文章信息
- 吴竞, 温子豪, 刘丹丹, 吴晨飞, 张勇, 张兰, 徐友兰, 杨光, 荆春霞.
- Wu Jing, Wen Zihao, Liu Dandan, Wu Chenfei, Zhang Yong, Zhang Lan, Xu Youlan, Yang Guang, Jing Chunxia
- 不同通气策略对新生儿呼吸窘迫综合征治疗的安全性评价:网状Meta分析
- Safety evaluation on different ventilation strategies set for neonatal respiratory distress syndrome: a network Meta-analysis
- 中华流行病学杂志, 2020, 41(2): 249-260
- Chinese Journal of Epidemiology, 2020, 41(2): 249-260
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2020.02.020
-
文章历史
收稿日期: 2019-05-05
2. 暨南大学病原生物学教研室, 广州 510632;
3. 中山大学医学院, 广州 510080;
4. 东莞市妇幼保健院新生儿科 523000
2. Department of Pathogenic Biology, Jinan University, Guangzhou 510632, China;
3. School of Medicine, Zhongshan University, Guangzhou 510080, China;
4. Department of Neonatology, Dongguan Maternal and Child Health Hospital, Dongguan 523000, China
新生儿呼吸窘迫综合征(neonatal respiratory distress syndrome,NRDS)也称为新生儿透明膜病,是由肺泡表面活性物质缺乏且肺泡萎陷所致的早产儿常见疾病,患儿出生后只有短暂的自然呼吸,后表现为呼吸困难、发绀、吸气三凹征,甚至导致呼吸衰竭和死亡[1]。NRDS是可治的,2016年NRDS管理的欧洲共识指南给出以表面活性剂治疗为主[2],补充稳定的氧气,辅助性采用呼吸通气策略,注意血压和灌注管理的治疗方案。机械通气作为NRDS治疗的必要手段,因机械呼吸机强制开放肺泡,不可避免地导致肺损伤[3],再加上NRDS患儿具有较高死亡率和并发症发生率,通气策略的及时正确选择在保护新生儿的生命安全和疾病转归中起着关键作用[4]。在通气策略中选取出合适的一种或两种需要借助循证医学手段(如Meta分析),而传统的Meta分析仅限于直接比较2种干预措施,观察范围较窄。而NRDS患儿的通气策略种类繁多,采用传统Meta分析,工作量大,且无法分析缺乏直接比较证据的两种通气策略的有效性及安全性。而网状Meta分析能够基于传统Meta分析对多种通气策略进行直接或间接比较,合理有效的解决了传统Meta分析无法同时对多种通气策略进行分析的局限性,为临床决策者选择最有效的治疗方法提供有力的证据[5]。因此,本研究通过整合网状Meta分析中所有可用的直接和间接证据,评估不同通气策略对NRDS的安全性。
