文章信息
- 徐晓慧, 杨静, 王黎君, 殷鹏, 刘江美, 董文兰, 王薇, 王璇, 秦莉, 周脉耕.
- Xu Xiaohui, Yang Jing, Wang Lijun, Yin Peng, Liu Jiangmei, Dong Wenlan, Wang Wei, Wang Xuan, Qin Li, Zhou Maigeng
- 2017年中国人群高血清低密度脂蛋白胆固醇归因疾病负担研究
- Burden of disease attributed to high level serum low-density lipoprotein cholesterol in China in 2017
- 中华流行病学杂志, 2020, 41(6): 839-844
- Chinese Journal of Epidemiology, 2020, 41(6): 839-844
- http://dx.doi.org/10.3760/cma.j.cn112338-20191205-00861
-
文章历史
收稿日期: 2019-12-05
2. 中国疾病预防控制中心慢性非传染性疾病预防控制中心科教与国际合作室, 北京 100050;
3. 中国疾病预防控制中心慢性非传染性疾病预防控制中心生命登记与死因监测室, 北京 100050;
4. 中国疾病预防控制中心慢性非传染性疾病预防控制中心危险因素监测室, 北京 100050;
5. 中国疾病预防控制中心慢性非传染性疾病预防控制中心肥胖与代谢室, 北京 100050;
6. 中国疾病预防控制中心慢性非传染性疾病预防控制中心, 北京 100050
2. Division of Science, Education and International Cooperation, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing 100050, China;
3. Division of Vital Statistics and Death Surveillance, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing 100050, China;
4. Division of Non-communicable Disease Risk Factor Surveillance, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing 100050, China;
5. Division of Obesity and Metabolic Diseases Control and Prevention, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing 100050, China;
6. National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing 100050, China
血清LDL-C在动脉粥样硬化性心血管疾病(arteriosclerotic cardiovascular disease,ASCVD)发病中起着重要作用[1],是缺血性心脏病(ischemic heart disease,IHD)和缺血性卒中(ischemic stroke,IS)的主要危险因素之一[2-3],卒中和IHD已成为我国主要死因,且死亡人数仍有上升趋势[4]。由于城镇化进程加快及生活方式的改变,我国人群血清LDL-C水平及高LDL-C血症患病率也有升高趋势[5],2013年监测数据显示,我国成年人血清LDL-C加权均值为2.88 mmol/L,高LDL-C血症患病率为8.1%[6],均高于2010年调查结果[7]。在ASCVD高危人群中,有74.5%的人LDL-C未达到控制水平(<2.88 mmol/L),治疗率仅有5.5%[6]。
国内外血脂指南提出,由于TC水平受HDL-C水平影响,LDL-C较TC相比,能够更好地作为ASCVD危险性评估的有效指标[3, 8-10],且LDL-C作为心血管疾病的主要干预靶点对防治心血管疾病有重大意义。2017年全球疾病负担研究(GBD2017)将既往研究中对TC的研究转为LDL-C归因疾病负担的研究,采用统一、可比的方法对全球195个国家和地区归因于LDL-C的疾病负担作出估算,发现高LDL-C是在全球导致死亡的第5位危险因素且上升明显[11],是导致中国人群死亡的第6位危险因素[4]。本研究利用GBD2017数据,对中国及各省份高LDL-C归因死亡及伤残调整寿命年(disability- adjusted life years,DALY)进行描述性分析,为血脂异常防治工作提供参考。
资料与方法1.资料来源:归因死亡及伤残疾病负担数据来自GBD2017。死亡数据主要来自全国疾病监测点系统死因监测、死因登记报告信息系统、全国妇幼卫生监测网、中国香港地区和中国澳门地区的死因数据,以及一些已发表的文献或报告。中国人群血清LDL-C数据来源于人群横断面调查研究、大型队列研究和局部地区的调查数据,包括中国慢性病与危险因素监测(2004、2007、2010、2013年)、2002年中国居民营养与健康状况调查等。通过文献检索和Meta分析,获取与高LDL-C有病因学联系的IHD及IS相对危险度估计值。其他数据来源见文献[11-12]。
