流感产生的GMT高于IIV3诱导产生,即IIV4具有更好的免疫原性[124]。
中国香港地区2017-2018流行季节一项6月龄~17岁儿童流感疫苗效果研究[125],共纳入1 078名儿童,研究对象接种的大多为IIV4,结果显示流感疫苗对确诊流感住院总的保护效果为65.6%(95%CI:42.7%~79.3%),对甲型和乙型流感的保护效果分别为66.0%(95%CI:3.4%~88.0%)和65.3%(95%CI:39.5%~80.1%)。北京市对2013-2016流行季节流感疫苗效果模型研究发现,对于5~14岁儿童,3个流行季节接种流感疫苗分别可以减少约104 000(95%CI:101 000~106 000)例、23 000(95%CI:22 000~23 000)例和21 000(95%CI:21 000~22 000)例流感相关门急诊病例就诊[126]。2016-2017流行季节北京市流感疫苗对减少流感相关门急诊就诊效果为25%(95%CI:0%~43%),对A(H1N1)pdm09为中等保护效果,而对A(H3N2)为低保护效果[127]。
儿童接种流感疫苗还能对其他人群起到间接保护作用。2001-2002年度开展的一项研究评估了大规模接种流感疫苗对预防儿童罹患流感的直接保护作用及其对老年人的间接保护作用[128],结果发现研究地区57%的幼儿园儿童和72%的小学生接种流感疫苗后,对幼儿园儿童和小学生预防流感的保护效果分别为60.9%和68.8%,同时还可以减少儿童接种疫苗的地区老年人3.4倍的ILI和1.7~2.6倍的流感相关并发症(如哮喘、肺炎、心血管疾病、糖尿病等)。
另外,接种流感疫苗还可以减少抗生素的使用。美国南加州开展的一项研究提示[129],6月龄~17岁儿童使用流感疫苗可以降低门诊处方抗生素的使用率,流感疫苗接种率每提高1%,门诊抗生素处方使用就下降3人次/每千人月。
(2)LAIV3:LAIV中含有鼻腔接种后可在鼻咽部复制的减毒流感病毒,其所含疫苗株具有以下3个特点:毒力衰减(限制其反应原性和致病性)、温度敏感性(限制其在下呼吸道复制)和冷适应性(允许其在鼻咽部复制)[130]。经鼻腔注射LAIV后可诱导血清和鼻黏膜均产生抗体,同时也可诱导细胞介导的免疫反应[131]。
在1996-1997和1997-1998年对1 602名15~71月龄的健康儿童进行的一项大型随机、双盲、安慰剂对照的试验中[132-133],疫苗株和循环株完全匹配的1996-1997流行季,接受2剂次对实验室确诊流感的保护效力为94%(95%CI:88%~97%),接受1剂次的保护效果为89%(95%CI:65%~96%);而疫苗株中A(H3N2)亚型与循环株不匹配的1997-1998流行季,接种1剂次的保护效力为86%(95%CI:75%~92%);2个季节总的效力为92%(95%CI:88%~94%)。另一项随机、安慰剂对照的试验比较了2001和2002年南非、巴西和阿根廷3 200名6~35月龄儿童接种1剂次和2剂次LAIV3的效力[134],第一年度,接种1剂和2剂的效力分别为57.7%(95%CI:44.7%~67.9%)和73.5%(95%CI:63.6%~81.0%);第二年度,接种1剂的效力为73.6%(95%CI:33.3%~91.2%),总的效力为65.2%(95%CI:31.2%~88.8%)。其他随机、安慰剂对照、2个流行季的试验研究同样也提示LAIV3对小年龄儿童有类似的保护效力[135-136]。一项2016-2017流行季在我国东部地区3~17岁儿童中开展的随机、双盲、对照试验评价了LAIV3的效力[137],结果发现疫苗对所有亚型流感的效力为62.5%(95%CI:27.6%~80.6%),对A(H3N2)亚型流感的效力63.3%(95%CI:27.5%~81.5%)。
除对实验室确诊流感有保护效果外,一项RCT试验提示[132],LAIV3可减少21%(95%CI:11%~30%)的发热性疾病,也可减少30%(95%CI:18%~45%)的中耳炎。对6项安慰剂对照试验研究的Meta分析提示,LAIV3对6~83月龄儿童实验室确诊流感合并急性中耳炎的保护效果为85%(95%CI:78%~90%)[138]。
4.学生:开展基于学校的流感疫苗接种可有效减少学龄儿童流感感染的发生。2014-2015流行季,中国北京市基于中小学校流感集中发热疫情的研究表明,在确诊流感的学生中,接种流感疫苗的学生与未接种的学生相比,出现>38 ℃发热的风险显著减低(OR=0.42,95%CI:0.19~0.93)[139]。疫苗株与流行毒株匹配的季节,北京市流感疫苗大规模集中接种可使流感集中发热疫情的发生风险大幅降低(OR=0.111,95%CI:0.075~0.165)[140]。2016-2017流行季,北京市中小学生接种流感疫苗的总体保护效果为69%(95%CI:51%~81%),其中甲型H1N1流感和A(H3N2)亚型流感的保护效果分别为60%(95%CI:15%~86%)和73%(95%CI:52%~84%)[141]。2016-2017流行季韩国的一项研究发现,韩国小学生接种流感疫苗后2周、3周以及4周以上预防流感的效果分别为17.6%(95%CI:4.6%~28.9%),22.5%(95%CI:10.3%~33.0%)和28.7%(95%CI:17.5%~38.3%)[142]。2018-2019流行季,中国香港地区的一项研究发现,接种流感疫苗的小学生与未接种的小学生相比,ILI发生率显著降低(7.7% vs. 14.1%),保护效果达45.3%[143]。同时,学生接种流感疫苗还可减少由于罹患流感导致的缺勤缺课。美国2005-2008年度开展的干预研究提示[144-145],流感流行季,小学生、中学生和高中生接种流感疫苗可以减少由于罹患流感导致缺勤的人数。
5.老年人:2018年对8个RCT的Meta分析发现,老年人接种流感疫苗预防流感的保护效力为58%(95%CI:34%~73%)[146]。2015-2020年4个流行季,美国≥65岁老年人接种流感疫苗预防因流感导致的急性呼吸道疾病就诊的效果分别为42%(95%CI:6%~64%)、46%(95%CI:4%~70%)、18%(95%CI:-25%~47%)和12%(95%CI:-31%~40%))[147-150]。2017年一项对检测阴性病例对照研究设计的社区老年人流感疫苗效果的Meta分析发现,无论流感疫苗与流行株是否匹配,接种流感疫苗均有效,疫苗株与循环株匹配时保护效果为44.4%(95%CI:22.6%~60.0%),不匹配时保护效果为20.0%(95%CI:3.5%~33.7%)[151]。我国一项对1998-2008年流感疫苗效果研究的Meta分析发现,针对老年人的队列研究,流感疫苗对≥60岁老年人的流感样疾病的预防效果为53%(95%CI:20%~72%)[105]。
接种流感疫苗还可降低老年人流感相关并发症发生率,减少流感相关住院及死亡。2013年1篇对95项研究的Meta分析发现,在流感季节,老年人接种流感疫苗能预防28%(95%CI:26%~30%)的流感相关致命性或非致命性并发症、39%(95%CI:35%~43%)的流感样症状、49%(95%CI:33%~62%)的确诊流感[152]。2017-2018流行季,美国>65岁老年人接种流感疫苗减少了715 073人发病,400 441人就诊,65 007人住院,6 796人死亡[153];2018-2019流行季,则减少了300 879人发病,168 492人就诊,28 695人住院,2 625人死亡[154]。
多项研究表明,老年人接种标准剂量的流感疫苗所产生的抗体水平、保护效力和保护效果与年轻人比较相对较低[103, 155-158]。为提高流感疫苗在老年人中的免疫应答、保护效力和保护效果,2009年美国FDA批准了高剂量IIV3,将每种抗原组分的含量由标准的15 μg提高到60 μg[159]。与接种标准剂量流感疫苗相比,老年人接种高剂量流感疫苗可产生较高水平的流感抗体[160-164],对于预防流感确诊感染具有相对较好保护效力[163-164],同时对于预防流感确诊感染、流感相关就诊、住院和死亡具有相对较好的保护效果[165-169]。
6.慢性基础性疾病患者:我国开展的队列研究表明,接种IIV3可以减少COPD和慢性支气管炎的急性感染和住院[170-171]。中国成都市一项队列研究发现,与未接种疫苗的对照组相比,IIV3接种3、6个月后COPD急性加重的住院天数分别减少3.3、7.1 d[170]。流感疫苗对儿童和成人哮喘患者有较好免疫原性[172];哮喘患者接种流感疫苗能够有效减少流感感染和哮喘发作[173]。流感疫苗在心血管疾病患者中免疫原性良好,能够保护心血管病患者减少流感感染。冠心病患者接种流感疫苗后,可以减少急性冠脉综合征(acute coronary syndromes,ACS)患者的心血管不良事件发生率,降低其住院风险和与心脏病相关的死亡率[174],减少ACS患者与流感有关的直接和间接医疗成本,符合成本效益[175-176]。流感疫苗还可降低心衰患者的死亡风险,丹麦的一项队列研究提示[177],在随访期间(中位随访时间为3.7年),校正相关混杂因素后,接种≥1剂次流感疫苗可使心力衰竭(heart failure,HF)患者的全因死亡风险降低18%(HR=0.82,95%CI:0.81~0.84),心血管死亡风险也降低18%(HR=0.82,95%CI:0.81~0.84)。18~64岁的糖尿病患者接种流感疫苗对住院的保护效果是58%;老年人糖尿病患者接种流感疫苗,对住院的保护效果为23%,对全死因死亡的保护效果为38%~56%[178]。另外,研究提示接种流感疫苗可以减少免疫功能受损的流感住院儿童并发症的发生风险,缩短住院时间[179]。
7.医务人员:医护人员接种流感疫苗不仅可保护自身健康,有效减少医务人员将病毒传给流感高危人群的机会,并维持流感流行季节医疗服务的正常运转[180]。2项系统综述结果显示:与流感病毒匹配良好的季节性流感疫苗,医务人员的疫苗效力高达90%[181-182]。一项收录了1980-2018年研究结果的系统综述显示,疫苗接种组实验室确诊的流感发病率明显低于未接种组(合并RR=0.40,95%CI:0.23~0.69),并且由ILI导致的缺勤率降低(合并RR=0.62,95%CI:0.45~0.85)[183]。2018-2019年沙特一项研究结果显示,接种流感疫苗的医务人员预防各亚型流感的效果为42%,预防A(H3N2)和甲型H1N1流感的效果分别为76%和55%,对乙型未显示保护作用[184]。研究提示,接种流感疫苗不仅可减少医务人员的缺勤率和实验室确认的流感发病率,还可降低患者死亡率[185]。国内研究结果也证实[186-187],医务人员接种流感疫苗可以减少缺勤、ILI发病和呼吸系统疾病的发病与就诊,降低心脑血管疾病和糖尿病的就诊率。
(三) 免疫持久性人体对感染流感病毒或接种流感疫苗后获得的免疫力会随时间衰减,衰减程度与人的年龄和身体状况、疫苗抗原等因素有关,临床试验的证据提示,接种灭活流感疫苗对抗原类似毒株的保护作用可维持6~8个月[188]。接种1年后血清抗体水平显著降低,但部分毒株的保护作用持续时间可更长。为匹配不断变异的流感病毒,WHO在多数季节推荐的流感疫苗组份会更新一个或多个毒株,疫苗毒株与前一季节完全相同的情况也存在。为保证接种人群得到最大程度地保护,即使流感疫苗组份与前一季节完全相同,鉴于多数接种者抗体滴度已显著下降[189-191],因此不管前一季节是否接种流感疫苗,仍建议在当年流感季节来临前接种。
流感疫苗需要每年接种。疫苗效果研究证实了重复接种的必要性。据中国香港地区对2012-2017年连续5个流行季节儿童住院病例中流感疫苗效果的分析[192],流感疫苗接种后每个月效果约下降2%~5%,接种后0.5~2个月时疫苗效果估计为79%(95%CI:64%~88%),至接种后7~9个月时疫苗效果仅余45%(95%CI:22%~61%)。此外,比较了连续2个季节接种、仅本季节接种、仅上一季节接种和2个季节均未接种的流感疫苗效果的系统综述发现[193],结论支持无论上一季节接种状态如何,本季节都应重新接种流感疫苗。
(四) 安全性疑似预防接种异常反应(adverse event following immunization,AEFI)是指在预防接种后发生的怀疑与预防接种有关的不良反应或医学事件。我国于2010年发布《全国疑似预防接种异常反应监测方案》,要求责任报告单位和报告人发现属于报告范围的AEFI(包括接到受种者或其监护人的报告)后应当及时向受种者所在地的县级卫生行政部门、药品监督管理部门报告,相关信息将通过AEFI信息管理系统进行网络报告,AEFI监测属于被动监测。
1. IIV:通过肌肉注射接种IIV是安全的,但也可能会出现不良反应。流感疫苗常见的副作用主要表现为局部反应(接种部位红晕、肿胀、硬结、疼痛、烧灼感等)和全身反应(发热、头痛、头晕、嗜睡、乏力、肌痛、周身不适、恶心、呕吐、腹痛、腹泻等)。通常是轻微的,并在几天内自行消失,极少出现重度反应。研究表明IIV3和IIV4在安全性上没有差别[194-204],国产和进口流感疫苗相比安全性也无显著性差异[205-207]。
2015-2018年AEFI信息管理系统的监测数据分析显示,所有IIV不良反应中报告最多的为发热(腋温≥37.1 ℃),其中高热(腋温≥38.6 ℃)发生率为4.274/10万剂,儿童型疫苗略高于成人型(4.465/10万剂vs. 4.165/10万剂);非严重异常反应中,以过敏性皮疹(442例,0.531/10万剂)和血管性水肿(70例,0.084/10万剂)报告最多;严重异常反应的报告发生率低,为0.143/10万剂,排名前两位为热性惊厥(27例,0.032/10万剂)和过敏性紫癜(21例,0.025/10万剂)[208]。
2. LAIV:
(1)疫苗株病毒排毒和人际传播:无论是儿童还是成年人,在接种LAIV后都会出现部分受种者排出疫苗株病毒的情况,排毒量和排毒时长均要少于自然感染流行毒株。一项对3个年龄段(5~8岁,9~17岁和18~49岁)的344名LAIV3的受种者鼻拭子病毒培养的研究提示:30%的受种者可检测到病毒,排毒的持续时间和排出量与年龄成反比,排毒多在接种后第2天发生(范围:1~11 d)[209]。一项针对200名6~59月龄儿童的研究提示,接受单剂次LAIV3,157名(79%)的受种者可培养出≥1种疫苗株病毒(低滴度排毒),并且在小年龄组更常见(6~23月龄的89% vs. 24~59月龄的69%);接种后第2天排毒的发生率最高,平均排毒持续时间为2.8 d(小年龄组和高年龄组分别为3.0和2.7 d);疫苗接种11 d后仍出现排毒的情况不常见,偶尔发生在6~23月龄儿童(未获得LAIV接种许可的年龄组)[210]。
偶有报道LAIV疫苗株病毒发生从受种者向未接种者的传播,但尚未发现被疫苗株病毒感染的未接种者发生严重疾病的报告。一项对197名9~36月龄的托幼中心儿童进行的研究评估了LAIV3疫苗毒株发生传播的可能性(98名受种儿童,99名未受种儿童),结果显示80%的受种者出现了排毒(平均持续时间:7.6 d);未接种者中1名儿童感染了乙型LAIV疫苗株病毒,出现了轻度上呼吸道感染症状;未受种儿童在接触1个LAIV受种儿童后出现疫苗株病毒传播的概率估计为0.58%(95%CI:0%~1.7%),提示发生概率较低[211]。
(2)不良反应:儿童接种LAIV3后报告的症状和体征包括流鼻涕或鼻塞、头痛、发热、呕吐、腹痛和肌痛等[212-216],多与第一次接种LAIV有关,并且为自限性。一项针对9 689名1~17岁儿童的安慰剂对照试验中,评估发现在疫苗接种后42 d内,LAIV3导致哮喘、上呼吸道感染、肌肉骨骼疼痛和中耳炎伴积液发生的风险增加,但并不常见;LAIV3和安慰剂接受者中严重不良事件的比例为0.2%,且与疫苗无关[213]。
我国于2020年新上市冻干鼻喷流感减毒活疫苗,疫苗Ⅲ期临床试验结果提示,4 500名3~17岁受试者接种1剂次LAIV3,安全性观察至接种后>6个月,发热、流涕/鼻塞为十分常见的不良反应(发生概率≥10%),咽痛、头痛、乏力或嗜睡、呕吐、食欲下降、咳嗽、上呼吸道感染、肌肉痛、恶心、烦躁为常见不良反应(1%≤发生概率<10%),变态反应、关节痛、鼻咽炎和寒战为偶见不良反应(0.1%≤发生概率<1%)。由于尚未开始在人群中使用,因此AEFI信息管理系统中尚无有关LAIV的不良反应事件报告。
(五) 疫苗成本效果、成本效益接种流感疫苗能有效减少流感相关门急诊、住院和死亡人数,继而降低治疗费用,产生明显的经济效益。一项系统综述总结了全球51项流感疫苗接种卫生经济学评价的结果[217],发现其中22项研究(分别有12、8和2项研究评估儿童、老年人和孕妇接种流感疫苗的成本效果)认为接种流感疫苗可节省成本;13项研究的成本效果<1万美元或成本效益比接近1(常用的成本效果评价标准:当成本效果比小于所在国家人均GDP时,认为干预措施极具有成本效果;当成本效果比为1~3倍人均GDP时,认为干预措施具有成本效果;当成本效果比>3倍人均GDP时,干预措施不具有成本效果);13项研究的成本效果为1万美元至5万美元或者成本效益比<6;3项研究的成本效果>5万美元。绝大部分研究认为儿童接种流感疫苗可节省成本或具有成本效果,在老年人和孕妇中接种流感疫苗具有较好的成本效果。另一项系统综述发现[218]:从全社会的角度,对儿童、孕产妇、高危人群和医务人员开展流感疫苗接种具有成本效果。
中国最新一项基于全国及各省的流感相关健康和经济负担、人口年龄结构、基础疾病患病情况、疫苗保护效果、就医行为等参数的模型研究,以1倍人均GDP(8 840美元)为支付意愿阈值,从全社会角度估计了全国及各区域(北方、东北、西北、东部、中部、南方和西南地区)老年人IIV3免费接种项目的成本效果,并测算了疫苗成本阈值(即具有成本效果的人均免疫接种成本上限,包括疫苗、冷链运输和储存、接种服务等),研究结果发现:在全国范围内,与自费接种相比,免费接种项目平均每年可减少19 812(95%UI:7 150~35 783)例流感相关ILI门急诊就诊,9 418(3 386~17 068)例流感相关SARI住院,以及8 800(5 300~11 667)例流感相关呼吸道疾病的超额死亡,避免70 212(42 106~93 635)质量调整生命年(quality-adjusted life year,QALY)损失;每获得一个QALY需多支付4 832(3 460~8 307)美元,低于1倍人均GDP;概率敏感性分析显示,为老年人提供免费流感疫苗接种具有成本效果的概率为98%,疫苗成本阈值为10.19(6.08~13.65)美元[219]。
我国尚无研究评估接种LAIV的卫生经济学效果。美国一项传播动力学模型评估了2~8岁儿童接种LAIV和IIV的成本效果,结果提示:当LAIV和IIV疫苗效果分别为83%和64%时,接种LAIV具有成本效果;但该结果高度依赖于2种疫苗的效果差异,当IIV疫苗效果超过LAIV时,则接种IIV更具有成本效果[220]。而法国基于传播动力学模型的研究显示,接种四价LAIV平均每年可避免613例流感相关死亡,每获得一个生命年需多支付18 001欧元,低于支付意愿阈值(31 000欧元),具有成本效果的概率为98%[221]。