资料与方法1.资料来源及检索策略:计算机检索1986年1月至2018年6月期间由PubMed、Cochrane、Web of Science、EBSCO和Springer Link数据库以英文形式收录的平均孕周<32周且符合NRDS诊断标准的早产儿肺通气策略的临床随机对照试验(RCTs)。将关键词neonatal respiratory distress syndrome,treatments,preterm infants,neonates,ventilation,oxygen therapy,continuous positive airway pressure,premature baby,randomized controlled trials,and exogenous pulmonary surfactants连接成为一个语句进行检索。
2.文献纳入与排除:纳入标准:①患者为早产儿(平均孕周<32周)NRDS;②实验组和对照组患儿均使用呼吸机进行肺通气治疗,不限制通气策略;③研究类型为RCTs;④使用肺表面活性物质。排除标准:①病例报告、评论、实验研究、观察性研究、回顾性研究以及会议和方案;②偏倚风险高的试验;③NRDS定义不明确的研究;④仅进行了肺表面活性物质研究的文献;⑤研究对象不是早产儿;⑥主要结果不可用或无法获得全文;⑦在1990年之前发表的研究。
3.资料提取和结局指标的定义:
(1)资料提取:①研究的基线资料:第一作者、发表时间、通气策略、例数、性别、随访、出生体重、孕周和结局指标的相关数据。②通气策略的纳入:本次共纳入了11种机械通气策略,包括高频震荡通气(high-frequency oscillation ventilation,HFOV)、高频喷射通气(high-frequency jet ventilation,HFJV)、常频通气(conventional mechanical ventilation,CMV)、双水平正压通气(bilevel positive airway pressure,BiPAP)、同步经鼻间歇压通气(synchronized nasal intermittent positive pressure ventilation,SNIPPV)、同步间歇性机械通气(synchronized intermittent mechanical ventilation,SIMV)、压力支持联合容量保证通气(pressure support ventilation+volume guarantee,PSV+VG)、经鼻间歇压通气(nasal intermittent positive pressure ventilation,NIPPV)、经鼻连续呼吸道正压通气(nasal continuous positive airway pressure,NCPAP)、插管-表面活性剂-拔管策略(intubate-surfactant-extubate,INSURE)、间歇性指令通气(intermittent mandatory ventilation,IMV)。在本次研究中常规通气(conventional ventilation,CV)和机械通气(mechanical ventilation,MV)被定义为CMV。③结局指标:包括死亡率、动脉导管未闭(patent ductus arteriosus,PDA)、视网膜病变(retinopathy of prematurity,ROP)和脑室出血(intraventricular hemorrhage,IVH)。