2.人群归因分值的估算:采用比较风险评估(comparative risk assessment,CRA)理论[11],假设将人群LDL-C水平降低到理论最小风险暴露的反事实情景,则人群归因分值(population attributable fraction,PAF)表示可减少的疾病负担百分比。CRA基本理论是假定在其他危险因素水平不变时,将目标人群某种危险因素的暴露水平与处于理论最小风险暴露水平(theoretical minimum-risk exposure level,TMREL)分布时的疾病负担相比较,以此来获取人群中最大归因负担[11]。
3. LDL-C暴露水平的估算:通过GBD历年数据进行系统回顾,将血脂相关数据(包括LDL-C、TC、TG和HDL-C)按年龄、性别、地点、年份进行提取和拆分,当无法获得LDL-C水平时,使用血脂的其他成分来估计LDL-C水平。GBD2017采用了更新的时空高斯过程回归(ST-GPR)框架,对LDL-C相关数据按地点、年份、性别年龄组进行建模。LDL-C的TMREL范围为0.7~1.3 mmol/L,本研究高LDL-C特指人群血清LDL-C>TMREL的人群归因疾病负担[11]。
4.归因死亡及归因疾病负担的估算:在本研究中,用归因死亡数及DALY来测量高LDL-C引起的疾病负担,以PAF分别乘以相关疾病死亡数、DALY,计算出归因于高LDL-C的死亡和DALY[11]。不同省份及性别死亡率及DALY率进行比较时通过GBD2017所采用的标准人口进行标化。DALY是早死导致的寿命损失年(YLL)和伤残导致的寿命损失年(YLD)两部分的总和[12],其中YLL=Σ(N×L),N表示某年龄组、某性别由于某种死因造成的死亡人数,L表示该年龄组的寿命损失值,即标准寿命表(来源于可观察到的全球分年龄段的最高期望寿命)中该死亡年龄组所对应的期望寿命值[13];YLD=患病率×伤残权重[14]。DALY率的计算方法为计算出的DALY数与该组人口数之比[12]。因高LDL-C导致的IHD、IS死亡在<25岁是罕见的,因此<25岁归因死亡不作估算。GBD2017按照国际疾病分类第10版(ICD-10),将IHD的编码范围定义为:I20~25.9,IS的编码范围为:G45~G46.8、I63~I63.9、I65~I66.9、I67.2~I67.3、I67.5~I67.6、I69.3[13]。
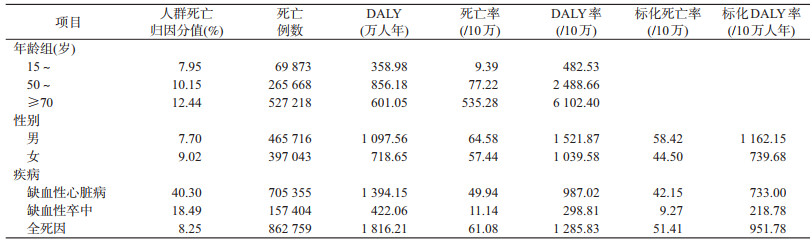
结 果1.整体情况:2017年中国人群全死因死亡中归因于高LDL-C的人数为862 759人,占全死因死亡的8.25%。其中男性归因死亡数为465 716人,女性397 043人,分别占男女性死亡人数的7.70%、9.02%,女性的死亡归因分值高于男性。造成DALY损失1 816.21万人年,其中男性1 097.56万人年,女性718.65万人年,分别占男女性所有疾病DALY损失的5.25%和4.44%。见表 1。
2.不同心血管疾病的归因死亡百分比:2017年中国人群血清高LDL-C造成心血管疾病死亡归因百分比为19.71%,其中造成的IHD、IS死亡人数分别为70.54万和15.74万,占总归因死亡例数的81.76%和18.14%。高LDL-C对IHD和IS归因死亡百分比分别为40.30%和18.49%。见表 1。
3.不同年龄组的归因死亡百分比:人群死亡归因分值、归因死亡人数、归因死亡率及归因DALY率均随着年龄组增大而升高,均在≥70岁人群最高。DALY数在50~69岁年龄组最高,为856.18万人年。见表 1。
4.不同省份的归因死亡百分比:有8个省份人群高LDL-C对总死亡的归因分值超过10%,前4位为吉林省、黑龙江省、天津市和内蒙古自治区;标化归因死亡率和标化DALY率最高的3个省份为:黑龙江省、内蒙古自治区和吉林省。见表 2。
本研究基于GBD2017的数据估算结果,以人群归因分值、归因死亡、归因DALY等量化指标评估了中国人群血清高LDL-C对死亡及伤残负担的归因情况。本研究结果表明,2017年我国归因于高LDL-C的死亡人数占总死亡人数的8.25%,高于全球水平(7.72%),表明我国人群高LDL-C较其他危险因素对全死因死亡的归因分值更高。本研究估算高LDL-C对IHD、IS死亡归因百分比(40.30%、18.49%),较其他研究估算的高TC对IHD、IS死亡归因百分比(19.2%、4.2%)高[15]。据估算,我国有3.3%左右的全死因死亡可归因于血清高TC[15-16],提示高LDL-C比高TC对人群全死因死亡及IHD、IS死亡的归因分值更高,也更加敏感。若扣除人口增长及老龄化因素,归因于高LDL-C的疾病负担仍较高,可能因为TC中含有HDL-C等保护成分,有证据表明HDL-C通过胆固醇逆转运可将外周组织如血管壁的胆固醇转运至肝脏分解代谢或以胆酸的形式排出体外,可能对动脉粥样硬化性心血管疾病发病有保护作用[17-18]。
2017年女性高LDL-C导致全人群死亡的PAF高于男性,表明女性因高LDL-C导致死亡的百分比高于男性,但男性标化死亡率和标化DALY率高于女性,可能由于男性IHD、IS死亡多于女性。≥70岁人群的归因疾病负担最高,表明高LDL-C对老年人群的死亡及伤残影响较大,但也与高年龄组本身死亡规律有关;DALY在50~69岁年龄组最高,为856.18万人年。从省份分布来看,中国东北地区的省份如吉林、黑龙江人群的高LDL-C对全死因死亡的归因分值较高,LDL-C归因死亡率也较高,而南方地区较低,可能与各省份IHD、IS死亡占比不同、血脂异常分布不同有关[4, 19-21]。