(六) 疫苗相互作用我国目前对流感疫苗与其他疫苗联合接种免疫原性和安全性影响的研究相对较少。国外研究提示,成人同时接种13价肺炎球菌结合疫苗(PCV13)[222-223]、破伤风疫苗或百日咳疫苗[224]、IIV,可观察到疫苗反应性降低,但无明确临床意义。≥50岁人群中的研究发现,IIV与带状疱疹减毒活疫苗同时接种和间隔4周接种相比[225-226],产生的抗体反应基本相同。≥65岁人群中研究发现,同时接种IIV4和23价肺炎球菌多糖疫苗(PPSV23)[227]与间隔2周接种相比,同时接种组4~6周后对B亚型流感抗原的血清保护率较低,但在接种6个月后,4种流感抗原的血清保护率没有差异。此外,IIV与带状疱疹减毒活疫苗[225-226]、PCV13[222-223]、PPSV23[227-228]、破伤风类毒素[224]或百日咳疫苗[224]分别同时接种于成年人,具有可靠的安全性。也有研究指出,6~23月龄儿童中IIV与PCV13联合接种会导致接种后0~1 d发热风险增加[229],IIV与PCV7、PCV13、破伤风疫苗及百日咳疫苗联合使用会导致接种后0~1 d热性惊厥风险增加[230-231],但大多数此类发热反应发作短暂且预后良好[232]。
研究显示,儿童同时接种LAIV、麻腮风疫苗及水痘疫苗,与单独接种相比不会降低任何1种成分的免疫原性[233]。但另一项研究显示,儿童同时接种LAIV和麻腮风疫苗,会降低风疹疫苗的免疫应答水平[234]。
综上,现有研究提示,目前尚未发现影响灭活流感疫苗和联合接种疫苗的免疫原性和安全性的明确证据[235]。虽然目前LAIV与其他疫苗联合接种研究相对有限,但均未发现安全性问题。美国CDC也在其流感疫苗预防接种技术指南中推荐灭活流感疫苗可以与其他IIV及减毒活疫苗同时或依次接种,而减毒流感疫苗则需要间隔一定时间后才能接种其他减毒疫苗[236]。
四、2020-2021年度接种建议每年接种流感疫苗是预防流感最有效的措施。目前,流感疫苗在我国大多数地区属于非免疫规划疫苗,公民自费、自愿接种。2019年7月,健康中国行动推进委员会制定印发了《健康中国行动(2019-2030年)》,列出了15项重大行动,包括全方位干预健康影响因素、维护全生命周期健康和防控重大疾病3个领域。其中在“慢性呼吸系统疾病防治行动”中建议慢性呼吸系统疾病患者和老年人等高危人群主动接种流感疫苗和肺炎球菌疫苗,在“传染病及地方病防控行动”中,明确提出儿童、老年人、慢性病患者的免疫力低、抵抗力弱,是流感的高危人群,建议每年流感流行季节前在医生指导下接种流感疫苗,并鼓励有条件地区为≥60岁老年人、托幼机构幼儿、在校中小学生和中等专业学校学生免费接种流感疫苗,同时,要求保障流感疫苗供应。该行动计划为推进流感疫苗预防接种提供了指导意见和工作要求。
国家卫生健康委员会2019年印发的《2019-2020年流行季流感防控工作方案》(国卫疾控函〔2019〕777号)要求实施“强化监测预警、免疫重点人群、规范疫情处置、落实医疗救治、广泛宣传动员”的举措,全面开展流感防控,保护群众身体健康,推进健康中国建设。关于疫苗接种,一是明确重点人群,推进疫苗接种,要以儿童、老年人、医务人员等为重点人群,关注心血管疾病、慢性呼吸疾病、糖尿病等特定慢性病患者,优先进行推荐。二是优化预防接种服务,提高疫苗接种便利化,其中医疗机构采用设立接种点等便利措施,继续组织免费为本院医务人员接种流感疫苗;同时在诊疗过程中,医务人员主动向患者及家属科学推荐接种流感疫苗。三是加强疫苗政策研究,提高疫苗接种率,推动各地结合当地实际,研究制订接种政策,降低重点人群疫苗接种费用,提高疫苗接种率。
为提高公众对流感疾病特征、危害及疫苗预防作用的认识,逐步提高高危人群的疫苗覆盖率,各级疾控中心要积极组织开展科学普及、健康教育、风险沟通和疫苗政策推进活动,组织指导疫苗接种时,应重点把握好剂型选择、优先接种人群、接种程序、禁忌证和接种时机等技术环节。
(一) 抗原组份WHO推荐的2020-2021年度北半球基于鸡胚生产的三价流感疫苗组份为:A/Guangdong-Maonan/SWL1536/2019(H1N1)pdm09类似株、A/Hong Kong/2671/2019(H3N2)类似株和B/Washington/02/2019(Victoria系)类似株。IIV4组份包含乙型毒株的两个系,为上述3个毒株及B/Phuket/3073/2013(Yamagata系)类似株。与上一年度相比,甲型H1N1亚型、A(H3N2)亚型和乙型(Victoria系)病毒更换了毒株。
(二) 疫苗种类及适用年龄组我国批准上市的流感疫苗包括IIV3、LAIV3和IIV4,其中IIV3有裂解疫苗和亚单位疫苗,可用于≥6月龄人群接种,包括0.25 ml和0.5 ml两种剂型;LAIV3为冻干制剂,用于3~17岁人群,每剂次0.2 ml;IIV4为裂解疫苗,可用于≥36月龄人群接种,包括0.5 ml一种剂型。0.25 ml剂型含每种组份血凝素7.5 μg,适用于6~35月龄婴幼儿;0.5 ml剂型含每种组份血凝素15 μg,适用于≥36月龄的人群;0.2 ml剂型含A(H3N2)亚型和甲型H1N1两种减毒病毒滴度各不低于6.9 lg EID50(50% egg infectious dose,EID50),含B/Victoria系减毒病毒滴度≥6.4 lg EID50。对可接种不同类型、不同厂家疫苗产品的人群,可自愿接种任一种流感疫苗,无优先推荐。
(三) 建议优先接种人群流感疫苗安全、有效。原则上,接种单位应为≥6月龄所有愿意接种疫苗且无禁忌证的人提供免疫服务。往年,我国推荐孕妇、6月龄~5岁儿童、≥60岁老年人、慢性病患者等流感高风险人群和医务人员为优先接种人群。结合今年新冠肺炎疫情形势,为尽可能降低流感的危害和对新冠肺炎疫情防控的影响,推荐按照优先顺序对重点和高风险人群进行接种。具体建议:
1.医务人员:包括临床救治人员、公共卫生人员、卫生检疫人员等。新冠肺炎大流行期间的流感疫苗使用,应优先考虑保护医务人员。医务人员接种流感疫苗既可预防个人因感染流感导致工作效率低下或缺勤影响医疗机构运转,又可有效避免传染流感给同事或患者,保障和维持医疗机构的正常接诊和救治能力。
2.养老机构、长期护理机构、福利院等人群聚集场所脆弱人群及员工:对以上人员接种流感疫苗,可降低此类集体场所聚集性疫情发生的风险,减少新冠肺炎疫情排查难度和工作量,同时降低老年人群罹患流感及感染后发生严重临床结局的风险。
3.重点场所人群:托幼机构、中小学校的教师和学生,监所机构的在押人员及工作人员等是容易发生流感和新冠肺炎暴发疫情的重点场所,对此类场所人群接种流感疫苗,可降低人群罹患流感风险和流感聚集性疫情的发生,减少新冠肺炎疫情排查难度和工作量。
4.其他流感高风险人群:包括≥60岁的居家老年人、6月龄~5岁儿童、特定慢性病患者、<6月龄婴儿的家庭成员和看护人员、以及孕妇或在流感季节备孕的女性,降低此类高危人群罹患流感及感染后发生严重临床结局的风险。
(1)≥60岁的居家老年人:患流感后死亡风险最高,也是新冠感染后重症和病死的高危人群,是流感疫苗接种的重要目标人群。虽然较多证据表明,现有流感疫苗在老年人中的效果不如年轻成年人,但疫苗接种仍是目前降低老年人罹患流感的最有效手段。
(2)6~23月龄的婴幼儿:患流感后出现重症的风险高,流感住院负担重,应优先接种流感疫苗。疫苗在该年龄组的效果高度依赖于疫苗株与循环毒株的匹配程度。
(3)2~5岁儿童:流感疾病负担也较高,但低于<2岁儿童。该年龄组儿童接种流感疫苗后,其免疫应答反应通常优于<2岁儿童。
(4)慢性病患者:心血管疾病(单纯高血压除外)、慢性呼吸系统疾病、肝肾功能不全、血液病、神经系统疾病、神经肌肉功能障碍、代谢性疾病(包括糖尿病)等慢性病患者、患有免疫抑制疾病或免疫功能低下者,患流感后出现重症的风险很高,应优先接种流感疫苗。
(5)<6月龄婴儿的家庭成员和看护人员:由于现有流感疫苗不可以直接给<6月龄婴儿接种,该人群可通过母亲孕期接种和对婴儿的家庭成员和看护人员接种流感疫苗,以预防流感。
(6)孕妇或在流感季节备孕的女性:国内外大量研究证实孕妇罹患流感后发生重症、死亡和不良妊娠结局的风险更高,国外对孕妇在孕期任何阶段接种流感疫苗的安全性证据充分,同时接种疫苗对预防孕妇罹患流感及通过胎传抗体保护<6月龄婴儿的效果明确。但由于国内缺乏孕妇接种流感疫苗的安全性评价数据,我国上市的部分流感疫苗产品说明书仍将孕妇列为禁忌证。为降低我国孕妇罹患流感及严重并发症风险,本指南建议孕妇或在流感季节备孕的女性接种流感疫苗,孕妇可在妊娠任何阶段接种。
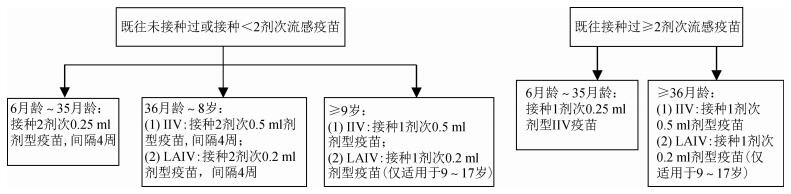
(四) 接种剂次1. 6月龄~8岁儿童:首次接种或既往接种<2剂次流感疫苗的6月龄~8岁儿童应接种2剂次,间隔≥4周,对IIV或LAIV均建议上述原则[130, 235-236];2019-2020年度或以前接种过≥2剂流感疫苗的儿童,则建议接种1剂[130, 235-236]。
2. ≥9岁儿童和成人:仅需接种1剂次。见图 1。
|
| 图 1 各年龄组流感疫苗接种剂次 |
通常接种流感疫苗2~4周后,可产生具有保护水平的抗体,6~8个月后抗体滴度开始衰减。我国各地每年流感活动高峰出现的时间和持续时间不同,为保证受种者在流感高发季节前获得免疫保护,建议各地在疫苗可及后尽快安排接种工作,最好在10月底前完成免疫接种;对10月底前未接种的对象,整个流行季节都可以提供免疫服务。同一流感流行季节,已按照接种程序完成全程接种的人员,无需重复接种。
孕妇在孕期的任一阶段均可接种流感疫苗,建议只要本年度的流感疫苗开始供应,可尽早接种。
(六) 接种部位及方法IIV接种采用肌肉注射(皮内注射制剂除外)[237-238]。成人和>1岁儿童首选上臂三角肌接种疫苗,6月龄~1岁婴幼儿的接种部位以大腿前外侧为最佳[237-238]。LAIV的接种采用鼻内喷雾法,严禁注射[238]。
(七) 疫苗储存按照《疫苗储存和运输管理规范(2017年版)》的要求,IIV及LAIV都应在2~8 ℃避光保存和运输,严禁冻结。
(八) 禁忌证对疫苗中所含任何成分(包括辅料、甲醛、裂解剂及抗生素)过敏者禁止接种。患伴或不伴发热症状的轻中度急性疾病者,建议症状消退后再接种。上次接种流感疫苗后6周内出现吉兰-巴雷综合征,不是禁忌证,但应特别注意。
以下人群不建议接种LAIV[236]:接种前48 h服用过流感抗病毒药物者;2~4岁患有哮喘的儿童;因使用药物、HIV感染等原因造成免疫功能低下者;需要与严重免疫功能低下者进行密切接触的人群;孕妇和使用阿司匹林或含有水杨酸成分药物治疗的儿童及青少年也禁止接种LAIV。
《中华人民共和国药典》(2015版和2020版)均未将对鸡蛋过敏者作为禁忌。药典规定流感全病毒灭活疫苗中卵清蛋白含量应不高于250 ng/剂,裂解疫苗中卵清蛋白含量应不高于200 ng/ml,未见减毒活疫苗说明。我国常用的流感疫苗中的卵蛋白含量测量显示含量最高不超过140ng/ml[239]。国外学者对于鸡蛋过敏者接种IIV或LAIV的研究表明未见发生严重过敏反应[240-244]。美国ACIP自2016年以来开始建议对鸡蛋过敏者亦可接种流感疫苗[130, 235-236, 238]。
(九) 药物相互作用综合考虑风险与收益,灭活流感疫苗与其他灭活疫苗及减毒活疫苗如肺炎球菌疫苗、带状疱疹减毒活疫苗、水痘疫苗、麻腮风疫苗、百白破疫苗可同时在不同部位接种[245];但在接种流感减毒活疫苗后,必须间隔>28 d才可接种其他减毒活疫苗[130, 235-236, 238]。>65岁老年人可同时接种流感疫苗和肺炎球菌疫苗[246-251]。
另外,如正在或近期曾使用过任何其他疫苗或药物,包括非处方药,请接种前告知接种医生。免疫抑制剂(如皮质类激素、细胞毒性药物或放射治疗)的使用可能影响接种后的免疫效果[252-253]。为避免可能的药物间相互作用,任何正在进行的治疗均应咨询医生。服用流感抗病毒药物预防和治疗期间也可以接种灭活流感疫苗[130, 235-236]。
(十) 接种注意事项各接种单位要按照《预防接种工作规范》的要求开展流感疫苗接种工作。接种过程应遵循“三查七对一验证”的原则,同时要注意以下事项:
1.疫苗瓶有裂纹、标签不清或失效者,疫苗出现浑浊等外观异物者均不得使用。
2.严格掌握疫苗剂量和适用人群的年龄范围,不能将0.5 ml剂型分为2剂次(每剂次0.25 ml)给2名婴幼儿接种。
3.国外同类产品显示哮喘患者(任何年龄)、活动性喘息或反复喘息发作的儿童(<5岁)接种LAIV后喘息发作的风险增高,国内临床试验没有此类受试者的数据,建议慎用。
4. LAIV为鼻内喷雾接种,严禁注射。
5. LAIV与其他减毒活疫苗接种应至少间隔4周。
6.接种完成后应告知接种对象留下观察≥30 min再离开。
7.建议注射现场备1:1 000肾上腺素等药品和其他抢救设施,以备偶有发生严重过敏反应时供急救使用。
利益冲突 所有作者均声明不存在利益冲突
指南编写专家组:中国疾病预防控制中心传染病管理处彭质斌、郑亚明、郑建东、秦颖;中国疾病预防控制中心病毒病预防控制所王大燕、陈涛;中国医学科学院北京协和医学院群医学及公共卫生学院冯录召;北京市疾病预防控制中心传染病地方病控制所杨鹏;复旦大学公共卫生学院杨娟;河南省疾病预防控制中心免疫预防与规划所张延炀;上海市疾病预防控制中心传染病防治所陈健;深圳市南山区疾病预防控制中心免疫规划科姜世强;青海省疾病预防控制中心传染病预防控制所徐莉立;广东省疾病预防控制中心传染病预防控制所康敏
指南编写专家组秘书:中国疾病预防控制中心传染病管理处杨孝坤
审定专家:中国疾病预防控制中心李中杰、冯子健
志谢 感谢中国疾病预防控制中心Lawrence Everett Rodewald、马超
| [1] |
中华人民共和国国家卫生和计划生育委员会. 流行性感冒诊疗方案(2018年版)[J]. 中华临床感染病杂志, 2018(1): 1-5. National Health and Family Planning Commission of the People's Republic of China. Protocol for diagnosis and treatment of influenza (2018 revised version)[J]. Chin J Clin Infect Dis, 2018(1): 1-5. DOI:10.3760/cma.j.issn.1674-2397.2018.01.001 |
| [2] |
Bischoff WE, Swett K, Leng I, et al. Exposure to influenza virus aerosols during routine patient care[J]. J Infect Dis, 2013, 207(7): 1037-1046. DOI:10.1093/infdis/jis773 |
| [3] |
World Health Organization (WHO). Influenza (Seasonal)[EB/OL]. (2018-11-06)[2020-08-20]. https://www.who.int/en/news-room/fact-sheets/detail/influenza-(seasonal).
|
| [4] |
李茜, 李霆, 吴绍强, 等. D型流感病毒研究概述[J]. 检验检疫学刊, 2017, 27(4): 73-75. Li Q, Li T, Wu SQ, et al. An overview of research progress on influenza D viruses Overview of Research on Influenza Virus D[J]. J Inspec Quar, 2017, 27(4): 73-75. |
| [5] |
Hause BM, Collin EA, Liu R, et al. Characterization of a novel influenza virus in cattle and Swine:proposal for a new genus in the Orthomyxoviridae family[J]. MBio, 2014, 5(2): e00031-00014. DOI:10.1128/mBio.00031-14 |
| [6] |
World Health Organization. Vaccines against influenza WHO position paper-November 2012[J]. Wkly Epidemiol Rec, 2012, 87(47): 461-476. |
| [7] |
Nicholson KG, Wood JM, Zambon M. Influenza[J]. Lancet, 2003, 362(9397): 1733-1745. DOI:10.1016/s0140-6736(03)14854-4 |
| [8] |
Kim DK, Poudel B. Tools to detect influenza virus[J]. Yonsei Med J, 2013, 54(3): 560-566. DOI:10.3349/ymj.2013.54.3.560 |
| [9] |
Kelso JM. Safety of influenza vaccines[J]. Curr Opin Allergy Clin Immunol, 2012, 12(4): 383-388. DOI:10.1097/ACI.0b013e328354395d |
| [10] |
Bell D, Nicoll A, Fukuda K, et al. Non-pharmaceutical interventions for pandemic influenza, international measures[J]. Emerg Infect Dis, 2006, 12(1): 81-87. DOI:10.3201/eid1201.051370 |
| [11] |
Lau LL, Ip DK, Nishiura H, et al. Heterogeneity in viral shedding among individuals with medically attended influenza A virus infection[J]. J Infect Dis, 2013, 207(8): 1281-1285. DOI:10.1093/infdis/jit034 |
| [12] |
Carrat F, Vergu E, Ferguson NM, et al. Time lines of infection and disease in human influenza:a review of volunteer challenge studies[J]. Am J Epidemiol, 2008, 167(7): 775-785. DOI:10.1093/aje/kwm375 |
| [13] |
Lipsitch M, Viboud C. Influenza seasonality:lifting the fog[J]. Proc Natl Acad Sci USA, 2009, 106(10): 3645-3646. DOI:10.1073/pnas.0900933106 |
| [14] |
Viboud C, Alonso WJ, Simonsen L. Influenza in tropical regions[J]. PLoS Med, 2006, 3(4): e89. DOI:10.1371/journal.pmed.0030089 |
| [15] |
Azziz Baumgartner E, Dao CN, Nasreen S, et al. Seasonality, timing, and climate drivers of influenza activity worldwide[J]. J Infect Dis, 2012, 206(6): 838-846. DOI:10.1093/infdis/jis467 |
| [16] |
Bloom-Feshbach K, Alonso WJ, Charu V, et al. Latitudinal variations in seasonal activity of influenza and respiratory syncytial virus (RSV):a global comparative review[J]. PLoS One, 2013, 8(2): e54445. DOI:10.1371/journal.pone.0054445 |