(2)结局指标的定义:本研究以死亡率和IVH作为主要观察结局,ROP和PDA作为次要观察结局。死亡率定义为因NRDS而死亡的频率。IVH定义为早产儿伴发NRDS经通气治疗后出现颅内血管破裂出血,通过CT扫描或多普勒超声诊断确诊。ROP定义为新生儿眼部视网膜血管增殖性病变,根据眼底检查确诊。PDA定义为NRDS患儿出生后72 h动脉导管仍未自发性关闭,根据心电图、超声心动图、胸部X线检查或升主动脉造影检查确诊。IVH根据Papile grade进行分级[6],本研究仅纳入Ⅲ~Ⅳ级数据,Ⅲ级:IVH伴有心室扩张;Ⅳ级:IVH伴脑实质性血肿。由于ROP和PDA在各个国家的分级标准不一致,不对ROP和PDA的纳入级别进行限制。
4.质量控制:本次研究由2名经统一培训的研究者独立进行初筛,并根据文献纳入排除标准进行文献取舍。在文献筛选阶段出现的不同意见时,则由第3位研究者决定是否纳入。为了评价所纳入文献的质量,本研究采用Cochrane偏倚风险工具进行偏倚评价[7],其中主要包括:随机序列生成、分配隐藏、参与者和人员致盲、结果评估盲法、不完整结果数据、选择性报告和其他偏见来源。
5.统计学方法:本次所有结局指标均为二分类数据,为了最大化准确度,本研究采用OR值和95%CI评估每种通气治疗策略的安全性。采用Revman 5.3软件对符合纳入标准的文献进行Cochrane偏倚评价。采用基于贝叶斯框架的Winbugs 1.4.3软件对数据进行分析,Gibbs抽样和马尔科夫-蒙特卡罗(MCMC)方法进行贝叶斯推断[8],并在假定MCMC已经达到收敛状态下进行估计和推断。WinBUGS设置模拟链2条,痕迹拟合度用于判断结果稳定性,迭代次数设置为10万次,前1万次用于退火以消除初始值的影响,初始值设置为0.5。对于初始值为“0”的事件,采用0.5进行矫正。采用STATA 13.0软件进行Inconsistency图、漏斗图、网络图、累积排序图、聚类排序图的绘制。将出生体重和孕龄作为协变量添加到网状Meta分析中进行Meta回归分析以评估网状Meta分析的相似性[9-10]。采用Inconsistency图表示每个结局指标中的环不一致性,环不一致性因子(IF值)的95%CI下限若为0,则说明环不具有不一致性。漏斗图用于检验发表偏倚,Egger检验用于数字化发表偏倚结果。基于累积曲线下面积(surface under the cumulative ranking curve,SUCRA)值绘制累积排序和聚类排序图,用于观察最佳通气策略,SUCRA值范围为0~100,越接近100,说明该干预措施成为最佳干预措施的可能性越大。
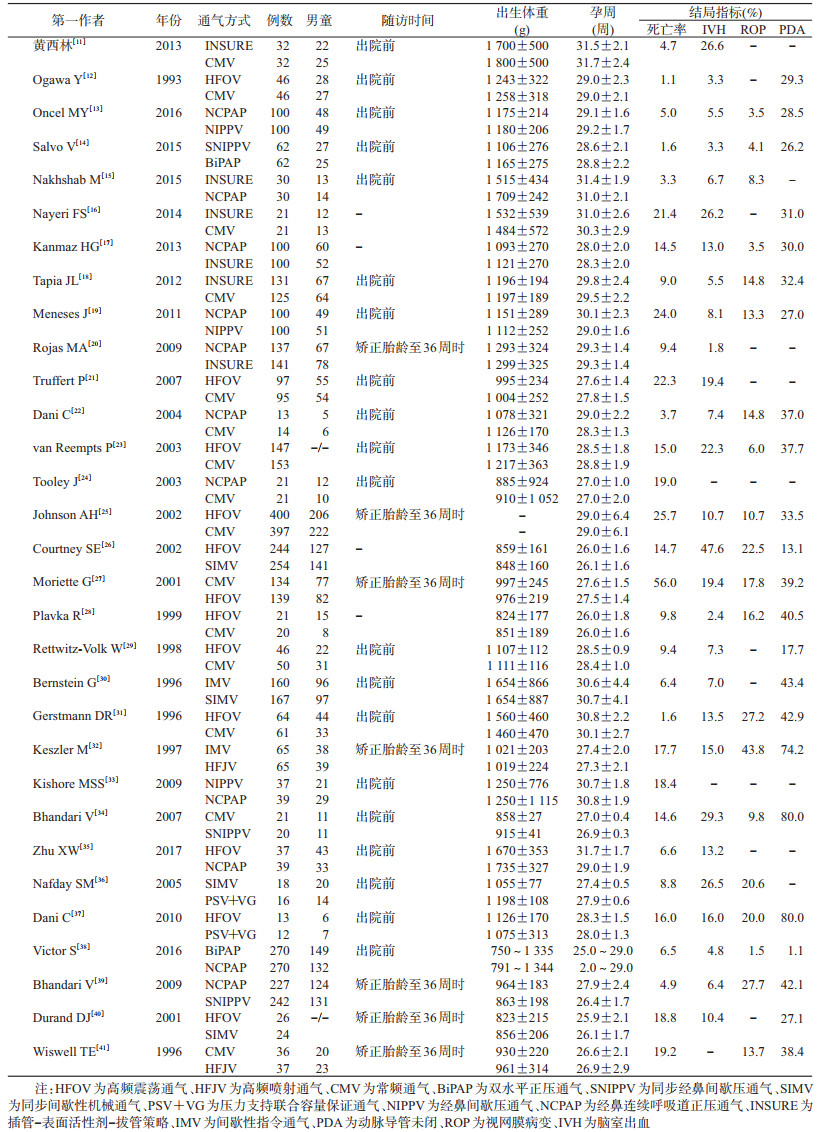
结果1.纳入文献的基线资料:纳入的31项研究均发表于1990-2018年,共5 829例早产儿,平均孕周为25.9~32.0周,平均出生体重为750~1 800 g,均为双臂研究。所有研究(5 827例患儿)均报道了死亡率结局,28项研究(5 546例患儿)报道了IVH结局,17项研究(4 176例患儿)报道了ROP结局,22项研究(4 873例患儿)报道了PDA结局。见表 1。
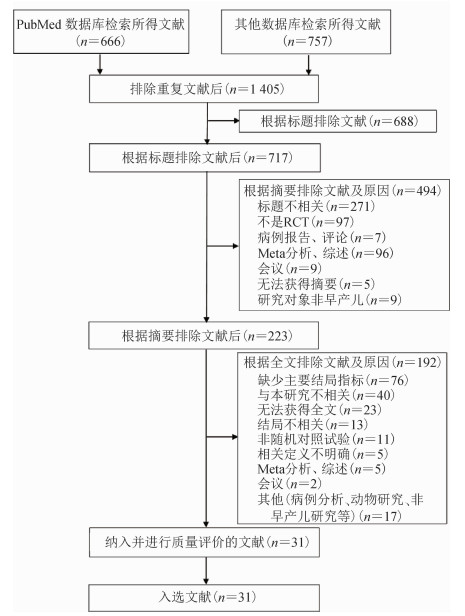
