文章信息
- 陈卫永, 马瞧勤, 潘晓红, 周欣, 陈婉君, 陈琳, 姜婷婷, 王憓.
- Chen Weiyong, Ma Qiaoqin, Pan Xiaohong, Zhou Xin, Chen Wanjun, Chen Lin, Jiang Tingting, Wang Hui
- 浙江省艾滋病综合防治示范区低档暗娼肛交行为调查
- Situation of anal sex among low-tier female sex workers in the Demonstration Areas of Comprehensive AIDS Responses in Zhejiang province
- 中华流行病学杂志, 2020, 41(7): 1081-1085
- Chinese Journal of Epidemiology, 2020, 41(7): 1081-1085
- http://dx.doi.org/10.3760/cma.j.cn112338-20190731-00567
-
文章历史
收稿日期: 2019-07-31
在所有性行为中,肛交较阴道交、口交更容易感染HIV/STD,MSM肛交是其感染HIV的主要途径[1-3]。但是,异性的肛交行为报道较少。全世界约有10%的女性有肛交行为[4-8]。国外有报道,女性与异性性伴发生肛交,即使其性伴是抗病毒治疗的HIV感染者,也比发生阴道交的HIV感染风险高8倍[4, 9-11]。2013年浙江省在11个城市的22个县(区)建立艾滋病综合防治示范区,其中21个县(区)开展低档暗娼的调查研究。为了解低档暗娼发生肛交情况及其HIV感染风险,本研究分析浙江省艾滋病综合防治示范区的低档暗娼与嫖客发生肛交的相关情况及影响因素,为做好该人群的行为干预提供参考依据。
对象与方法1.调查现场:2013年9-11月浙江省21个艾滋病综合防治示范区。
2.调查对象:纳入标准:①从事商业性交易的暗娼;②来自规模较小的性交易场所(暗娼人数≤8人,如发廊/按摩店、路边店或站街);③年龄≥18岁。本研究通过浙江省CDC伦理委员会审批(2012ZX10001001-011)。
3.调查方法:采用横断面调查方法。制定调查计划前,先摸底调查,确定当地低档暗娼的活动场所和规模,暗娼人数规模估计为3 100人,由于低档暗娼流动性较大,应答率约为80%,估计调查对象样本量为2 480人。调查人员为经过培训的当地CDC专业人员。采用面对面访谈式问卷调查,调查场所设立相对独立空间,以保护调查对象隐私。选择2个县(区)开展预调查,完成调查对象招募、现场组织和调查流程、测试和完善调查问卷。调查问卷收集社会人口学特征、艾滋病性病知识、阴道交/口交/肛交性行为、STD患病、艾滋病性病危险认知等。问卷的信度测量,Cronbach’s α系数为0.932(参考值范围0.800~0.900),说明问卷的信度较好。
4.相关定义:肛交定义来自暗娼自我报告最近1个月与嫖客发生肛交行为。安全套使用自我效能包括3个问题:嫖客拒绝使用安全套时能否拒绝发生性行为、嫖客拒绝使用安全套时能否说服嫖客使用安全套、与嫖客发生性行为时能否每次坚持使用安全套,得分最高3分,最低0分。
5.统计学分析[12-13]:采用SPSS 17.0软件进行统计学分析。描述采用频数分布和构成比。采用logistic回归模型分析最近1个月与嫖客发生肛交的相关影响因素,单因素分析的自变量筛选标准为0.05,再进行多因素logistic回归分析。双侧检验,以P<0.05为差异有统计学意义。
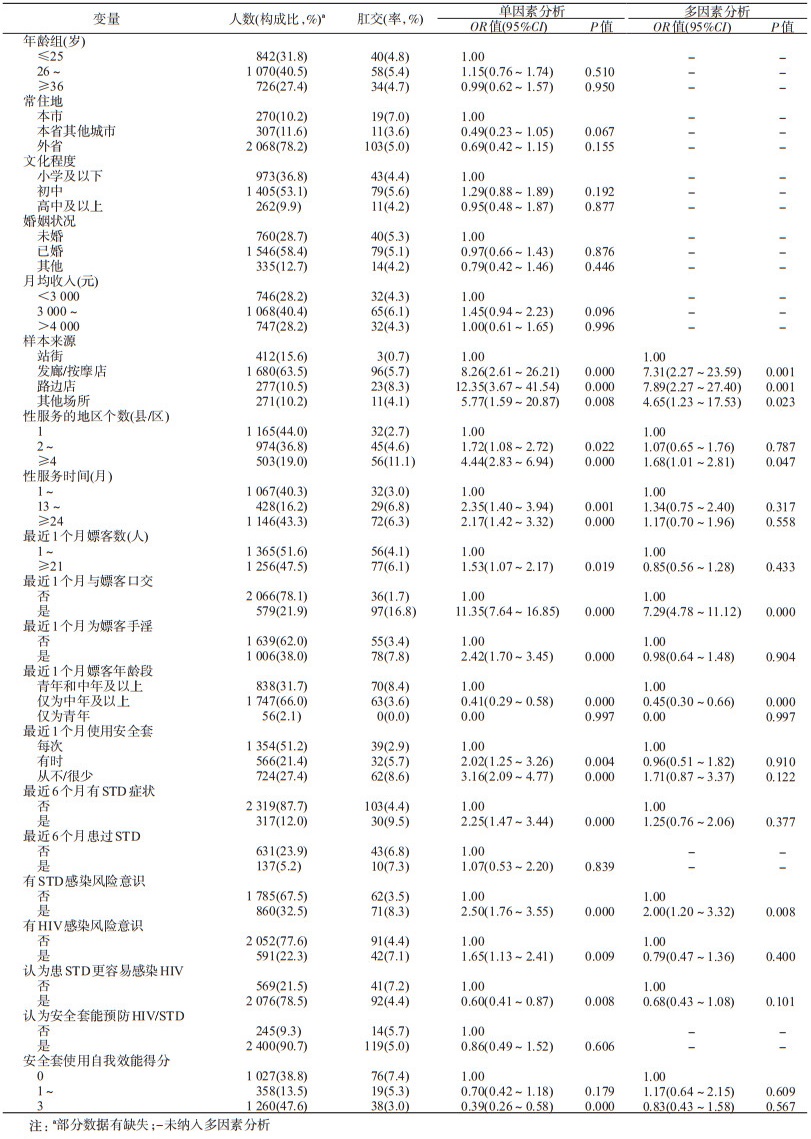
结果1.基本情况:共招募低档暗娼2 648人,调查对象2 645人,≥26岁占67.9%(1 796/2 645)、初中及以下文化程度占89.9%(2 378/2 645)、已婚占58.4%(1 546/2 645)、外省籍占78.2%(2 068/2 645)、月均收入≤4 000元的占68.6%(1 814/2 645)。见表 1。
2.最近1个月与嫖客肛交情况:低档暗娼最近1个月与嫖客肛交发生率为5.03%(133/2 645)。其中,仅发生肛交的有12人,口交、阴道交和肛交均发生的有95人,阴道交和肛交均发生的有24人,口交和肛交发生的有2人。
3.最近1个月与嫖客肛交的相关因素:单因素logistic回归分析结果显示,低档暗娼的年龄、常住地、文化程度、婚姻状况、月均收入、认为安全套能预防HIV/STD、最近6个月患过STD等自变量,无统计学意义。
多因素logistic回归分析结果显示,低档暗娼最近1个月与嫖客发生肛交的影响因素包括:性服务类型为发廊/按摩店、路边店和其他场所服务,分别是站街服务的7.31倍(95%CI:2.27~23.59)、7.89倍(95CI:2.27~27.40)和4.65倍(95%CI:1.23~17.53);性服务地区数量≥4个县(区)是性服务仅固定在1个县(区)的1.68倍(95%CI:1.01~2.81);最近1个月嫖客年龄段仅为中年及以上是青年和中年及以上嫖客的0.45倍(95%CI:0.30~0.66);有STD感染风险意识者是无STD感染风险意识者的2.00倍(95%CI:1.20~3.32);最近1个月与嫖客发生口交者是与未发生口交者的7.29倍(95%CI:4.78~11.12)。见表 1。