| [17] |
Zou J, Yang H, Cui H, et al. Geographic divisions and modeling of virological data on seasonal influenza in the Chinese mainland during the 2006-2009 monitoring years[J]. PLoS One, 2013, 8(3): e58434. DOI:10.1371/journal.pone.0058434 |
| [18] |
Yu H, Alonso WJ, Feng LZ, et al. Characterization of regional influenza seasonality patterns in China and implications for vaccination strategies:spatio-temporal modeling of surveillance data[J]. PLoS Med, 2013, 10(11): e1001552. DOI:10.1371/journal.pmed.1001552 |
| [19] |
Yang J, Lau YC, Wu P, et al. Variation in Influenza B Virus Epidemiology by Lineage, China[J]. Emerg Infect Dis, 2018, 24(8): 1536-1540. DOI:10.3201/eid2408.180063 |
| [20] |
Somes MP, Turner RM, Dwyer LJ, et al. Estimating the annual attack rate of seasonal influenza among unvaccinated individuals:A systematic review and Meta-analysis[J]. Vaccine, 2018, 36(23): 3199-3207. DOI:10.1016/j.vaccine.2018.04.063 |
| [21] |
Feng L, Feng S, Chen T, et al. Burden of influenza-associated outpatient influenza-like illness consultations in China, 2006-2015:A population-based study[J]. Influenza Other Respir Viruses, 2020, 14(2): 162-172. DOI:10.1111/irv.12711 |
| [22] |
张惺惺, 吴双胜, 王全意, 等. 北京市2017-2018流行季流感感染率和发病率研究[J]. 国际病毒学杂志, 2019, 26(2): 73-76. Zhang XX, Wu SS, Wang QY, et al. Estimated infection rates and incidence rates of seasonal influenza in Beijing during the 2017-2018 influenza season[J]. Int J Virol, 2019, 26(2): 73-76. DOI:10.3760/cma.j.issn.1673-4092.2019.02.001 |
| [23] |
Iuliano AD, Roguski KM, Chang HH, et al. Estimates of global seasonal influenza-associated respiratory mortality:a modelling study[J]. Lancet, 2018, 391(10127): 1285-1300. DOI:10.1016/s0140-6736(17)33293-2 |
| [24] |
Li L, Liu YN, Peng W, et al. Influenza-associated excess respiratory mortality in China, 2010-15:a population-based study[J]. Lancet Public Health, 2019, 4(9): e473-481. DOI:10.1016/S2468-2667(19)30163-X |
| [25] |
李飒, 刘思家, 朱爱琴, 等. 中国流感死亡负担研究系统综述[J]. 中华预防医学杂志, 2019, 53(10): 1049-1055. Li S, Liu SJ, Zhu AQ, et al. The mortality burden of influenza in China:a systematic review Systematic review of Influenza death burden in China[J]. Chin J Prev Med, 2019, 53(10): 1049-1055. DOI:10.3760/cma.j.issn.0253-9624.2019.10.018 |
| [26] |
Bauch CT, Puig-Barberà J, Natividad-Sancho A, et al. Epidemiology of Hospital Admissions with Influenza during the 2013/2014 Northern Hemisphere Influenza Season:Results from the Global Influenza Hospital Surveillance Network[J]. PLoS One, 2016, 11(5): e0154970. DOI:10.1371/journal.pone.0154970 |
| [27] |
Zou QD, Zheng SF, Wang XC, et al. Influenza A-associated severe pneumonia in hospitalized patients:Risk factors and NAI treatments[J]. Int J Infect Dis, 2020, 92: 208-213. DOI:10.1016/j.ijid.2020.01.017 |
| [28] |
Homaira N, Briggs N, Oei JL, et al. Impact of influenza on hospitalization rates in children with a range of chronic lung diseases[J]. Influenza Other Respir Viruses, 2019, 13(3): 233-239. DOI:10.1111/irv.12633 |
| [29] |
Plans-Rubió P. Prevention and control of influenza in persons with chronic obstructive pulmonary disease[J]. Int J Chron Obstruct Pulmon Dis, 2007, 2(1): 41-53. DOI:10.2147/copd.2007.2.1.41 |
| [30] |
Liu WD, Yeh CY, Shih MC, et al. Clinical manifestations and risk factors for mortality of patients with severe influenza during the 2016-2018 season[J]. Int J Infect Dis, 2020, 95: 347-351. DOI:10.1016/j.ijid.2020.04.013 |
| [31] |
Racicot K, Kwon JY, Aldo P, et al. Understanding the complexity of the immune system during pregnancy[J]. Am J Reprod Immunol, 2014, 72(2): 107-116. DOI:10.1111/aji.12289 |
| [32] |
Pillay PS, Piercy CN, Tolppanen H, et al. Physiological changes in pregnancy[J]. Cardiovasc J Afr, 2016, 27(2): 89-94. DOI:10.5830/CVJA-2016-021 |
| [33] |
Sappenfield E, Jamieson DJ, Kourtis AP. Pregnancy and susceptibility to infectious diseases[J]. Infect Dis Obstet Gynecol, 2013, 2013: 752852. DOI:10.1155/2013/752852 |
| [34] |
Goodnight WH, Soper DE. Pneumonia in pregnancy[J]. Crit Care Med, 2005, 33(10): 390-397. DOI:10.1097/01.ccm.0000182483.24836.66 |
| [35] |
Ohfuji S, Deguchi M, Tachibana D, et al. Estimating influenza disease burden among pregnant women:Application of self-control method[J]. Vaccine, 2017, 35(36): 4811-4816. DOI:10.1016/j.vaccine.2017.07.006 |
| [36] |
Lindley MC, Kahn KE, Bardenheier BH, et al. Vital Signs:Burden and Prevention of Influenza and Pertussis Among Pregnant Women and Infants-United States[J]. MMWR Morb Mortal Wkly Rep, 2019, 68(40): 885-892. DOI:10.15585/mmwr.mm6840e1 |
| [37] |
Mertz D, Lo CK, Lytvyn L, et al. Pregnancy as a risk factor for severe influenza infection:an individual participant data Meta-analysis[J]. BMC Infect Dis, 2019, 19(1): 683. DOI:10.1186/s12879-019-4318-3 |
| [38] |
Callaghan WM, Chu SY, Jamieson DJ. Deaths from seasonal influenza among pregnant women in the United States, 1998-2005[J]. Obstet Gynecol, 2010, 115(5): 919-923. DOI:10.1097/AOG.0b013e3181d99d85 |
| [39] |
Vilca LM, Verma A, Bonati M, et al. Impact of influenza on outpatient visits and hospitalizations among pregnant women in Catalonia, Spain[J]. J Infect, 2018, 77(6): 553-560. DOI:10.1016/j.jinf.2018.06.015 |
| [40] |
Yu HJ, Feng ZJ, Uyeki TM, et al. Risk factors for severe illness with 2009 pandemic influenza A (H1N1) virus infection in China[J]. Clin Infect Dis, 2011, 52(4): 457-465. DOI:10.1093/cid/ciq144 |
| [41] |
Luteijn JM, Brown MJ, Dolk H. Influenza and congenital anomalies:a systematic review and Meta-analysis[J]. Hum Reprod, 2014, 29(4): 809-823. DOI:10.1093/humrep/det455 |
| [42] |
Steinhoff MC, MacDonald N, Pfeifer D, et al. Influenza vaccine in pregnancy:policy and research strategies[J]. Lancet, 2014, 383(9929): 1611-1613. DOI:10.1016/S0140-6736(14)60583-3 |
| [43] |
He J, Liu ZW, Lu YP, et al. A Systematic Review and Meta-Analysis of Influenza A Virus Infection During Pregnancy Associated with an Increased Risk for Stillbirth and Low Birth Weight[J]. Kidney Blood Press Res, 2017, 42(2): 232-243. DOI:10.1159/000477221 |
| [44] |
Fraaij PL, Heikkinen T. Seasonal influenza:the burden of disease in children[J]. Vaccine, 2011, 29(43): 7524-7528. DOI:10.1016/j.vaccine.2011.08.010 |
| [45] |
Monto AS, Koopman JS, Longini IM Jr. Tecumseh study of illness[J]. Am J Epidemiol. DOI:10.1093/oxfordjournals.aje.a114052 |
| [46] |
Cowling BJ, Perera RA, Fang VJ, et al. Incidence of influenza virus infections in children in Hong Kong in a 3-year randomized placebo-controlled vaccine study, 2009-2012[J]. Clin Infect Dis, 2014, 59(4): 517-524. DOI:10.1093/cid/ciu356 |
| [47] |
高君玫, 陈立凌, 田健美, 等. 2011-2017年苏州市区 < 5岁儿童流感相关门诊就诊率的估计[J]. 中华疾病控制杂志, 2019, 23(1): 34-38. Gao JM, Chen LL, Tian JM, et al. The estimation of influenza-related outpatient rate in children under 5 years in Suzhou from 2011 to 2017[J]. Chin J Dis Cont Prev, 2019, 23(1): 34-38. DOI:10.13315/j.cnki.zhjcep.2019.01.008 |
| [48] |
Wang X, Li Y, O'Brien KL, et al. Global burden of respiratory infections associated with seasonal influenza in children under 5 years in 2018:a systematic review and modelling study[J]. Lancet Glob Health, 2020, 8(4): e497-510. DOI:10.1016/s2214-109x(19)30545-5 |
| [49] |
Yu HJ, Huang JG, Huai Y, et al. The substantial hospitalization burden of influenza in central China:surveillance for severe, acute respiratory infection, and influenza viruses, 2010-2012[J]. Influenza Other Respir Viruses, 2014, 8(1): 53-65. DOI:10.1111/irv.12205 |
| [50] |
Yu J, Zhang XY, Shan W, et al. Influenza-associated Hospitalization in Children Younger Than 5 Years of Age in Suzhou, China, 2011-2016[J]. Pediatr Infect Dis J, 2019, 38(5): 445-452. DOI:10.1097/inf.0000000000002178 |
| [51] |
Finnie TJ, Copley VR, Hall IM, et al. An analysis of influenza outbreaks in institutions and enclosed societies[J]. Epidemiol Infect, 2014, 142(1): 107-113. DOI:10.1017/s0950268813000733 |
| [52] |
Gaglani MJ. Editorial commentary:school-located influenza vaccination:why worth the effort?[J]. Clin Infect Dis, 2014, 59(3): 333-335. DOI:10.1093/cid/ciu344 |
| [53] |
Fiore AE, Epperson S, Perrotta D, et al. Expanding the recommendations for annual influenza vaccination to school-age children in the United States[J]. Pediatrics, 2012, 129. DOI:10.1542/peds.2011-0737C |
| [54] |
Wu S, L VANA, Wang L, et al. Estimated incidence and number of outpatient visits for seasonal influenza in 2015-2016 in Beijing, China[J]. Epidemiol Infect, 2017, 145(16): 3334-3344. DOI:10.1017/s0950268817002369 |