我国人群血清LDL-C水平近年来有所上升[6, 22],IHD、IS造成的疾病负担也显著增加[23-24]。LDL-C水平过高是IHD、IS的重要危险因素,控制LDL-C水平对减少IHD、IS的疾病负担尤为重要[3]。然而我国血脂异常患病率高,知晓、治疗、控制率均较低[25-26]。有研究表明,年龄增长、身体活动不足、油脂摄入过高、高BMI、饮酒及红肉摄入过多是血脂升高的相关危险因素[8, 27]。加强健康教育,改变不良生活方式,必要时采取药物控制是控制血脂异常的重要措施[27]。部分国家已经提出针对胆固醇管理的国家策略,如美国为预防心脏病开展的“百万心脏”计划,提出“ABCS”策略,其中C代表胆固醇管理,将其与阿司匹林、血压管理、戒烟共同作为预防心血管疾病的重要策略[28]。我国的部分研究和政策也提出[29-30],应将血脂异常与高血糖、高血压的管理共同纳入健康管理实现“三高共管”,是对血脂管理的有益尝试。
本研究基于GBD2017研究结果对中国及各省高LDL-C归因疾病负担作了分析,省间数据具有可比性。但本研究仅探讨了LDL-C高于理论最小暴露水平时可能对IHD和IS死亡、伤残负担的影响,处于或小于理论最小暴露水平下对其他疾病是否产生影响仍需进一步探讨。有证据表明,中国人群TG异常率也较高且可能与动脉粥样硬化性疾病有关联[6, 31],建议今后对高TG造成的疾病负担作进一步测算。
利益冲突 所有作者均声明不存在利益冲突
| [1] |
Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies:a consensus statement from the european atherosclerosis society consensus panel[J]. Eur Heart J, 2017, 38(32): 2459-2472. DOI:10.1093/eurheartj/ehx144 |
| [2] |
Silverman MG, Ference BA, Im K, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions:a systematic review and Meta-analysis[J]. JAMA, 2016, 316(12): 1289-1297. DOI:10.1001/jama.2016.13985 |
| [3] |
中国成人血脂异常防治指南修订联合委员会. 中国成人血脂异常防治指南(2016年修订版)[J]. 中国循环杂志, 2016, 31(10): 937-950. Joint Committee on the Revision of Guidelines for the Prevention and Treatment of Adult Dyslipidemia in China. Guidelines for prevention and treatment of dyslipidemia in Chinese adults (2016)[J]. Chin Circ J, 2016, 31(10): 937-950. DOI:10.3969/j.issn.1000-3614.2016.10.001 |
| [4] |
Zhou MG, Wang HD, Zeng XY, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017:a systematic analysis for the global burden of disease study 2017[J]. Lancet, 2019, 394(10204): 1145-1158. DOI:10.1016/S0140-6736(19)30427-1 |
| [5] |
胡盛寿, 高润霖, 刘力生, 等. 《中国心血管病报告2018》概要[J]. 中国循环杂志, 2019, 34(3): 209-220. Hu SS, Gao RL, Liu LS, et al. Summary of the 2018 report on cardiovascular diseases in China[J]. Chin Circ J, 2019, 34(3): 209-220. DOI:10.3969/j.issn.1000-3614.2019.03.001 |
| [6] |
Zhang M, Deng Q, Wang LH, et al. Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults:a nationally representative survey of 163641 adults[J]. Int J Cardiol, 2018, 260: 196-203. DOI:10.1016/j.ijcard.2017.12.069 |
| [7] |