讨论本研究发现,最近1个月与嫖客肛交发生率为5.03%,明显低于国外报道的暗娼与嫖客的肛交发生率[14-15]。在所有类别的暗娼中,站街服务暗娼与嫖客肛交发生率为0.7%,而发廊/按摩店、路边店和其他场所服务的暗娼与嫖客肛交发生率分别为5.7%、8.3%和4.1%,明显高于站街服务暗娼,推测可能与站街服务暗娼招揽嫖客时往往没有固定的场所,嫖客多为追求性满足而非不同性行为方式带来的刺激与快感等有关。有研究发现,肛交接受方的HIV感染风险是1.7%,阴道交则是0.7%[3];如果女性的8次异性性行为中发生2次肛交,其HIV感染风险增加9倍[16];而且,肛交的安全套使用率低于阴道交的安全套使用率[10, 17]。另外,我国暗娼人群STD患病率很高[18]。因此,低档暗娼的高危行为干预中,应关注肛交行为的HIV/STD传播风险。
本研究发现,低档暗娼以年龄≥26岁、初中及以下文化程度、已婚、外省籍、月均收入≤4 000元为主。这与其他的研究结果一致[19-21]。尽管上述社会人口学特征不是最近1个月低档暗娼与嫖客发生肛交的影响因素,但是,低档暗娼的这些社会人口学特征可能会妨碍其正常获得HIV/STD预防信息或服务。国外报道,男性通过肛交向女性传播HIV的风险非常高[4, 22];肛交接受方也是STD、HBV及HPV感染的危险因素[10-11, 23-26]。本研究发现,低档暗娼发生肛交的伴有阴道交和/或口交占91.0%,而3种性行为均可能传播HIV/STD;这些暗娼可能为了获得更多的金钱而顺从嫖客的需求发生多种性行为,但坚持每次使用安全套比例仅为29.3%,因此,该类暗娼是HIV/STD传播的核心人群。针对他们的干预活动必须强调肛交的危险性以及在3种商业性性行为中坚持每次使用安全套。
有文献显示,肛交发生与较低的安全套使用率有关联[15, 27]。本研究发现,那些有肛交行为者可能意识到了肛交的危险性,可能有更高的风险意识。但是,暗娼在发生肛交的安全套使用率并没有增加,需要加强安全性行为的健康教育。国外有报道,女性性工作者发生肛交有更高的STD感染水平[14, 17]。本研究单因素分析显示最近半年有STD症状的低档暗娼最近1个月与嫖客更容易发生肛交,但在多因素分析中这种影响不再存在。为获得更多的嫖客数量和性交易收入,低档暗娼提供口交时也会提供肛交,不同县(区)和/或不同年龄的嫖客接受这种性服务。虽然她们能够意识到这种性行为相比于阴道交,感染STD的风险更高,但她们的安全套使用率并没有相应提高,需重点关注低档暗娼肛交的危险行为干预。去过医院寻求STD诊治无论是否诊断为STD,也与最近1个月肛交发生没有影响。这可能是因为调查对象报告STD症状时漏报直肠及肛周疾患,或者临床医生也没有关注到。建议临床医生为暗娼人群的外阴及生殖器体检时,增加直肠/肛门检查。
本研究发现,年龄、常住地、文化程度、婚姻状况、月均收入等人口学特征、性服务时间长短、最近1个月嫖客数与最近1个月低档暗娼发生肛交之间关联无统计学意义,推测低档暗娼发生肛交更多是满足嫖客的要求。但是,最近1个月低档暗娼发生肛交的影响因素包括性服务场所、性服务地区数量、嫖客年龄、STD感染风险意识、与嫖客发生口交。
本研究存在不足。仅调查低档暗娼最近1个月性行为,且肛交为我国传统性文化所忌讳,实际发生存在报告偏倚;STD患病史存在回忆偏倚;现场调查阶段低档暗娼可能约有20.0%不在现场;横断面调查问卷设计限制,无法准确收集发生肛交/阴道交/口交的安全套使用情况。
综上所述,浙江省艾滋病综合防治示范区的低档暗娼与嫖客的商业性行为存在肛交现象,发生口交的低档暗娼更容易发生肛交。应重点关注低档暗娼的肛交及危险行为干预。
利益冲突 所有作者均声明不存在利益冲突
| [1] |
Nguyen TA, Nguyen HT, Le GT, et al. Prevalence and risk factors associated with HIV infection among men having sex with men in Ho Chi Minh City, Vietnam[J]. AIDS Behav, 2008, 12(3): 476-482. DOI:10.1007/s10461-007-9267-y |
| [2] |