2.文献检索及文献质量评价:共检索得到1 423篇文献,最终纳入文献31篇,流程见图 1。31篇文献中除2项研究外,均提到使用随机方法对研究对象进行分组。1项研究未报告分配隐藏,1项研究具有结果评估盲法偏倚的高风险,7项研究未报告研究人员致盲与否。由于新生儿几乎无认知能力,无法区分干预差异,故认为所有参与者均被致盲。文献质量评估见图 2。
|
| 图 1 文献筛选流程图 |

|
| 图 2 纳入文献质量评价 |
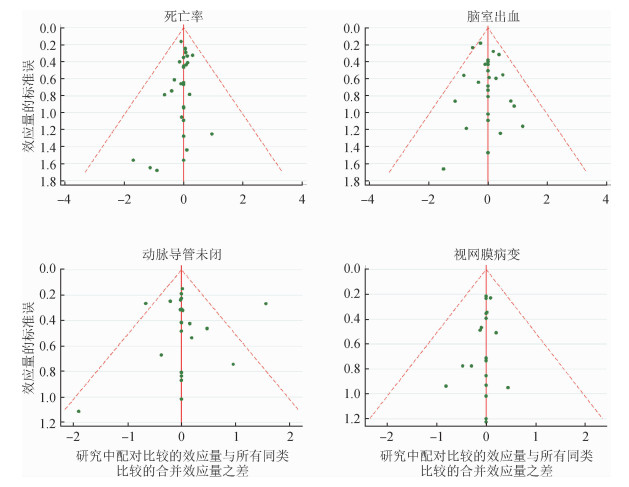
3.环不一致性、相似性和发表偏倚评价:本次研究采用Inconsistency图展示4个结局的环不一致性,IF值的95%CI下限均为0,提示闭合环具有一致性,见图 3。对于相似性分析,Meta回归结果显示,出生体重和孕龄对实际估计存在影响,出生体重越重和孕龄越大的患儿,更易于获得更佳的预后。漏斗图和Egger检验结果(死亡率P=0.155;IVH P=0.901;PDA P=0.097;ROP P=0.207)均显示不存在发表偏倚。见图 4。

|
| 注:HFOV为高频震荡通气、HFJV为高频喷射通气、CMV为常频通气、BiPAP为双水平正压通气、SNIPPV为同步经鼻间歇压通气、SIMV为同步间歇性机械通气、PSV+VG为压力支持联合容量保证通气、NCPAP为经鼻连续呼吸道正压通气、INSURE为插管-表面活性剂-拔管策略、IMV为间歇性指令通气 图 3 环不一致性检验(Inconsistency图) |
|
| 图 4 主要指标发表偏倚漏斗图 |
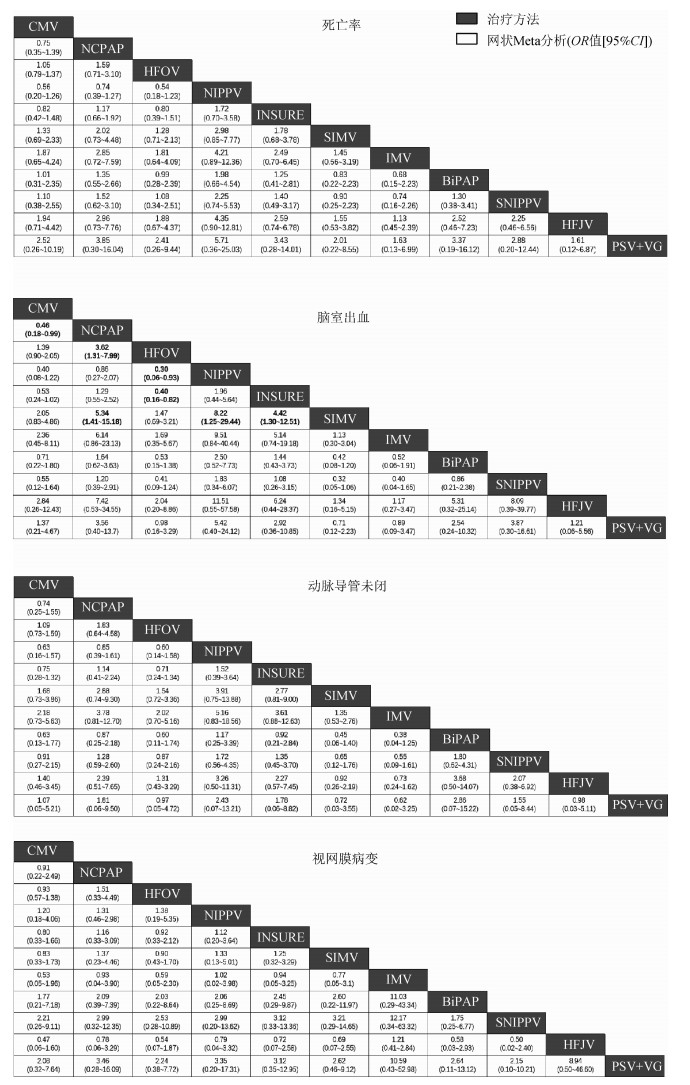
4.网络图和网状Meta分析:4个结局指标的网络图见图 5,其中接受HFOV、CMV和NCPAP治疗的患儿最多,分别有1 322、1 265和1 076例,高于其他通气策略。各项结局的总发生率为死亡率为14.95%(871/5 827),IVH为13.76%(763/5 546),PDA为30.02%(1 463/4 873),ROP为13.48%(563/4 176)。对于死亡率、PDA和ROP,11项通气策略间差异无统计学意义。与NIPPV相比,HFOV(OR=3.33,95%CI:1.08~16.67),SIMV(OR=8.22,95%CI:1.25~29.44)增加了NRDS患IVH的风险。INSURE导致IVH的可能性低于SIMV(OR=0.23,95%CI:0.08~0.77)和HFOV(OR=0.40,95%CI:0.16~0.82)。见图 6。

|
| 注:节点的大小与样本量呈正比,线的宽度表示直接比较试验的数量;HFOV为高频震荡通气、HFJV为高频喷射通气、CMV为常频通气、BiPAP为双水平正压通气、SNIPPV为同步经鼻间歇压通气、SIMV为同步间歇性机械通气、PSV+VG为压力支持联合容量保证通气、NIPPV为经鼻间歇压通气、NCPAP为经鼻连续呼吸道正压通气、INSURE为插管-表面活性剂-拔管策略、IMV为间歇性指令通气 图 5 网络证据图 |
|
| 注:为方便描述OR值及95%CI,所有数据均取倒数进行描述;HFOV为高频震荡通气、HFJV为高频喷射通气、CMV为常频通气、BiPAP为双水平正压通气、SNIPPV为同步经鼻间歇压通气、SIMV为同步间歇性机械通气、PSV+VG为压力支持联合容量保证通气、NIPPV为经鼻间歇压通气、NCPAP为经鼻连续呼吸道正压通气、INSURE为插管-表面活性剂-拔管策略、IMV为间歇性指令通气 图 6 网状Meta分析结果 |