| [55] |
Neuzil KM, Hohlbein C, Zhu Y. Illness among schoolchildren during influenza season:effect on school absenteeism, parental absenteeism from work, and secondary illness in families[J]. Arch Pediatr Adolesc Med, 2002, 156(10): 986-991. DOI:10.1001/archpedi.156.10.986 |
| [56] |
Chiu SS, Chan KH, So LY, et al. The population based socioeconomic burden of pediatric influenza-associated hospitalization in Hong Kong[J]. Vaccine, 2012, 30(10): 1895-900. DOI:10.1016/j.vaccine.2011.12.027 |
| [57] |
Kuster SP, Shah PS, Coleman BL, et al. Incidence of influenza in healthy adults and healthcare workers:a systematic review and Meta-analysis[J]. PLoS One, 2011, 6(10): e26239. DOI:10.1371/journal.pone.0026239 |
| [58] |
Lietz J, Westermann C, Nienhaus A, et al. The Occupational Risk of Influenza A (H1N1) Infection among Healthcare Personnel during the 2009 Pandemic:A Systematic Review and Meta-Analysis of Observational Studies[J]. PLoS One, 2016, 11(8): e0162061. DOI:10.1371/journal.pone.0162061 |
| [59] |
Jenkin DC, Mahgoub H, Morales KF, et al. A Rapid Evidence Appraisal of influenza vaccination in health workers:an important policy in an area of imperfect evidence[J]. Vaccine:X, 2019, 2: 100036. DOI:10.1016/j.jvacx.2019.100036 |
| [60] |
Kumar S, Fan J, Melzer-Lange M, et al. H1N1 hemagglutinin-inhibition seroprevalence in Emergency Department Health Care workers after the first wave of the 2009 influenza pandemic[J]. Pediatr Emerg Care, 2011, 27(9): 804-807. DOI:10.1097/PEC.0b013e31822c125e |
| [61] |
Salgado CD, Farr BM, Hall KK, et al. Influenza in the acute hospital setting[J]. Lancet Infect Dis, 2002, 2(3): 145-155. DOI:10.1016/s1473-3099(02)00221-9 |
| [62] |
Elder AG, O'Donnell B, Mccruden EAB, et al. Incidence and recall of influenza in a cohort of Glasgow healthcare workers during the 1993-4 epidemic:results of serum testing and questionnaire[J]. BMJ, 1996, 313(7067): 1241-1242. DOI:10.1136/bmj.313.7067.1241 |
| [63] |
Pereira M, Williams S, Restrick L, et al. Healthcare worker influenza vaccination and sickness absence-an ecological study[J]. Clin Med (Lond), 2017, 17(6): 484-489. DOI:10.7861/clinmedicine.17-6-484 |
| [64] |
Nielsen J, Vestergaard LS, Richter L, et al. European all-cause excess and influenza-attributable mortality in the 2017/18 season:should the burden of influenza B be reconsidered?[J]. Clin Microbiol Infect, 2019, 25(10): 1266-1276. DOI:10.1016/j.cmi.2019.02.011 |
| [65] |
Wang H, Fu CX, Li KB, et al. Influenza associated mortality in Southern China, 2010-2012[J]. Vaccine, 2014, 32(8): 973-978. DOI:10.1016/j.vaccine.2013.12.013 |
| [66] |
Yang L, Ma S, Chen PY, et al. Influenza associated mortality in the subtropics and tropics:Results from three Asian cities[J]. Vaccine, 2011, 29(48): 8909-8914. DOI:10.1016/j.vaccine.2011.09.071 |
| [67] |
Wu P, Goldstein E, Ho LM, et al. Excess mortality associated with influenza A and B virus in Hong Kong, 1998-2009[J]. J Infect Dis, 2012, 206(12): 1862-1871. DOI:10.1093/infdis/jis628 |
| [68] |
Chow A, Ma S, Ling AE, et al. Influenza-associated deaths in tropical Singapore[J]. Emerging Infectious Diseases, 2006, 12(1): 114-121. DOI:10.3201/eid1201.050826 |
| [69] |
Nunes B, Viboud C, Machado A, et al. Excess Mortality Associated with Influenza Epidemics in Portugal, 1980 to 2004[J]. PLoS One, 2011, 6(6): e20661. DOI:10.1371/journal.pone.0020661 |
| [70] |
Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States[J]. JAMA, 2003, 289(2): 179-186. DOI:10.1001/jama.289.2.179 |
| [71] |
Feng LZ, Shay DK, Jiang Y, et al. Influenza-associated mortality in temperate and subtropical Chinese cities, 2003-2008[J]. Bull World Health Organ, 2012, 90(4): 279-288B. DOI:10.2471/blt.11.096958 |
| [72] |
Yu HJ, Huang JG, Huai Y, et al. The substantial hospitalization burden of influenza in central C hina:surveillance for severe, acute respiratory infection, and influenza viruses, 2010-2012[J]. Influenza Other Respir Viruses, 2014, 8(1): 53-65. DOI:10.1111/irv.12205 |
| [73] |
徐郁, 周伴群, 周勇, 等.珠海市甲型H1N1流感患者经济负担分析[J].实用预防医学, 2012, 19(6):827-829. DOI:10.3969/j.issn.1006-3110.2012.06.009. Xu Y, Zhou BQ, Zhou Y, et al. Estimation of Economic Burden of Pandemic Influenza A (H1N1) in Zhuhai, 2012, 19(6): 827-829. DOI: 10.3969/j.issn.1006-3110.2012.06.009. |
| [74] |
郑慧贞, 郭汝宁, 李灵辉, 等. 广东省城乡居民流感样疾病2周患病及经济负担人户调查[J]. 现代预防医学, 2010(2): 201-203. Zheng HZ, Guo RN, Li LH, et al. Household Survey of 2-Week-Incidence and Economic Burden for Influenza-like Illness in Guangdong Residents[J]. Mod Prev Med, 2010(2): 201-203. |
| [75] |
Guo RN, Z ZH, Li JS, et al. A population-based study on incidence and economic burden of influenza-like illness in south China, 2007[J]. Public Health, 2011, 125(6): 389-395. DOI:10.1016/j.puhe.2011.03.004 |
| [76] |
田雪莹, 王显军, 张圣洋, 等. 183例甲型H1N1流感确诊病例住院费用及影响因素分析[J]. 中国卫生经济, 2012, 31(07): 34-36. Tian XY, Wang XJ, Zhang SX, et al. Analysis of the Cost and its Related Factors of 183 Laboratory-confirmed Influenza A H1N1 Cases[J]. Chin Heal Econ, 2012, 31(7): 34-36. DOI:10.3969/j.issn.1003-0743.2012.07.011 |
| [77] |
于佳, 张涛, 王胤, 等. 苏州市2011-2017年 < 5岁儿童流感门诊病例临床特征及疾病负担[J]. 中华流行病学杂志, 2018, 39(6): 847-851. Yu J, Zhang T, Wang Y, et al. Clinical characteristics and economic burden of influenza among children under 5 years old, in Suzhou, 2011-2017[J]. Chin J Epidemiol, 2018, 39(6): 847-851. DOI:10.3760/cma.j.issn.0254-6450.2018.06.029 |
| [78] |
Wang D, Zhang T, Wu J, et al. Socio-economic burden of influenza among children younger than 5 years in the outpatient setting in Suzhou, China[J]. PLoS One, 2013, 8(8): e69035. DOI:10.1371/journal.pone.0069035 |
| [79] |
Zhang X, Zhang J, Chen L, et al. Pneumonia and influenza hospitalizations among children under 5 years of age in Suzhou, China, 2005-2011[J]. Influenza Other Respir Viruses, 2017, 11(1): 15-22. DOI:10.1111/irv.12405 |
| [80] |
何晓定, 徐云蕴, 李颖, 等. 上海市长宁区某医院流感样病例的经济负担分析[J]. 中国初级卫生保健, 2012, 26(10): 75-76. He XD, Xu YY, Li Y, et al. Economic Burden Analysis of ILI Cases in Changning District, Shanghai,[J]. Chin Prim Health Care, 2012, 26(10): 75-76. |
| [81] |
王相诗, 蔡洁皓, 姚玮蕾, 等. 上海地区某医院门诊儿童流感社会经济负担调查[J]. 中华流行病学杂志, 2015, 36(1): 27-30. Wang XS, Cai JH, Yao WL, et al. Socio-economic impact of influenza in children:a single-centered hospital study in Shanghai[J]. Chin J Epidemiol, 2015, 36(1): 27-30. DOI:10.3760/cma.j.issn.0254-6450.2015.01.007 |
| [82] |
张涛, 蔡华, 顾宝柯, 等. 上海市甲型H1N1流感患者经济负担估计[J]. 中国卫生经济, 2011, 30(5): 25-28. Zhang T, Cai H, Gu BK, et al. Economic Burden Estimation of Pandemic Influenza A H1N1 in Shanghai[J]. Chin Health Econ, 2011, 30(5): 25-38. DOI:10.3969/j.issn.1003-0743.2011.05.009 |
| [83] |
Chen J, Li YT, Gu BK, et al. Estimation of the Direct Cost of Treating People Aged More Than 60 Years Infected by Influenza Virus in Shanghai[J]. Asia Pacific J Public Health, 2012, 27(2): NP936-946. DOI:10.1177/1010539512460269 |
| [84] |
王慎玉, 甘正凯, 邵燕志, 等. 2016-2018年杭州市农村地区学校和幼托机构流感疾病负担研究[J]. 中华预防医学杂志, 2019, 53(7): 713-718. Wang SY, Gan ZK, Shao YZ, et al. Disease burden of influenza in schools and child care settings in rural areas of Hangzhou, 2016-2018[J]. Chin J Prev Med, 2019, 53(7): 713-718. DOI:10.3760/cma.j.issn.0253-9624.2019.07.011 |
| [85] |
李琳, 张颖, 董晓春, 等. 2015年天津市流感确诊病例流行病学特征分析及疾病负担评估[J]. 职业与健康, 2017, 33(2): 216-218, 222. Li L, Zhang Y, Dong XC, et al. Analysis on epidemiological characteristics and evaluation on disease burden of confirmed influenza cases in Tianjin in 2015[J]. Occup Health, 2017, 33(2): 216-218, 222. DOI:10.13329/j.cnki.zyyjk.2017.0064 |
| [86] |
董晓春, 徐文体, 李琳, 等. 基于天津市汉沽街社区流行性感冒监测结果的疾病负担研究[J]. 疾病监测, 2011, 26(10): 785-787. Dong XC, Xu WT, Li L, et al. Disease burden based on community influenza surveillance in Hangu street, Tianjin municipality[J]. Dis Surveill, 2011, 26(10): 785-787. DOI:10.3784/j.issn.1003-9961.2011.10.009 |
| [87] |
孙淑苍, 王文娟, 王德全, 等. 流行性感冒流行期间学生缺课率、带病上课率、医药费用及疫苗接种效果调查[J]. 中华流行病学杂志, 2003, 24(3): 243. Sun SC, Wang WJ, Wang DQ, et al. Investigation on the rate of students' absenteeism, attendance rate with illness, medical expenses and effect of vaccination during influenza epidemic[J]. Chin J Epidemiol, 2003, 24(3): 243. |
| [88] |
吴双胜, 王全意, 马春娜, 等. 北京市成年流感样病例就诊行为及其经济负担研究[J]. 国际病毒学杂志, 2019, 26(2): 82-86. Wu SS, Wang QY, Ma CN, et al. Medical-seeking behaviors and economic burden of adult influenza-like illness cases in Beijing[J]. Int J Virol, 2019, 26(2): 82-86. DOI:10.3760/cma.j.issn.1673-4092.2019.02.003 |
| [89] |