宋丹丹, 张洪波, 王君, 等. 广州和成都市男男性行为兼异性性行为者的HIV感染状况及性行为特征[J]. 中华流行病学杂志, 2012, 33(4): 368-373. Song DD, Zhang HB, Wang J, et al. The prevalence of HIV infection and sexual behaviors among men who have sex with men and women in Chengdu and Guangzhou, China[J]. Chin J Epidemiol, 2012, 33(4): 368-373. DOI:10.3760/cma.j.issn.0254-6450.2012.04.005 |
| [3] |
Boily MC, Baggaley R, Wang L, et al. Heterosexual risk of HIV-1 infection per sexual act:Systematic review and Meta-analysis of observational studies[J]. Lancet Infect Dis, 2009, 9(2): 118-129. DOI:10.1016/S1473-3099(09)70021-0 |
| [4] |
Baggaley RF, White RG, Boily MC. HIV transmission risk through anal intercourse:systematic review, Meta-analysis and implications for HIV prevention[J]. Int J Epidemiol, 2010, 39(4): 1048-1063. DOI:10.1093/ije/dyq057 |
| [5] |
Health-e News. Anal sex a major driver in HIV epidemic[EB/OL]. (2010-05-26)[2019-07-01]. https: //health-e.org.za/2010/05/26/anal-sex-a-major-driver-in-hiv-epidemic/.
|
| [6] |
Kloos H, Mariam DH. Some neglected and emerging factors in HIV transmission in Ethiopia[J]. Ethiop Med J, 2007, 45(1): 103-107. |
| [7] |
Mosher WD, Chandra A, Jones J. Sexual behavior and selected health measures:men and women 15-44 years of age, United States, 2002[J]. Adv Data, 2005, 362: 1-55. |
| [8] |
Voeller B. AIDS and heterosexual anal intercourse[J]. Arch Sex Behav, 1991, 20(3): 233-276. DOI:10.1007/BF01541846 |
| [9] |
Baldwin JI, Baldwin JD. Heterosexual anal intercourse:an understudied, high-risk sexual behavior[J]. Arch Sex Behav, 2000, 29(4): 357-373. DOI:10.1023/A:1001918504344 |
| [10] |
Halperin DT. Heterosexual anal intercourse:Prevalence, cultural factors, and HIV infection and other health risks, PartⅠ[J]. AIDS, Patient, Care, Stds, 1999, 13(12): 717-730. DOI:10.1089/apc.1999.13.717 |
| [11] |
Misegades L, Page-Shafer K, Halperin D, et al. Anal intercourse among young low-income women in California:An overlooked risk factor for HIV?[J]. AIDS, 2001, 15(4): 534-535. DOI:10.1097/00002030-200103090-00017 |
| [12] |
廖玫珍, 刘冬莹, 朱晓艳, 等. 山东省男男性行为人群单性性行为者与双性性行为者特征及HIV感染相关因素[J]. 中华流行病学杂志, 2019, 40(8): 941-946. Liao MZ, Liu DY, Zhu XY, et al. Behavior and influencing factors of HIV infection among men who have sex with men only and men who have sex with both men and women in Shandong province[J]. Chin J Epidemiol, 2019, 40(8): 941-946. DOI:10.3760/cma.j.issn.0254-6450.2019.08.013 |