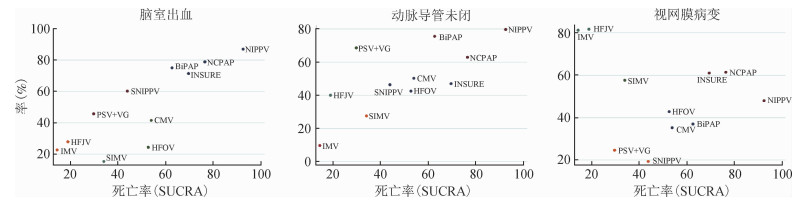
5.等级累积概率排序和聚类排序:对于死亡率和IVH,NIPPV在11种通气策略中成为最佳的通气策略的累积概率最高;对于PDA,NIPPV则排在第二位的可能性最大,在ROP结局中NIPPV排在第三位的可能性最大,见图 7。在死亡率-IVH、死亡率-PDA和死亡率-ROP的聚类排序中,NIPPV和NCPAP具有较高排名(基于SUCRA值),提示在平衡4种不良结局后,NIPPV可能是NRDS的最佳通气策略。见图 8。

|
| 注:不同色块表示排名,色块越大表示该种通风策略按此顺序排序的概率越大;HFOV为高频震荡通气、HFJV为高频喷射通气、CMV为常频通气、BiPAP为双水平正压通气、SNIPPV为同步经鼻间歇压通气、SIMV为同步间歇性机械通气、PSV+VG为压力支持联合容量保证通气、NIPPV为经鼻间歇压通气、NCPAP为经鼻连续呼吸道正压通气、INSURE为插管-表面活性剂-拔管策略、IMV为间歇性指令通气 图 7 累积概率排序 |
|
| 注:基于SUCRA值进行聚类分析,每个图显示2种结果的SUCRA值,每种颜色代表属于同一簇,位于右上角的通气策略更有效;HFOV为高频震荡通气、HFJV为高频喷射通气、CMV为常频通气、BiPAP为双水平正压通气、SNIPPV为同步经鼻间歇压通气、SIMV为同步间歇性机械通气、PSV+VG为压力支持联合容量保证通气、NIPPV为经鼻间歇压通气、NCPAP为经鼻连续呼吸道正压通气、INSURE为插管-表面活性剂-拔管策略、IMV为间歇性指令通气 图 8 聚类排序图 |
NRDS是早产儿常见病,死亡率与早产儿体重具有明显相关,即体重越低,死亡率越高[42]。2016年“新生儿呼吸窘迫综合征欧洲共识指南”要求NRDS患儿要采用肺表面活性剂治疗,同时首选无创性通气(NIV)进行联合治疗。与有创机械通气相比,NIV能够显著减轻呼吸道损伤和呼吸肌疲劳[43]。柏林的一项研究发现[44],仅有38.6%的患儿接受了NIV治疗,且NIV治疗的失败率高达71%,院内死亡率高达62.7%。且当肺部疾病严重时,NIV难以改善二氧化碳潴留,其中约43%~80%的中重度呼吸窘迫的新生儿需要进行气管插管和有创通气[45]。且在部分医疗技术不发达的区域有创机械通气策略仍然是必要的和有效的。由此,NIV和有创通气策略在NRDS群体中的应用价值一直受到争议。有研究显示,由于不同呼吸机厂商间的竞争以及参数的可调节性,使得NRDS通气策略高达30余种[46]。在我国,常用于NRDS的通气策略主要有CMV、IMV、HFV、NCPAP、NIPPV、SIMV、BiPAP以及INSURE等,临床决策者在为NRDS患儿选择合适的通气策略时存在争议。因此本研究中,通过网状Meta分析的方法对应用于NRDS患儿的11种通气策略进行安全性评估。
在本研究中,共比较了11种NRDS通气策略的安全性,并发现NIPPV可能是最佳的通气策略。2015年的1篇网状Meta分析发表纳入了20项研究[47],2 832例新生儿接受了16种通气模式中的1或2种,结果较为可靠,且做了大量的循证医学工作,但>80%的直接比较只有1项研究支持,网络中仅存在3个环,使得结果的偶然性增加。2017年的另1篇网状Meta分析发表在纳入和排除标准方面优于前者[48],但仅观察了7种NIV策略,使得结果缺少有创通气策略的比较,相似地,2015年的分析也放弃了NIV策略,如NCPAP、NIPPV、INSURE等。而本研究将NIV策略与有创通气策略合并比较,且使得>60%的直接比较超过2个证据支持,以期获得更加全面和稳定的结果。