朱爱琴, 郑亚明, 秦颖, 等. 中国流感经济负担研究系统综述[J]. 中华预防医学杂志, 2019, 53(10): 1043-1048. Zhu AQ, Zheng YM, Qin Y, et al. A systematic review of the economic burden of influenza in China[J]. Chin J Prev Med, 2019, 53(10): 1043-1048. DOI:10.3760/cma.j.issn.0253-9624.2019.10.017 |
| [90] |
Zhou L, Situ S, Huang T, et al. Direct medical cost of influenza-related hospitalizations among severe acute respiratory infections cases in three provinces in China[J]. PLoS One, 2013, 8(5): e63788. DOI:10.1371/journal.pone.0063788 |
| [91] |
Yang J, Jit M, Leung KS, et al. The economic burden of influenza-associated outpatient visits and hospitalizations in China:a retrospective survey[J]. Infect Dis Poverty, 2015, 4: 44. DOI:10.1186/s40249-015-0077-6 |
| [92] |
Yang J, Jit M, Zheng Y, et al. The impact of influenza on the health related quality of life in China:an EQ-5D survey[J]. BMC Infect Dis, 2017, 17(1): 686. DOI:10.1186/s12879-017-2801-2 |
| [93] |
Chan SS. Does vaccinating ED health care workers against influenza reduce sickness absenteeism?[J]. Am J Emerg Med, 2007, 25(7): 808-811. DOI:10.1016/j.ajem.2007.02.002 |
| [94] |
于佳, 张涛, 王胤, 等. 苏州市2011-2017年 < 5岁儿童流感门诊病例临床特征及疾病负担[J]. 中华流行病学杂志, 2018, 39(6): 847-851. Yu J, Zhang T, Wang Y, et al. Clinical characteristics and economic burden of influenza among children under 5 years old, in Suzhou, 2011-2017[J]. Chin J Epidemiol, 2018, 39(6): 847-851. DOI:10.3760/cma.j.issn.0254-6450.2018.06.029 |
| [95] |
Li S, Li L, Ai X, et al. A randomized, controlled, blinded study of the safety, immunogenicity and batch consistency of Aleph inactivated split influenza vaccine made in China in Chinese people[J]. Hum Vaccin Immunother, 2014, 10(3): 557-565. DOI:10.4161/hv.27329 |
| [96] |
Hu YM, Shao M, Hu YS, et al. Immunogenicity and safety of an inactivated quadrivalent influenza vaccine:a randomized, double-blind, controlled phase Ⅲ clinical trial in children aged 6-35 months in China[J]. Hum Vaccin Immunother, 2020, 16(7): 1691-1698. DOI:10.1080/21645515.2020.1721994 |
| [97] |
Zhu FC, Zhou WZ, Pan HX, et al. Safety and immunogenicity of two subunit influenza vaccines in healthy children, adults and the elderly:a randomized controlled trial in China[J]. Vaccine, 2008, 26(35): 4579-4584. DOI:10.1016/j.vaccine.2008.05.082 |
| [98] |
He XS, Holmes TH, Zhang C, et al. Cellular Immune Responses in Children and Adults Receiving Inactivated or Live Attenuated Influenza Vaccines[J]. J Virol, 2006, 80(23): 11756-11766. DOI:10.1128/jvi.01460-06 |
| [99] |
Mohn KG, Brokstad KA, Islam S, et al. Early Induction of Cross-Reactive CD8+T-Cell Responses in Tonsils After Live-Attenuated Influenza Vaccination in Children[J]. J Infect Dis, 2020, 221(9): 1528-1537. DOI:10.1093/infdis/jiz583 |
| [100] |
Wen F, Guo JY, Huang SJ. A Meta-analysis identified genes responsible for distinct immune responses to trivalent inactivated and live attenuated influenza vaccines[J]. J Cell Physiol, 2019, 234(4): 5196-5202. DOI:10.1002/jcp.27327 |
| [101] |
Lindsey BB, Jagne YJ, Armitage EP, et al. Effect of a Russian-backbone live-attenuated influenza vaccine with an updated pandemic H1N1 strain on shedding and immunogenicity among children in The Gambia:an open-label, observational, phase 4 study[J]. Lancet Respir Med, 2019, 7(8): 665-676. DOI:10.1016/S2213-2600(19)30086-4 |
| [102] |
Coelingh K, Olajide IR, MacDonald P, et al. Efficacy and effectiveness of live attenuated influenza vaccine in school-age children[J]. Expert Rev Vaccines, 2015, 14(10): 1331-1346. DOI:10.1586/14760584.2015.1078732 |
| [103] |
Osterholm MT, Kelley NS, Sommer A, et al. Efficacy and effectiveness of influenza vaccines:a systematic review and Meta-analysis[J]. Lancet Infect Dis, 2012, 12(1): 36-44. DOI:10.1016/S1473-3099(11)70295-X |
| [104] |
Demicheli V, Jefferson T, Ferroni E, et al. Vaccines for preventing influenza in healthy adults[J]. Cochrane Database Syst Rev, 2018, 2: CD001269. DOI:10.1002/14651858.CD001269.pub6 |
| [105] |
星一, 刘民. 流感灭活疫苗在中国应用效果的Meta分析[J]. 中华流行病学杂志, 2009, 30(4): 368-370. Xing Y, Liu M. Meta analysis on the effectiveness of inactivated influenza vaccine[J]. Chin J Epidemiol, 2009, 30(4): 368-370. DOI:10.3760/cma.j.issn.0254-6450.2009.04.015 |
| [106] |
Belongia EA, Simpson MD, King JP, et al. Variable influenza vaccine effectiveness by subtype:a systematic review and Meta-analysis of test-negative design studies[J]. Lancet Infect Dis, 2016, 16(8): 942-951. DOI:10.1016/s1473-3099(16)00129-8 |
| [107] |
Moa AM, Chughtai AA, Muscatello DJ, et al. Immunogenicity and safety of inactivated quadrivalent influenza vaccine in adults:A systematic review and Meta-analysis of randomised controlled trials[J]. Vaccine, 2016, 34(35): 4092-4102. DOI:10.1016/j.vaccine.2016.06.064 |
| [108] |
Bekkat-Berkani R, Ray R, Jain VK, et al. Evidence update:GlaxoSmithKline's inactivated quadrivalent influenza vaccines[J]. Expert Rev Vaccines, 2016, 15(2): 201-214. DOI:10.1586/14760584.2016.1113878 |
| [109] |
Su LM, Zhang J, Hou X, et al. Surveillance on the Immune Effectiveness of Quadrivalent and Trivalent Split Influenza Vaccines-Shenzhen City and Changzhou City, China, 2018-2019[J]. China CDC Weekly, 2020, 2(21): 370-375. DOI:10.46234/ccdcw2020.095 |
| [110] |
Zhou SZ, Greene CM, Song Y, et al. Review of the status and challenges associated with increasing influenza vaccination coverage among pregnant women in China[J]. Hum Vaccin Immunother, 2020, 16(3): 602-611. DOI:10.1080/21645515.2019.1664230 |
| [111] |
Munoz FM, Patel SM, Jackson LA, et al. Safety and immunogenicity of three seasonal inactivated influenza vaccines among pregnant women and antibody persistence in their infants[J]. Vaccine, 2020, 38(33): 5355-5363. DOI:10.1016/j.vaccine.2020.05.059 |
| [112] |
Vesikari T, Virta M, Heinonen S, et al. Immunogenicity and safety of a quadrivalent inactivated influenza vaccine in pregnant women:a randomized, observer-blind trial[J]. Hum Vaccin Immunother, 2020, 16(3): 623-629. DOI:10.1080/21645515.2019.1667202 |
| [113] |
Steinhoff MC, Omer SB, Roy E, et al. Influenza immunization in pregnancy-antibody responses in mothers and infants[J]. N Engl J Med, 2010, 362(17): 1644-1646. DOI:10.1056/NEJMc0912599 |
| [114] |
Molgaard ND, Fischer TK, Krause TG, et al. Effectiveness of maternal immunization with trivalent inactivated influenza vaccine in pregnant women and their infants[J]. J Intern Med, 2019, 286(4): 469-480. DOI:10.1111/joim.12947 |
| [115] |
Maltezou HC, Asimakopoulos G, Stavrou S, et al. Effectiveness of quadrivalent influenza vaccine in pregnant women and infants, 2018-2019[J]. Vaccine, 2020, 38(29): 4625-4631. DOI:10.1016/j.vaccine.2020.04.060 |
| [116] |
Omer SB, Clark DR, Madhi SA, et al. Efficacy, duration of protection, birth outcomes, and infant growth associated with influenza vaccination in pregnancy:a pooled analysis of three randomised controlled trials[J]. Lancet Respir Medi, 2020, 8(6): 597-608. DOI:10.1016/s2213-2600(19)30479-5 |
| [117] |
Nunes MC, Madhi SA. Influenza vaccination during pregnancy for prevention of influenza confirmed illness in the infants:A systematic review and Meta-analysis[J]. Hum Vaccin Immunother, 2018, 14(3): 758-766. DOI:10.1080/21645515.2017.1345385 |
| [118] |
Cuningham W, Geard N, Fielding JE, et al. Optimal timing of influenza vaccine during pregnancy:A systematic review and Meta-analysis[J]. Influenza Other Respir Viruses, 2019, 13(5): 438-452. DOI:10.1111/irv.12649 |
| [119] |
Zhong Z, Haltalli M, Holder B, et al. The impact of timing of maternal influenza immunization on infant antibody levels at birth[J]. Clin Exp Immunol, 2019, 195(2): 139-152. DOI:10.1111/cei.13234 |
| [120] |
Fu CX, He Q, Li ZT, et al. Seasonal influenza vaccine effectiveness among children, 2010-2012[J]. Influenza Other Respir Viruses, 2013, 7(6): 1168-1174. DOI:10.1111/irv.12157 |
| [121] |
Neuzil KM, Jackson LA, Nelson J, et al. Immunogenicity and reactogenicity of 1 versus 2 doses of trivalent inactivated influenza vaccine in vaccine-naive 5-8-year-old children[J]. J Infect Dis, 2006, 194(8): 1032-1039. DOI:10.1086/507309 |
| [122] |
Shinjoh M, Sugaya N, Furuichi M, et al. Effectiveness of inactivated influenza vaccine in children by vaccine dose, 2013-18[J]. Vaccine, 2019, 37(30): 4047-4054. DOI:10.1016/j.vaccine.2019.05.090 |
| [123] |
Chua H, Chiu SS, Chan ELY, et al. Effectiveness of partial and full influenza vaccination in children aged < 9 years in Hong Kong, 2011-2019[J]. J Infect Dis, 2019, 220(10): 1568-1576. DOI:10.1093/infdis/jiz361 |
| [124] |