| [13] |
贾蕾, 吕冰, 田祎, 等. 北京市2008-2017年细菌性痢疾病原学监测分析[J]. 中华流行病学杂志, 2019, 40(2): 165-169. Jia L, Lyu B, Tian W, et al. Pathogenic surveillance and related factors on bacillary dysentery in Beijing, 2008-2017[J]. Chin J Epidemiol, 2019, 40(2): 165-169. DOI:10.3760/cma.j.issn.0254-6450.2019.02.008 |
| [14] |
Schwandt M, Morris C, Ferguson A, et al. Anal and dry sex in commercial sex work, and relation to risk for sexually transmitted infections and HIV in Meru, Kenya[J]. Sex Transm Infect, 2006, 82(5): 392-396. DOI:10.1136/sti.2006.019794 |
| [15] |
Priddy FH, Wakasiaka S, Hoang TD, et al. Anal sex, vaginal practices, and HIV incidence in female sex workers in urban Kenya:implications for the development of intravaginal HIV prevention methods[J]. AIDS Res Hum Retroviruses, 2011, 27(10): 1067-1072. DOI:10.1089/aid.2010.0362 |
| [16] |
Boily MC, Baggaley RF, Masse B. The role of heterosexual anal intercourse for HIV transmission in developing countries:Are we ready to draw conclusions?[J]. Sex Transm Infect, 2009, 85(6): 408-410. DOI:10.1136/sti.2009.037499 |
| [17] |
Kalichman SC, Simbayi LC, Cain D, et al. Heterosexual anal intercourse among community and clinical settings in Cape Town, South Africa[J]. Sex Transm Infect, 2009, 85(6): 411-415. DOI:10.1136/sti.2008.035287 |
| [18] |
Su S, Chow EPF, Muessig KE, et al. Sustained high prevalence of viral hepatitis and sexually transmissible infections among female sex workers in China:a systematic review and Meta-analysis[J]. BMC Infect Dis, 2016, 16: 2. DOI:10.1186/s12879-015-1322-0 |
| [19] |
Li J, Chen XS, Merli MG, et al. Systematic differences in risk behaviors and syphilis prevalence across types of female sex workers:a preliminary study in Liuzhou, China[J]. Sex Transm Dis, 2012, 39(3): 195-200. DOI:10.1097/OLQ.0b013e31823d2e2a |
| [20] |
付笑冰, 王冰娜, 李艳, 等. 广东省中低档女性性工作者艾滋病病毒/性传播疾病感染状况及危险因素分析[J]. 中华流行病学杂志, 2014, 35(5): 510-513. Fu XB, Wang BN, Li Y, et al. Prevalence of HIV and sexually transmitted diseases as well as related associated risk factors among middle/low level female sex workers in a city in Guangdong Province[J]. Chin J Epidemiol, 2014, 35(5): 510-513. DOI:10.3760/cma.j.issn.0254-6450.2014.05.009 |