中国疾病预防控制中心, 中国疾病预防控制中心慢性非传染性疾病预防控制中心. 中国慢性病及其危险因素监测报告-2010[M]. 北京: 军事医学科学出版社, 2012. Chinese Center for Disease Control and Prevention, National Center for Chronic and Non-communicable Disease Control and Prevention, China CDC. Report on chronic disease risk factor surveillance in China (2010)[M]. Beijing: Military Medical Science Press, 2012. |
| [8] |
Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol:a report of the American College Of Cardiology/American Heart Association task force on clinical practice guidelines[J]. J Am Coll Cardiol, 2019, 73(24): e285-350. DOI:10.1016/j.jacc.2018.11.003 |
| [9] |
2014年中国胆固醇教育计划血脂异常防治建议专家组, 中华心血管病杂志编辑委员会, 血脂与动脉粥样硬化循证工作组, 等. 2014年中国胆固醇教育计划血脂异常防治专家建议[J]. 中华心血管病杂志, 2014, 42(8): 633-636. China Cholesterol Education Program Recommended Expert Group on the Prevention and Treatment of Dyslipidemia (2014), Editorial Board of Chinese Journal of Cardiovascular Disease, Evidence-Based Working Group on Lipids and Atherosclerosis, et al. China cholesterol education program experts recommendations for treatment of dyslipidemia[J]. Chin Circulat J, 2014, 42(8): 633-636. DOI:10.3760/cma.j.issn.0253-3758.2014.08.003 |
| [10] |
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias:lipid modification to reduce cardiovascular risk[J]. Eur Heart J, 2020, 41(1): 111-188. DOI:10.1093/eurheartj/ehz455 |
| [11] |
GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017:a systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet, 2018, 392(10159): 1923-1994. DOI:10.1016/S0140-6736(18)32225-6 |
| [12] |
GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017:a systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet, 2018, 392(10159): 1859-1922. DOI:10.1016/S0140-6736(18)32335-3 |
| [13] |
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017:a systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet, 2018, 392(10159): 1736-1788. DOI:10.1016/S0140-6736(18)32203-7 |
| [14] |
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017:a systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet, 2018, 392(10159): 1789-1858. DOI:10.1016/S0140-6736(18)32279-7 |
| [15] |
杨静, 王卓群, 赵艳芳, 等. 2013年中国归因于高血清总胆固醇的疾病负担研究[J]. 中华预防医学杂志, 2016, 50(9): 764-768. Yang J, Wang ZQ, Zhao YF, et al. Burden of disease attributed to high total cholesterol in 2013 in China[J]. Chin J Prev Med, 2016, 50(9): 764-768. DOI:10.3760/cma.j.issn.0253-9624.2016.09.004 |