Pepin S, Szymanski H, Rochin Kobashi IA, et al. Safety and immunogenicity of an intramuscular quadrivalent influenza vaccine in children 3 to 8 y of age:A phase Ⅲ randomized controlled study[J]. Hum Vaccin Immunother, 2016, 12(12): 3072-3078. DOI:10.1080/21645515.2016.1212143 |
| [125] |
Chiu SS, Kwan MYW, Feng S, et al. Interim estimate of influenza vaccine effectiveness in hospitalised children, Hong Kong, 2017/18[J]. Euro Surveill, 2018, 23(8): 18-00062. DOI:10.2807/1560-7917.ES.2018.23.8.18-00062 |
| [126] |
Zhang Y, Cao ZD, Costantino V, et al. Influenza illness averted by influenza vaccination among school year children in Beijing, 2013-2016[J]. Influenza Other Respir Viruses, 2018, 12(6): 687-694. DOI:10.1111/irv.12585 |
| [127] |
Wu SS, Pan Y, Zhang XX, et al. Influenza vaccine effectiveness in preventing laboratory-confirmed influenza in outpatient settings:A test-negative case-control study in Beijing, China, 2016/17 season[J]. Vaccine, 2018, 36(38): 5774-5780. DOI:10.1016/j.vaccine.2018.07.077 |
| [128] |
Ghendon YZ, Kaira AN, Elshina GA. The effect of mass influenza immunization in children on the morbidity of the unvaccinated elderly[J]. Epidemiol Infect, 2006, 134(1): 71-78. DOI:10.1017/S0950268805005650 |
| [129] |
Younas M, Royer J, Rac H, et al. Association Between Influenza Vaccination Coverage and Ambulatory Antibiotic Prescription Rates in Children in South Carolina[J]. Open Forum Infect Dis, 2019, 6 Suppl 2: S962. DOI:10.1093/ofid/ofz360.2411 |
| [130] |
Rodriguez L, Blanco-Lobo P, Reilly EC, et al. Comparative Study of the Temperature Sensitive, Cold Adapted and Attenuated Mutations Present in the Master Donor Viruses of the Two Commercial Human Live Attenuated Influenza Vaccines[J]. Viruses, 2019, 11(10): 928. DOI:10.3390/v11100928 |
| [131] |
Hoft DF, Babusis E, Worku S, et al. Live and inactivated influenza vaccines induce similar humoral responses, but only live vaccines induce diverse T-cell responses in young children[J]. Infect Dis, 2011, 204(6): 845-853. DOI:10.1093/infdis/jir436 |
| [132] |
Belshe RB, Mendelman PM, Treanor J, et al. The efficacy of live attenuated, cold-adapted, trivalent, intranasal influenzavirus vaccine in children[J]. N Engl J Med, 1998, 338(20): 1405-1412. DOI:10.1056/NEJM199805143382002 |
| [133] |
Belshe RB, Gruber WC, Mendelman PM, et al. Efficacy of vaccination with live attenuated, cold-adapted, trivalent, intranasal influenza virus vaccine against a variant (A/Sydney) not contained in the vaccine[J]. J Pediatr, 2000, 136(2): 168-175. DOI:10.1016/s0022-3476(00)70097-7 |
| [134] |
Bracco NH, Farhat CK, Tregnaghi MW, et al. Efficacy and safety of 1 and 2 doses of live attenuated influenza vaccine in vaccine-naive children[J]. Pediatr Infect Dis J, 2009, 28(5): 365-371. DOI:10.1097/INF.0b013e31819219b8 |
| [135] |
Vesikari T, Fleming DM, Aristegui JF, et al. Safety, efficacy, and effectiveness of cold-adapted influenza vaccine-trivalent against community-acquired, culture-confirmed influenza in young children attending day care[J]. Pediatrics, 2006, 118(6): 2298-2312. DOI:10.1542/peds.2006-0725 |
| [136] |
Tam JS, Capeding MR, Lum LC, et al. Efficacy and safety of a live attenuated, cold-adapted influenza vaccine, trivalent against culture-confirmed influenza in young children in Asia[J]. Pediatr Infect Dis J, 2007, 26(7): 619-628. DOI:10.1097/INF.0b013e31806166f8 |
| [137] |
Wang S, Zheng Y, Jin X, et al. Efficacy and safety of a live attenuated influenza vaccine in Chinese healthy children aged 3-17 years in one study center of a randomized, double-blind, placebo-controlled phase 3 clinical trial, 2016/17 season[J]. Vaccine, 2020, 38(38): 5979-5986. DOI:10.1016/j.vaccine.2020.07.019 |
| [138] |
Block SL, Heikkinen T, Toback SL, et al. The efficacy of live attenuated influenza vaccine against influenza-associated acute otitis media in children[J]. Pediatr Infect Dis J, 2011, 30(3): 203-207. DOI:10.1097/INF.0b013e3181faac7c |
| [139] |
Duan W, Zhang L, Wu SS, et al. Reduction of influenza A(H3N2)-associated symptoms by influenza vaccination in school aged-children during the 2014-2015 winter season dominated by mismatched H3N2 viruses[J]. Hum Vaccin Immunother, 2019, 15(5): 1031-1034. DOI:10.1080/21645515.2019.1575573 |
| [140] |
Pan Y, Wang QY, Yang P, et al. Influenza vaccination in preventing outbreaks in schools:A long-term ecological overview[J]. Vaccine, 2017, 35(51): 7133-7138. DOI:10.1016/j.vaccine.2017.10.096 |
| [141] |
Zhang L, van der Hoek W, Krafft T, et al. Influenza vaccine effectiveness estimates against influenza A(H3N2) and A(H1N1) pdm09 among children during school-based outbreaks in the 2016-2017 season in Beijing, China[J]. Hum Vaccin Immunother, 2020, 16(4): 816-822. DOI:10.1080/21645515.2019.1677438 |
| [142] |
Kim YM, Kang S, Lim JS, et al. Influenza Vaccine Effectiveness among Elementary School Students in Korea during the 2016-2017 Seasons:a Cross-Sectional Survey[J]. J Korean Med Sci, 2020, 35(5): e45. DOI:10.3346/jkms.2020.35.e45 |
| [143] |
Lau YL, Wong WHS, Hattangdi HSR, et al. Evaluating impact of school outreach vaccination programme in Hong Kong influenza season 2018-2019[J]. Hum Vaccin Immunother, 2020, 16(4): 823-826. DOI:10.1080/21645515.2019.1678357 |
| [144] |
Davis MM, King JC, J r. , Moag L, et al[J]. Pediatrics, 2008, 122(1): e260-265. DOI:10.1542/peds.2007-2963 |
| [145] |
King JC Jr, Beckett D, Snyder J, et al. Direct and indirect impact of influenza vaccination of young children on school absenteeism[J]. Vaccine, 2012, 30(2): 289-293. DOI:10.1016/j.vaccine.2011.10.097 |
| [146] |
Demicheli V, Jefferson T, Di Pietrantonj C, et al. Vaccines for preventing influenza in the elderly[J]. Cochrane Database Syst Rev, 2018, 2: CD004876. DOI:10.1002/14651858.CD004876.pub4 |
| [147] |
Jackson ML, Chung JR, Jackson LA, et al. Influenza Vaccine Effectiveness in the United States during the 2015-2016 Season[J]. N Engl J Med, 2017, 377(6): 534-543. DOI:10.1056/NEJMoa1700153 |
| [148] |
Flannery B, Chung JR, Thaker SN, et al. Interim Estimates of 2016-17 Seasonal Influenza Vaccine Effectiveness-United States, February 2017[J]. MMWR Morb Mortal Wkly Rep, 2017, 66(6): 167-171. DOI:10.15585/mmwr.mm6606a3 |
| [149] |
Flannery B, Chung JR, Belongia EA, et al. Interim Estimates of 2017-18 Seasonal Influenza Vaccine Effectiveness-United States, February 2018[J]. MMWR Morb Mortal Wkly Rep, 2018, 67(6): 180-185. DOI:10.15585/mmwr.mm6706a2 |
| [150] |
Dawood FS, Chung JR, Kim SS, et al. Interim Estimates of 2019-20 Seasonal Influenza Vaccine Effectiveness-United States, February 2020[J]. MMWR Morb Mortal Wkly Rep, 2020, 69(7): 177-82. DOI:10.15585/mmwr.mm6907a1 |
| [151] |
Darvishian M, van den Heuvel ER, Bissielo A, et al. Effectiveness of seasonal influenza vaccination in community-dwelling elderly people:an individual participant data Meta-analysis of test-negative design case-control studies[J]. Lancet Respir Med, 2017, 5(3): 200-211. DOI:10.1016/s2213-2600(17)30043-7 |
| [152] |
Beyer WE, McElhaney J, Smith DJ, et al. Cochrane re-arranged:support for policies to vaccinate elderly people against influenza[J]. Vaccine, 2013, 31(50): 6030-6033. DOI:10.1016/j.vaccine.2013.09.063 |
| [153] |
Rolfes MA, Flannery B, Chung JR, et al. Effects of Influenza Vaccination in the United States During the 2017-2018 Influenza Season[J]. Clin Infect Dis, 2019, 69(11): 1845-1853. DOI:10.1093/cid/ciz075 |
| [154] |
Chung JR, Rolfes MA, Flannery B, et al. Effects of Influenza Vaccination in the United States during the 2018-2019 Influenza Season[J]. Clin Infect Dis, 2020. DOI:10.1093/cid/ciz1244 |
| [155] |
Gross PA, Hermogenes AW, Sacks HS, et al. The efficacy of influenza vaccine in elderly persons[J]. Ann Intern Med, 1995, 123(7): 518-527. DOI:10.7326/0003-4819-123-7-199510010-00008 |
| [156] |
Beyer WE, Nauta JJ, Palache AM, et al. Immunogenicity and safety of inactivated influenza vaccines in primed populations:a systematic literature review and Meta-analysis[J]. Vaccine, 2011, 29(34): 5785-5792. DOI:10.1016/j.vaccine.2011.05.040 |
| [157] |
Govaert TM, Thijs CT, Masurel N, et al. The efficacy of influenza vaccination in elderly individuals[J]. JAMA. DOI:10.1001/jama.1994.03520210045030 |
| [158] |
Praditsuwan R, Assantachai P, Wasi C, et al. The efficacy and effectiveness of influenza vaccination among Thai elderly persons living in the community[J]. J Med Assoc Thai, 2005, 88(2): 256-264. |
| [159] |
Centers for Disease Control and Prevention (CDC). Licensure of a high-dose inactivated influenza vaccine for persons aged >or=65 years (Fluzone High-Dose) and guidance for use-United States, 2010[J]. MMWR Morb Mortal Wkly Rep, 2010, 59(16): 485-486.