| [21] |
孙燕鸣, 李桂英, 卢红艳. 2011-2016年北京市女性性工作者HIV梅毒血清学调查[J]. 中国艾滋病性病, 2019, 25(3): 260-272. Sun YM, Li GY, Lu HY. Characteristics of female sex workers and their HIV and syphilis prevalence in Beijing, 2011-2016[J]. Chin J AIDS STD, 2019, 25(3): 260-272. DOI:10.13419/j.cnki.aids.2019.03.11 |
| [22] |
Leynaert B, Downs AM, de Vincenzi I, et al. Heterosexual transmission of human immunodeficiency virus:variability of infectivity throughout the course of infection[J]. Am J Epidemiol, 1998, 148(1): 88-96. DOI:10.1093/oxfordjournals.aje.a009564 |
| [23] |
Risser JMH, Padgett P, Wolverton M, et al. Relationship between heterosexual anal sex, injection drug use and HIV infection among black men and women[J]. Int J STD AIDS, 2009, 20(5): 310-314. DOI:10.1258/ijsa.2008.008394 |
| [24] |
Diclemente RJ, Wingood GM, Crosby RA, et al. Anal sex is a behavioural marker for laboratory-confirmed vaginal sexually transmissible infections and HIV-associated risk among African-American female adolescents[J]. Sexual Health, 2009, 6(2): 111-116. DOI:10.1071/SH08062 |
| [25] |
Chirgwin KD, Feldman J, Dehovitz JA, et al. Incidence and risk factors for heterosexually acquired HIV in an inner-city cohort of women:temporal association with pregnancy[J]. J Acquir Immune Defic Syndr Hum Retrovirol, 1999, 20(3): 295-299. DOI:10.1097/00042560-199903010-00013 |
| [26] |
Skurnick JH, Kennedy CA, Perez G, et al. Behavioral and demographic risk factors for transmission of human immunodeficiency virus type 1 in heterosexual couples:report from the heterosexual HIV transmission study[J]. Clin Infect Dis, 1998, 26(4): 855-864. DOI:10.1086/513929 |
| [27] |
Somanath RP, Mishra RM, Saggurti N, et al. The association between noncommercial partnerships and risk of HIV among female sex workers:evidences from a cross-sectional behavioral and biological survey in southern India[J]. AIDS Res Treat, 2013, 2013: 108630. DOI:10.1155/2013/108630 |
 2020, Vol. 41
2020, Vol. 41