死亡是NRDS的最差的结局,在本研究中,11项通气策略相比差异无统计学意义,然而在排序结果中显示NIPPV和NCPAP可能是减少NRDS患儿死亡的最佳通气方法,但概率排名仅仅是对多种通气方案的可能的排序,不能单独作为最终参考依据,通过结合直接和间接证据各种通气策略对NRDS患儿死亡率的有效性则具有更大的参考意义。一项国外研究通过传统Meta分析中发现,与NCPAP相比,NIPPV没有明显降低NRDS患儿死亡率的趋势[49]。一项在爱尔兰进行的研究发现,NIPPV治疗由于其具有更低的死亡率,越来越多的应用于新生儿病房,间接证实了本研究的正确性[50]。研究显示,NRDS(OR=3.8,95%CI:1.5~9.4)和机械通气(OR=23.6,95%CI:5.1~109.5)是IVH发生的主要危险因素[51]。IVH是导致NRDS死亡的主要原因之一,NIPPV也能够减少IVH的发生率。本研究通过贝叶斯固定效应模型,对包含有5 546名NRDS患儿的28项RCTs进行网状Meta分析。与HFOV和SIMV相比NIPPV能够减少IVH发生率,且在概率排序中SUCRA值高达87.1。相似地,在PDA和ROP结局中排序也靠前。聚类排序结果在平衡了4种不良结局后也表明NIPPV可能是最佳的通气策略。这可能是由于NIPPV通过更加符合生理条件的参数为NRDS患儿提供吸气气道压力和呼气气道压力,增加肺泡通气,改善呼吸肌功能,降低呼吸功率消耗,纠正高碳酸血症[52]。而本研究中发现IMV、HFOV改善4种不良结局的效果较差。这可能是由于HFOV的通气频率(>150次/min)远大于生理情况,且此种模式一般选择大容量通气,20%~80%的解剖死腔气体要通过活塞进入气道,从而使得动脉压迅速升高[53]。由于早产儿血管自主调节神经节发育不成熟,动脉压迅速升高意味着脑毛细血管出血,从而导致IVH。IMV和SIMV能够导致过度通气,从而使得中心静脉压(MAP)升高并发生呼吸性碱中毒,且IMV和SIMV无法满足部分患儿呼吸气体流速,患儿需要进行额外的呼吸做功,进一步增加肺动脉压和MAP[54]。从而使得上腔静脉压力增加,阻碍脑静脉回流,异常增加颅内血管容积,导致脑血管破裂而发生IVH[55]。上述结果提示NIPPV可以作为NRDS患儿的首选NIV通气策略。而通过Meta回归分析,出生体重和孕龄对本研究结局存在一定影响,这是由于出生体重越低和孕龄越小的患儿,死亡率和并发症发生率越高,是符合临床实际的,故不作为本研究结局影响因素进行考虑。
本研究存在一定局限性。由于缺乏证据支持,未对NRDS其他的并发症如支气管肺发育不良(bronchopulmonary dysplasia)和败血症等进行评估。同时纳入研究的基线特征存在一定差异,仅限制了平均孕龄,同时由于研究报道的差异使得其间所用的肺表面活性剂不同或定义不明确,可能会导致结果出现一定偏倚。未来研究应在研究证据足够的基础上着重改善上述不足。
综上所述,临床决策者在采用机械通气治疗NRDS患儿时可首选NIPPV,以降低IVH发生率,改善死亡、PDA和ROP的发生情况,不建议采用HFOV、SIMV和IMV对孕周<32周的NRDS患儿应用。
利益冲突 所有作者均声明不存在利益冲突
| [1] |