|
| [160] |
Couch RB, Winokur P, Brady R, et al. Safety and immunogenicity of a high dosage trivalent influenza vaccine among elderly subjects[J]. Vaccine, 2007, 25(44): 7656-7663. DOI:10.1016/j.vaccine.2007.08.042 |
| [161] |
Falsey AR, Treanor JJ, Tornieporth N, et al. Randomized, double-blind controlled phase 3 trial comparing the immunogenicity of high-dose and standard-dose influenza vaccine in adults 65 years of age and older[J]. J Infect Dis, 2009, 200(2): 172-180. DOI:10.1086/599790 |
| [162] |
Keitel WA, Atmar RL, Cate TR, et al. Safety of high doses of influenza vaccine and effect on antibody responses in elderly persons[J]. Arch Intern Med, 2006, 166(10): 1121-1127. DOI:10.1001/archinte.166.10.1121 |
| [163] |
Wilkinson K, Wei Y, Szwajcer A, et al. Efficacy and safety of high-dose influenza vaccine in elderly adults:A systematic review and Meta-analysis[J]. Vaccine, 2017, 35(21): 2775-2780. DOI:10.1016/j.vaccine.2017.03.092 |
| [164] |
DiazGranados CA, Dunning AJ, Kimmel M, et al. Efficacy of high-dose versus standard-dose influenza vaccine in older adults[J]. N Engl J Med, 2014, 371(7): 635-645. DOI:10.1056/NEJMoa1315727 |
| [165] |
Izurieta HS, Thadani N, Shay DK, et al. Comparative effectiveness of high-dose versus standard-dose influenza vaccines in US residents aged 65 years and older from 2012 to 2013 using Medicare data:a retrospective cohort analysis[J]. Lancet Infect Dis, 2015, 15(3): 293-300. DOI:10.1016/s1473-3099(14)71087-4 |
| [166] |
Shay DK, Chillarige Y, Kelman J, et al. Comparative Effectiveness of High-Dose Versus Standard-Dose Influenza Vaccines Among US Medicare Beneficiaries in Preventing Postinfluenza Deaths During 2012-2013 and 2013-2014[J]. J Infect Dis, 2017, 215(4): 510-517. DOI:10.1093/infdis/jiw641 |
| [167] |
Young-Xu Y, van Aalst R, Mahmud SM, et al. Relative Vaccine Effectiveness of High-Dose Versus Standard-Dose Influenza Vaccines Among Veterans Health Administration Patients[J]. J Infect Dis, 2018, 217(11): 1718-1727. DOI:10.1093/infdis/jiy088 |
| [168] |
Doyle JD, Beacham L, Martin ET, et al. Relative and absolute effectiveness of high-dose and standard-dose influenza vaccine against influenza-related hospitalization among older adults-United States, 2015-2017[J]. Clin Infect Dis, 2020, ciaa160. DOI:10.1093/cid/ciaa160 |
| [169] |
Izurieta HS, Chillarige Y, Kelman J, et al. Relative Effectiveness of Influenza Vaccines Among the United States Elderly, 2018-2019[J]. J Infect Dis, 2020, 222(2): 278-287. DOI:10.1093/infdis/jiaa080 |
| [170] |
黄远东, 赵晓平, 万涛, 等. 慢性阻塞性肺病人群流感疫苗接种的效果观察[J]. 海南医学, 2011, 22(4): 29-31. Huang YD, Zhao XP, Wan T, et al. Effects of influenza vaccination in chronic obstructive pulmonary disease[J]. Hainan Med J, 2011, 22(4): 29-31. DOI:10.3969/j.issn.1003-6350.2011.04.011 |
| [171] |
高忠翠, 李江涛, 展胜. 卡舒宁联合流感疫苗对老年性慢性支气管炎合并急性感染的防治效果[J]. 中国生物制品学杂志, 2011, 24(10): 1214-1216. Gao ZC, Li JT, Zhan S. Preventive and curative effects of Card Shu Ning Combined with Influenza Vaccine on senile chronic bronchitis complicated with acute infection[J]. Chin J Biol, 2011, 24(10): 1214-1216. |
| [172] |
Schwarze J, Openshaw P, Jha A, et al. Influenza burden, prevention, and treatment in asthma-A scoping review by the EAACI Influenza in asthma task force[J]. Allergy, 2018, 73(6): 1151-1181. DOI:10.1111/all.13333 |
| [173] |
Vasileiou E, Sheikh A, Butler C, et al. Effectiveness of Influenza Vaccines in Asthma:A Systematic Review and Meta-Analysis[J]. Clin Infect Dis, 2017, 65(8): 1388-1395. DOI:10.1093/cid/cix524 |
| [174] |
Clar C, Oseni Z, Flowers N, et al. Influenza vaccines for preventing cardiovascular disease[J]. Cochrane Database Syst Rev, 2015(5): CD005050. DOI:10.1002/14651858.CD005050.pub3 |
| [175] |
Sribhutorn A, Phrommintikul A, Wongcharoen W, et al. Influenza vaccination in acute coronary syndromes patients in Thailand:the cost-effectiveness analysis of the prevention for cardiovascular events and pneumonia[J]. J Geriatr Cardiol, 2018, 15(6): 413-421. DOI:10.11909/j.issn.1671-5411.2018.06.008 |
| [176] |
Suh J, Kim B, Yang Y, et al. Cost effectiveness of influenza vaccination in patients with acute coronary syndrome in Korea[J]. Vaccine, 2017, 35(21): 2811-2817. DOI:10.1016/j.vaccine.2017.04.016 |
| [177] |
Modin D, Jørgensen ME, Gislason G, et al. Influenza Vaccine in Heart Failure[J]. Circulation, 2019, 139(5): 575-586. DOI:10.1161/circulationaha.118.036788 |
| [178] |
Goeijenbier M, van Sloten TT, Slobbe L, et al. Benefits of flu vaccination for persons with diabetes mellitus:A review[J]. Vaccine, 2017, 35(38): 5095-5101. DOI:10.1016/j.vaccine.2017.07.095 |
| [179] |
Collins JP, Campbell AP, Openo K, et al. Clinical Features and Outcomes of Immunocompromised Children Hospitalized With Laboratory-Confirmed Influenza in the United States, 2011-2015[J]. J Pediatric Infect Dis Soc, 2019, 8(6): 539-549. DOI:10.1093/jpids/piy101 |
| [180] |
徐莉立, 赵金华, 秦颖, 等. 医务人员流感疫苗接种政策与现状分析[J]. 中华预防医学杂志, 2019, 53(10): 973-977. Xu LL, Zhao JH, Qin Y, et al. Current situation and related policies on the implementation and promotion of influenza vaccination among health care workers[J]. Chin J Prev Med, 2019, 53(10): 973-977. DOI:10.3760/cma.j.issn.0253-9624.2019.10.004 |
| [181] |
Ng AN, Lai CK. Effectiveness of seasonal influenza vaccination in healthcare workers:a systematic review[J]. J Hosp Infect, 2011, 79(4): 279-286. DOI:10.1016/j.jhin.2011.08.004 |
| [182] |
Kliner M, Keenan A, Sinclair D, et al. Influenza vaccination for healthcare workers in the UK:appraisal of systematic reviews and policy options[J]. BMJ Open, 2016, 6(9): e12149. DOI:10.1136/bmjopen-2016-012149 |
| [183] |
Imai C, Toizumi M, Hall L, et al. A systematic review and Meta-analysis of the direct epidemiological and economic effects of seasonal influenza vaccination on healthcare workers[J]. PLoS One, 2018, 13(6): e198685. DOI:10.1371/journal.pone.0198685 |
| [184] |
Al Qahtani AA, Selim M, Hamouda NH, et al. Seasonal influenza vaccine effectiveness among health-care workers in Prince Sultan Military Medical City, Riyadh, KSA, 2018-2019[J]. Human Vaccines Immunother, 2020, 1-5. DOI:10.1080/21645515.2020.1764827 |
| [185] |
Amodio E, Restivo V, Firenze A, et al. Can influenza vaccination coverage among healthcare workers influence the risk of nosocomial influenza-like illness in hospitalized patients?[J]. J Hosp Infect, 2014, 86(3): 182-187. DOI:10.1016/j.jhin.2014.01.005 |
| [186] |
刘民, 刘改芬, 赵伟, 等. 医务人员接种流感疫苗的效果及效益研究[J]. 中国实用护理杂志, 2006, 9(9): 708-711. Liu M, Liu GF, Zhao W, et al. An effect and cost-benefit analysis of influenza vaccine among the healthcare worker[J]. Chin Gen Pract, 2006, 9(9): 708-711. DOI:10.3969/j.issn.1007-9572.2006.09.006 |
| [187] |
吴承菊, 郑修霞, 孙菲, 等. 医务人员接种流感疫苗的效果分析[J]. 中国实用护理杂志, 2008, 24(17): 57-59. Wu CJ, Zheng XX, Sun F, et al. Effect analysis of influenza vaccination among medical staff[J]. Chin J Pract Nurs, 2008, 24(17): 57-59. DOI:10.3760/cma.j.issn.1672-7088.2008.17.029 |
| [188] |
Cate TR, Couch RB, Parker D, et al. Reactogenicity, immunogenicity, and antibody persistence in adults given inactivated influenza virus vaccines-1978[J]. Rev Infect Dis, 1983, 5(4): 737-747. DOI:10.1093/clinids/5.4.737 |
| [189] |
Ochiai H, Shibata M, Kamimura K, et al. Evaluation of the efficacy of split-product trivalent A(H1N1), A(H3N2), and B influenza vaccines:reactogenicity, immunogenicity and persistence of antibodies following two doses of vaccines[J]. Microbiol Immunol, 1986, 30(11): 1141-1149. DOI:10.1111/j.1348-0421.1986.tb03043.x |
| [190] |
Kunzel W, Glathe H, Engelmann H, et al. Kinetics of humoral antibody response to trivalent inactivated split influenza vaccine in subjects previously vaccinated or vaccinated for the first time[J]. Vaccine, 1996, 14(12): 1108-1110. DOI:10.1016/0264-410x(96)00061-8 |
| [191] |
Song JY, Cheong HJ, Hwang IS, et al. Long-term immunogenicity of influenza vaccine among the elderly:Risk factors for poor immune response and persistence[J]. Vaccine, 2010, 28(23): 3929-3935. DOI:10.1016/j.vaccine.2010.03.067 |
| [192] |
Feng S, Chiu SS, Chan ELY, et al. Effectiveness of influenza vaccination on influenza-associated hospitalizations over time among children in Hong Kong:a test-negative case-control study[J]. Lancet Respir Med, 2018, 6(12): 925-934. DOI:10.1016/s2213-2600(18)30419-3 |
| [193] |
Ramsay LC, Buchan SA, Stirling RG, et al. The impact of repeated vaccination on influenza vaccine effectiveness:a systematic review and Meta-analysis[J]. BMC Med, 2019, 17(1): 9. DOI:10.1186/s12916-018-1239-8 |
| [194] |
de Lusignan S, Dos Santos G, Byford R, et al. Enhanced Safety Surveillance of Seasonal Quadrivalent Influenza Vaccines in English Primary Care:Interim Analysis[J]. Adv Ther, 2018, 35(8): 1199-1214. DOI:10.1007/s12325-018-0747-4 |
| [195] |
Greenberg DP, Robertson CA, Landolfi VA, et al. Safety and immunogenicity of an inactivated quadrivalent influenza vaccine in children 6 months through 8 years of age[J]. Pediatr Infect Dis J, 2014, 33(6): 630-636. DOI:10.1097/INF.0000000000000254 |
| [196] |
Tsurudome Y, Kimachi K, Okada Y, et al. Immunogenicity and safety of an inactivated quadrivalent influenza vaccine in healthy adults:a phase Ⅱ, open-label, uncontrolled trial in Japan[J]. Microbiol Immunol, 2015, 59(10): 597-604. DOI:10.1111/1348-0421.12316 |
| [197] |
Tinoco JC, Pavia-Ruz N, Cruz-Valdez A, et al. Immunogenicity, reactogenicity, and safety of inactivated quadrivalent influenza vaccine candidate versus inactivated trivalent influenza vaccine in healthy adults aged ≥ 18 years:a phase Ⅲ, randomized trial[J]. Vaccine, 2014, 32(13): 1480-1487. DOI:10.1016/j.vaccine.2014.01.022 |
| [198] |
Statler VA, Albano FR, Airey J, et al. Immunogenicity and safety of a quadrivalent inactivated influenza vaccine in children 6-59 months of age:A phase 3, randomized, noninferiority study[J]. Vaccine, 2019, 37(2): 343-351. DOI:10.1016/j.vaccine.2018.07.036 |
| [199] |
van de Witte S, Nauta J, Montomoli E, et al. A Phase Ⅲ randomised trial of the immunogenicity and safety of quadrivalent versus trivalent inactivated subunit influenza vaccine in adult and elderly subjects, assessing both anti-haemagglutinin and virus neutralisation antibody responses[J]. Vaccine, 2018, 36(40): 6030-6038. DOI:10.1016/j.vaccine.2018.04.043 |
| [200] |
Haber P, Moro PL, Lewis P, et al. Post-licensure surveillance of quadrivalent inactivated influenza (IIV4) vaccine in the United States, Vaccine Adverse Event Reporting System (VAERS), July 1, 2013-May 31, 2015[J]. Vaccine, 2016, 34(22): 2507-2512. DOI:10.1016/j.vaccine.2016.03.048 |
| [201] |
胡昱, 李倩, 陈雅萍, 等. 18岁以上人群接种四价流感病毒灭活疫苗免疫原性和安全性的Meta分析[J]. 国际流行病学传染病学杂志, 2017, 44(1): 47-52. Hu Y, Li Q, Chen YP, et al. Meta-analysis on immunogenicity and safety of inactivated quadrivalent influenza vaccine in adults aged above 18 years[J]. Inter J Epidemiol Infect Dis, 2017, 44(1): 47-52. DOI:10.3760/cma.j.issn.1673-4149.2017.01.010 |
| [202] |
Gandhi-Banga S, Chabanon A L, Eymin C, et al. Enhanced passive safety surveillance of three marketed influenza vaccines in the UK and the Republic of Ireland during the 2017/18 season[J]. Hum Vaccin Immunother, 2019, 15(9): 2154-2158. DOI:10.1080/21645515.2019.1581538 |
| [203] |
Pepin S, Dupuy M, Borja-Tabora CFC, et al. Efficacy, immunogenicity, and safety of a quadrivalent inactivated influenza vaccine in children aged 6-35months:A multi-season randomised placebo-controlled trial in the Northern and Southern Hemispheres[J]. Vaccine, 2019, 37(13): 1876-1884. DOI:10.1016/j.vaccine.2018.11.074 |
| [204] |
Gandhi-Banga S, Chabanon AL, Eymin C, et al. Enhanced passive safety surveillance of three marketed influenza vaccines in the UK and the Republic of Ireland during the 2017/18 season[J]. Hum Vaccin Immunother, 2019, 15(9): 2154-2158. DOI:10.1080/21645515.2019.1581538 |
| [205] |
张佩如, 祝小平, 周良君, 等. 国产流行性感冒病毒裂解疫苗安全性及免疫效果观察[J]. 中华预防医学杂志, 2009, 43(7): 615-618. Zhang PR, Zhu XP, Zhou LJ, et al. Safety and immunological effect of domestic split influenza virus vaccine[J]. Chin J Prev Med, 2009, 43(7): 615-618. DOI:10.3760/cma.j.issn.0253-9624.2009.07.019 |
| [206] |