| [16] |
刘明波, 王文, 马丽媛, 等. 1990至2010年中国居民高胆固醇血症疾病负担分析[J]. 中华心血管病杂志, 2015, 43(9): 802-805. Liu MB, Wang W, Ma LY, et al. Change on burden of diseases from hypercholesterolemia among the Chinese population from 1990 to 2010[J]. Chin J Cardiol, 2015, 43(9): 802-805. DOI:10.3760/cma.j.issn.0253-3758.2015.09.012 |
| [17] |
Feig JE, Hewing B, Smith JD, et al. High-density lipoprotein and atherosclerosis regression:evidence from preclinical and clinical studies[J]. Circ Res, 2014, 114(1): 205-213. DOI:10.1161/CIRCRESAHA.114.300760 |
| [18] |
Duprez DA, Otvos J, Tracy RP, et al. High-density lipoprotein subclasses and non-cardiovascular, non-cancer chronic inflammatory-related events versus cardiovascular events:the multi-ethnic study of atherosclerosis[J]. J Am Heart Assoc, 2015, 4(9): e002295. DOI:10.1161/JAHA.115.002295 |
| [19] |
靳林, 周雪, 姜戈. 2013年黑龙江省成年人血脂异常流行调查研究[J]. 慢性病学杂志, 2017, 18(9): 954-956. Jin L, Zhou X, Jiang G. Epidemic characteristics of adult dyslipidemia in Heilongjiang province in 2013[J]. Chron Pathematol J, 2017, 18(9): 954-956. DOI:10.16440/j.cnki.1674-8166.2017.09.002 |
| [20] |
王明杰, 邵双双, 王燕, 等. 2013年吉林省居民高血脂患病情况及影响因素分析[J]. 实用预防医学, 2018, 25(4): 508-510. Wang MJ, Shao SS, Wang Y, et al. Prevalence of hyperlipemia and its influencing factors among residents in Jilin Province, 2013[J]. Pract Prev Med, 2018, 25(4): 508-510. DOI:10.3969/j.issn.1006-3110.2018.04.035 |
| [21] |
梁丹艳. 2013、2015年内蒙古地区高血压、糖尿病及血脂异常流行状况及影响因素研究[D].呼和浩特: 内蒙古医科大学, 2018. Liang DY. Study on prevalence and influencing factors of hypertension, diabetes and dyslipidemia in Inner Mongolia, 2013 and 2015[D]. Hohhot: Inner Mongolia Medical University, 2018. |
| [22] |
中国高血压调查研究组. 2012-2015年我国≥ 35岁人群血脂异常状况调查[J]. 中国循环杂志, 2019, 34(7): 681-687. China Hypertension Survey Investigators. Status of dyslipidemia among adults aged 35 years and above in China[J]. Chin Circ J, 2019, 34(7): 681-687. DOI:10.3969/j.issn.1000-3614.2019.07.011 |
| [23] |
李配瑶.中国40岁以上人群主要心脑血管病死亡及影响因素分析[D].北京: 中国疾病预防控制中心, 2018. Li PY. A vital surveillance based descriptive study: death of main cardiovascular diseases and its influential factors for Chinese adults aged above 40[D]. Beijing: Chinese Center for Disease Control and Prevention, 2018. http://cdmd.cnki.com.cn/Article/CDMD-84501-1018274411.htm |