Oh KJ, Park JY, Lee JH, et al. The combined exposure to intra-amniotic inflammation and neonatal respiratory distress syndrome increases the risk of intraventricular hemorrhage in preterm neonates[J]. J Perinat Med, 2017, 46(1): 9-20. DOI:10.1515/jpm-2016-0348 |
| [2] |
欧洲新生儿呼吸窘迫综合征防治共识指南: 2016版[J].中华儿科杂志, 2017, 55(3): 169-176. DOI: 10.1159/000448985. European consensus guidelines for the prevention and treatment of neonatal respiratory distress syndrome[J]. Chin J Pediatr, 2017, 55(3): 169-176. DOI: 10.1159/000448985. |
| [3] |
Greenough A, Lingam I. Invasive and non-invasive ventilation for prematurely born infants-current practice in neonatal ventilation[J]. Expert Rev Respir Med, 2016, 10(2): 185-192. DOI:10.1586/17476348.2016.1135741 |
| [4] |
王华, 母得志. 新生儿呼吸窘迫综合征的通气策略[J]. 中华妇幼临床医学杂志:电子版, 2017, 13(1): 10-13. Wang H, Mu DZ. Ventilation strategies of the neonatal respiratory distress syndrome[J]. Chin J Obstetr Gynecol Pediatr:Electron Ed, 2017, 13(1): 10-13. DOI:10.3877/cma.j.issn.1673-5250.2017.01.002 |
| [5] |
Lumley T. Network Meta-analysis for indirect treatment comparisons[J]. Stat Med, 2002, 21(16): 2313-2324. DOI:10.1002/sim.1201 |
| [6] |
Papile LA, Munsick-Bruno G, Schaefer A. Relationship of cerebral intraventricular hemorrhage and early childhood handicaps[J]. J Pediatr, 1983, 103(2): 273-277. DOI:10.1016/S0022-3476(83)80366-7 |
| [7] |
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions:cochrane book series[M]. England: Wiley, 2008.