孙立娜, 李丽芳, 刘静芹, 等. 国产与进口流感疫苗接种的临床观察[J]. 中国免疫学杂志, 2014, 30(1): 77-79. Sun LN, Li LF, Liu JQ, et al. Clinical observation of domestic and imported influenza vaccination[J]. Chin J Immunol, 2014, 30(1): 77-79. DOI:10.3969/j.issn.1000-484X.2014.01.015 |
| [207] |
胡锦流, 王仪, 范刚, 等. 流行性感冒裂解疫苗临床安全性及免疫原性研究[J]. 现代预防医学, 2006, 33(5): 828-829. Hu JL, Wang Y, Fan G, et al. Study on clinical safety and immunogenicity of influenza lysing vaccine[J]. Mod Prev Med, 2006, 33(5): 828-829. DOI:10.3969/j.issn.1003-8507.2006.05.077 |
| [208] |
武文娣, 李克莉, 许涤沙, 等. 中国2015-2018年3个流感季节流感疫苗疑似预防接种异常反应监测数据分析[J]. 中华预防医学杂志, 2019, 53(10): 987-992. Wu WD, Li KL, Xu DS, et al. Study on surveillance data of adverse events following immunization of seasonal influenza vaccine in China during 2015-2018 influenza season Data analysis of monitoring abnormal response of influenza vaccines in China from 2015 to 2018[J]. Chin J Prev Med, 2019, 53(10): 987-992. DOI:10.3760/cma.j.issn.0253-9624.2019.10.007 |
| [209] |
Block SL, Yogev R, Hayden FG, et al. Shedding and immunogenicity of live attenuated influenza vaccine virus in subjects 5-49 years of age[J]. Vaccine, 2008, 26(38): 4940-4946. DOI:10.1016/j.vaccine.2008.07.013 |
| [210] |
Mallory RM, Yi T, Ambrose CS. Shedding of Ann Arbor strain live attenuated influenza vaccine virus in children 6-59 months of age[J]. Vaccine, 2011, 29(26): 4322-4327. DOI:10.1016/j.vaccine.2011.04.022 |
| [211] |
Vesikari T, Karvonen A, Korhonen T, et al. A randomized, double-blind study of the safety, transmissibility and phenotypic and genotypic stability of cold-adapted influenza virus vaccine[J]. Pediatr Infect Dis J, 2006, 25(7): 590-595. DOI:10.1097/01.inf.0000220229.51531.47 |
| [212] |
Vesikari T, Fleming DM, Aristegui JF, et al. Safety, efficacy, and effectiveness of cold-adapted influenza vaccine-trivalent against community-acquired, culture-confirmed influenza in young children attending day care[J]. Pediatrics, 2006, 118(6): 2298-2312. DOI:10.1542/peds.2006-0725 |
| [213] |
Bergen R, Black S, Shinefield H, et al. Safety of cold-adapted live attenuated influenza vaccine in a large cohort of children and adolescents[J]. Pediatr Infect Dis J, 2004, 23(2): 138-144. DOI:10.1097/01.inf.0000109392.96411.4f |
| [214] |
Redding G, Walker RE, Hessel C, et al. Safety and tolerability of cold-adapted influenza virus vaccine in children and adolescents with asthma[J]. Pediatr Infect Dis J, 2002, 21(1): 44-48. DOI:10.1097/00006454-200201000-00010 |
| [215] |
Piedra PA, Yan L, Kotloff K, et al. Safety of the trivalent, cold-adapted influenza vaccine in preschool-aged children[J]. Pediatrics, 2002, 110(4): 662-672. DOI:10.1542/peds.110.4.662 |
| [216] |
Belshe RB, Ambrose CS, Yi T. Safety and efficacy of live attenuated influenza vaccine in children 2-7 years of age[J]. Vaccine, 2008, 26 Suppl 4: D10-16. DOI:10.1016/j.vaccine.2008.06.083 |
| [217] |
Peasah SK, Azziz-Baumgartner E, Breese J, et al. Influenza cost and cost-effectiveness studies globally-a review[J]. Vaccine, 2013, 31(46): 5339-5348. DOI:10.1016/j.vaccine.2013.09.013 |
| [218] |
Ting EE, Sander B, Ungar WJ. Systematic review of the cost-effectiveness of influenza immunization programs[J]. Vaccine, 2017, 35(15): 1828-1843. DOI:10.1016/j.vaccine.2017.02.044 |
| [219] |
Yang J, Atkins KE, Feng LZ, et al. Cost-effectiveness of introducing national seasonal influenza vaccination for adults aged 60 years and above in mainland China:a modelling analysis[J]. BMC Medicine, 2020, 18(1). DOI:10.1186/s12916-020-01545-6 |
| [220] |
Shim E, Brown ST, DePasse J, et al. Cost Effectiveness of Influenza Vaccine for U.S. Children:Live Attenuated and Inactivated Influenza Vaccine[J]. Am J Prev Med, 2016, 51(3): 309-317. DOI:10.1016/j.amepre.2016.02.027 |
| [221] |
Gerlier L, Lamotte M, Grenèche S, et al. Assessment of Public Health and Economic Impact of Intranasal Live-Attenuated Influenza Vaccination of Children in France Using a Dynamic Transmission Model[J]. Appl Health Econ Health Policy, 2017, 15(2): 261-276. DOI:10.1007/s40258-016-0296-4 |
| [222] |
Frenck RW, J r. Randomized, controlled trial of a 13-valent pneumococcal conjugate vaccine administered concomitantly with an influenza vaccine in healthy adults[J]. Clin Vaccine Immunol, 2012, 19(8): 1296-1303. DOI:10.1128/cvi.00176-12 |
| [223] |
Schwarz TF, Flamaing J, Rümke HC, et al. A randomized, double-blind trial to evaluate immunogenicity and safety of 13-valent pneumococcal conjugate vaccine given concomitantly with trivalent influenza vaccine in adults aged ≥ 65 years[J]. Vaccine, 2011, 29(32): 5195-5202. DOI:10.1016/j.vaccine.2011.05.031 |
| [224] |
McNeil SA, Noya F, Dionne M, et al. Comparison of the safety and immunogenicity of concomitant and sequential administration of an adult formulation tetanus and diphtheria toxoids adsorbed combined with acellular pertussis (Tdap) vaccine and trivalent inactivated influenza vaccine in adults[J]. Vaccine, 2007, 25(17): 3464-3474. DOI:10.1016/j.vaccine.2006.12.047 |
| [225] |
Kerzner B, Murray AV, Cheng E, et al. Safety and immunogenicity profile of the concomitant administration of ZOSTAVAX and inactivated influenza vaccine in adults aged 50 and older[J]. J Am Geriatr Soc, 2007, 55(10): 1499-1507. DOI:10.1111/j.1532-5415.2007.01397.x |
| [226] |
Levin MJ, Buchwald UK, Gardner J, et al. Immunogenicity and safety of zoster vaccine live administered with quadrivalent influenza virus vaccine[J]. Vaccine, 2018, 36(1): 179-185. DOI:10.1016/j.vaccine.2017.08.029 |
| [227] |
Nakashima K, Aoshima M, Ohfuji S, et al. Immunogenicity of simultaneous versus sequential administration of a 23-valent pneumococcal polysaccharide vaccine and a quadrivalent influenza vaccine in older individuals:A randomized, open-label, non-inferiority trial[J]. Hum Vaccin Immunother, 2018, 14(8): 1923-1930. DOI:10.1080/21645515.2018.1455476 |
| [228] |
Song JY, Cheong HJ, Tsai TF, et al. Immunogenicity and safety of concomitant MF59-adjuvanted influenza vaccine and 23-valent pneumococcal polysaccharide vaccine administration in older adults[J]. Vaccine, 2015, 33(36): 4647-4652. DOI:10.1016/j.vaccine.2015.05.003 |
| [229] |
Stockwell MS, Broder K, LaRussa P, et al. Risk of fever after pediatric trivalent inactivated influenza vaccine and 13-valent pneumococcal conjugate vaccine[J]. JAMA Pediatr, 2014, 168(3): 211-219. DOI:10.1001/jamapediatrics.2013.4469 |
| [230] |
Duffy J, Weintraub E, Hambidge SJ, et al. Febrile Seizure Risk After Vaccination in Children 6 to 23 Months[J]. Pediatrics, 2016, 138(1): e20160320. DOI:10.1542/peds.2016-0320 |
| [231] |
Li R, Stewart B, McNeil MM, et al. Post licensure surveillance of influenza vaccines in the Vaccine Safety Datalink in the 2013-2014 and 2014-2015 seasons[J]. Pharmacoepidemiol Drug Saf, 2016, 25(8): 928-934. DOI:10.1002/pds.3996 |
| [232] |
Patterson JL, Carapetian SA, Hageman JR, et al. Febrile seizures[J]. Pediatr Ann, 2013, 42(12): 249-254. DOI:10.3928/00904481-20131122-09 |
| [233] |
Nolan T, Bernstein DI, Block SL, et al. Safety and immunogenicity of concurrent administration of live attenuated influenza vaccine with measles-mumps-rubella and varicella vaccines to infants 12 to 15 months of age[J]. Pediatrics, 2008, 121(3): 508-516. DOI:10.1542/peds.2007-1064 |
| [234] |
Lum LC, Borja-Tabora CF, Breiman RF, et al. Influenza vaccine concurrently administered with a combination measles, mumps, and rubella vaccine to young children[J]. Vaccine, 2010, 28(6): 1566-1574. DOI:10.1016/j.vaccine.2009.11.054 |
| [235] |
Grohskopf LA, Alyanak E, Broder KR, et al. Prevention and Control of Seasonal Influenza with Vaccines:Recommendations of the Advisory Committee on Immunization Practices-United States, 2020-21 Influenza Season[J]. MMWR Recomm Rep, 2020, 69(8): 1-24. DOI:10.15585/mmwr.rr6908a1 |
| [236] |
Grohskopf LA, Alyanak E, Broder KR, et al. Prevention and Control of Seasonal Influenza with Vaccines:Recommendations of the Advisory Committee on Immunization Practices-United States, 2019-20 Influenza Season[J]. MMWR Recomm Rep, 2019, 68(3): 1-21. DOI:10.15585/mmwr.rr6803a1 |
| [237] |
Vaccines against influenza WHO position paper-November 2012[J]. Wkly Epidemiol Rec, 2012.87(47): 461-476.
|
| [238] |
Ezeanolue E, Harriman K, Hunter P, et al. General Best Practice Guidelines for Immunization[EB/OL].(2017-04-20)[2020-08-15]. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/.
|
| [239] |
庄文佳, 丛莉, 蔡兴雁, 等. 五种国内常用流感疫苗的分析比较[J]. 中外健康文摘, 2012, 09(27): 71-74. Zhuang WJ, Cong L, Cai XY, et al. Analysis and comparison of five common influenza vaccines in China[J]. World Health Digest, 2012, 09(27): 71-74. DOI:10.3969/j.issn.1672-5085.2012.27.055 |
| [240] |
Des Roches A, Paradis L, Gagnon R, et al. Egg-allergic patients can be safely vaccinated against influenza[J]. J Allergy Clin Immunol, 2012, 130(5): 1213-1216. DOI:10.1016/j.jaci.2012.07.046 |
| [241] |
Des Roches A, Samaan K, Graham F, et al. Safe vaccination of patients with egg allergy by using live attenuated influenza vaccine[J]. J Allergy Clin Immunol Pract, 2015, 3(1): 138-139. DOI:10.1016/j.jaip.2014.08.008 |
| [242] |
Turner PJ, Southern J, Andrews NJ, et al. Safety of live attenuated influenza vaccine in atopic children with egg allergy[J]. J Allergy Clin Immunol, 2015, 136(2): 376-381. DOI:10.1016/j.jaci.2014.12.1925 |
| [243] |
Turner PJ, Southern J, Andrews NJ, et al. Safety of live attenuated influenza vaccine in young people with egg allergy:multicentre prospective cohort study[J]. BMJ, 2015, 351: h6291. DOI:10.1136/bmj.h6291 |
| [244] |
Grohskopf LA, Sokolow LZ, Broder KR, et al. Prevention and Control of Seasonal Influenza with Vaccines:Recommendations of the Advisory Committee on Immunization Practices-United States, 2018-19 Influenza Season[J]. MMWR Recomm Rep, 2018, 67(3): 1-20. DOI:10.15585/mmwr.rr6703a1 |
| [245] |
Chiavenna C, Presanis AM, Charlett A, et al. Estimating age-stratified influenza-associated invasive pneumococcal disease in England:A time-series model based on population surveillance data[J]. PLoS Med, 2019, 16(6): e1002829. DOI:10.1371/journal.pmed.1002829 |
| [246] |
Ofori-Anyinam O, Leroux-Roels G, Drame M, et al. Immunogenicity and safety of an inactivated quadrivalent influenza vaccine co-administered with a 23-valent pneumococcal polysaccharide vaccine versus separate administration, in adults ≥ 50 years of age:Results from a phase Ⅲ, randomized, non-inferiority trial[J]. Vaccine, 2017, 35(46): 6321-6328. DOI:10.1016/j.vaccine.2017.09.012 |
| [247] |
Chang YC, Chou YJ, Liu JY, et al. Additive benefits of pneumococcal and influenza vaccines among elderly persons aged 75 years or older in Taiwan-a representative population-based comparative study[J]. J Infect, 2012, 65(3): 231-238. DOI:10.1016/j.jinf.2012.04.014 |
| [248] |
Christenson B, Pauksen K, Sylvan SP. Effect of influenza and pneumococcal vaccines in elderly persons in years of low influenza activity[J]. Virol J, 2008, 5: 52. DOI:10.1186/1743-422X-5-52 |
| [249] |
Yin M, Huang L, Zhang Y, et al. Effectiveness and safety of dual influenza and pneumococcal vaccination versus separate administration or no vaccination in older adults:a Meta-analysis[J]. Expert Rev Vaccines, 2018, 17(7): 653-663. DOI:10.1080/14760584.2018.1495077 |
| [250] |
Poscia A, Collamati A, Carfi A, et al. Influenza and pneumococcal vaccination in older adults living in nursing home:a survival analysis on the shelter study[J]. Eur J Public Health, 2017, 27(6): 1016-1020. DOI:10.1093/eurpub/ckx150 |
| [251] |
Li C, Gubbins PO, Chen GJ. Prior pneumococcal and influenza vaccinations and in-hospital outcomes for community-acquired pneumonia in elderly veterans[J]. J Hosp Med, 2015, 10(5): 287-293. DOI:10.1002/jhm.2328 |
| [252] |
Farkas K, Terhes G, Deak J, et al. The efficiency of influenza vaccines in patients with inflammatory bowel disease on immunosuppressive therapy[J]. Orv Hetil, 2012, 153(47): 1870-1874. DOI:10.1556/OH.2012.29484 |
| [253] |
Huemer HP. Possible immunosuppressive effects of drug exposure and environmental and nutritional effects on infection and vaccination[J]. Mediators Inflamm, 2015, 2015: 349176. DOI:10.1155/2015/349176 |
 2020, Vol. 41
2020, Vol. 41