| [24] |
Zhang GS, Yu CH, Zhou MG, et al. Burden of ischemic heart disease and attributable risk factors in China from 1990 to 2015:findings from the global burden of disease 2015 study[J]. BMC Cardiovasc Disord, 2018, 18(1): 18. DOI:10.1186/s12872-018-0761-0 |
| [25] |
李剑虹, 王丽敏, 米生权, 等. 2010年我国成年人血脂异常知晓率和治疗率及控制率调查[J]. 中华预防医学杂志, 2012, 46(8): 687-691. Li JH, Wang LM, Mi SQ, et al. Awareness rate, treatment rate and control rate of dyslipidemia in Chinese adults, 2010[J]. Chin J Prev Med, 2012, 46(8): 687-691. DOI:10.3760/cma.j.issn.0253-9624.2012.08.004 |
| [26] |
中国疾病预防控制中心, 中国疾病预防控制中心慢性非传染性疾病预防控制中心. 中国慢性病及其危险因素监测报告2013[M]. 北京: 军事医学出版社, 2016. Chinese Center for Disease Control and Prevention, National Center for Chronic and Non-communicable Disease Control and Prevention, China CDC. National Center for Chronic and Non-communicable Disease Control and Prevention, China CDC. Report on chronic disease risk factors surveillance in China (2013)[M]. Beijing: Military Medical Science Press, 2016. |
| [27] |
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias:lipid modification to reduce cardiovascular risk[J]. Eur Heart J, 2019, 41(1): 111-188. DOI:10.1093/eurheartj/ehz455 |
| [28] |
Farley T, Demaria AN, Wright J, et al. CDC grand rounds:the million hearts initiative[J]. JAMA, 2013, 309(12): 1221-1223. DOI:10.1001/jama.2013.221 |
| [29] |
赵文华, 孔灵芝, 霍勇. 血脂异常应成为基层慢性病健康管理的核心内容[J]. 中华健康管理学杂志, 2018, 12(4): 289-291. Zhao WH, Kong LZ, Huo Y. Making dyslipidemia the core of health management for chronic diseases at the grass-roots level[J]. Chin J Health Manag, 2018, 12(4): 289-291. DOI:10.3760/cma.j.issn.1674-0815.2018.04.001 |
| [30] |
健康中国行动推进委员会.健康中国行动(2019-2030年)[EB/OL]. (2019-07-15)[2019-12-03]. http://www.nhc.gov.cn/guihuaxxs/s3585u/201907/e9275fb95d5b4295be8308415d4cd1b2.shtml. Healthy China Action Promotion Committee. Healthy China action, 2019-2030[EB/OL]. (2019-07-15)[2019-12-03].http://www.nhc.gov.cn/guihuaxxs/s3585u/201907/e9275fb95d5b4295be8308415d4cd1b2.shtml. |
| [31] |
Pan L, Yang ZH, Wu Y, et al. The prevalence, awareness, treatment and control of dyslipidemia among adults in China[J]. Atherosclerosis, 2016, 248: 2-9. DOI:10.1016/j.atherosclerosis.2016.02.006 |
 2020, Vol. 41
2020, Vol. 41