|
| [8] |
Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons[J]. Stat Med, 2004, 23(20): 3105-3124. DOI:10.1002/sim.1875 |
| [9] |
White IR. Multivariate random-effects Meta-regression:updates to mvmeta[J]. Stata J, 2011, 11(2): 255-270. DOI:10.1177/1536867X1101100206 |
| [10] |
Jackson D, Riley R, White IR. Multivariate Meta-analysis:potential and promise[J]. Stat Med, 2011, 30(20): 2481-2498. DOI:10.1002/sim.4172 |
| [11] |
黄西林, 陈丹, 李小萍, 等. INSURE策略治疗新生儿呼吸窘迫综合征的临床研究[J]. 中国当代儿科杂志, 2013, 15(1): 9-13. Huang XL, Chen D, Li XP, et al. Clinical effectiveness of INSURE method in the treatment of neonatal respiratory distress syndrome[J]. Chin J Contemp Pediatr, 2013, 15(1): 9-13. DOI:10.7499/j.issn.1008-8830.2013.01.004 |
| [12] |
Ogawa Y, Miyasaka K, Kawano T, et al. A multicenter randomized trial of high frequency oscillatory ventilation as compared with conventional mechanical ventilation in preterm infants with respiratory failure[J]. Early Human Dev, 1993, 32(1): 1-10. DOI:10.1016/0378-3782(93)90088-C |
| [13] |
Oncel MY, Arayici S, Uras N, et al. Nasal continuous positive airway pressure versus nasal intermittent positive-pressure ventilation within the minimally invasive surfactant therapy approach in preterm infants:a randomised controlled trial[J]. Arch Dis Child Fetal Neonatal Ed, 2016, 101(4): F323-328. DOI:10.1136/archdischild-2015-308204 |
| [14] |
Salvo V, Lista G, Lupo E, et al. Noninvasive ventilation strategies for early treatment of RDS in preterm infants:an RCT[J]. Pediatrics, 2015, 135(3): 444-451. DOI:10.1542/peds.2014-0895 |
| [15] |
Nakhshab M, Tajbakhsh M, Khani S, et al. Comparison of the effect of surfactant administration during nasal continuous positive airway pressure with that of nasal continuous positive airway pressure alone on complications of respiratory distress syndrome:a randomized controlled study[J]. Pediatr Neonatol, 2015, 56(2): 88-94. DOI:10.1016/j.pedneo.2014.05.006 |
| [16] |
Nayeri FS, Esmaeilnia Shirvani T, Aminnezhad M, et al. Comparison of INSURE method with conventional mechanical ventilation after surfactant administration in preterm infants with respiratory distress syndrome:therapeutic challenge[J]. Acta Med Iran, 2014, 52(8): 596-600. |
| [17] |
Kanmaz HG, Erdeve O, Canpolat FE, et al. Surfactant administration via thin catheter during spontaneous breathing:randomized controlled trial[J]. Pediatrics, 2013, 131(2): e502-509. DOI:10.1542/peds.2012-0603 |
| [18] |
Tapia JL, Urzua S, Bancalari A, et al. Randomized trial of early bubble continuous positive airway pressure for very low birth weight infants[J]. J Pediatr, 2012, 161(1): 75-80. DOI:10.1016/j.jpeds.2011.12.054 |
| [19] |
Meneses J, Bhandari V, Alves JG, et al. Noninvasive ventilation for respiratory distress syndrome:a randomized controlled trial[J]. Pediatrics, 2011, 127(2): 300-307. DOI:10.1542/peds.2010-0922 |
| [20] |
Rojas MA, Lozano JM, Rojas MX, et al. Very early surfactant without mandatory ventilation in premature infants treated with early continuous positive airway pressure:a randomized, controlled trial[J]. Pediatrics, 2009, 123(1): 137-142. DOI:10.1542/peds.2007-3501 |
| [21] |
Truffert P, Paris-Llado J, Escande B, et al. Neuromotor outcome at 2 years of very preterm infants who were treated with high-frequency oscillatory ventilation or conventional ventilation for neonatal respiratory distress syndrome[J]. Pediatrics, 2007, 119(4): e860-865. DOI:10.1542/peds.2006-2082 |
| [22] |
Dani C, Bertini G, Pezzati M, et al. Early Extubation and nasal continuous positive airway pressure after surfactant treatment for respiratory distress syndrome among preterm infants < 30 Weeks' gestation[J]. Pediatrics, 2004, 113(6): e560-563. DOI:10.1542/peds.113.6.e560 |
| [23] |
van Reempts P, Borstlap C, Laroche S, et al. Early use of high frequency ventilation in the premature neonate[J]. Eur J Pediatr, 2003, 162(4): 219-226. DOI:10.1007/s00431-002-1145-z |
| [24] |
Tooley J, Dyke M. Randomized study of nasal continuous positive airway pressure in the preterm infant with respiratory distress syndrome[J]. Acta Paediatr, 2003, 92(10): 1170-1174. DOI:10.1111/j.1651-2227.2003.tb02479.x |
| [25] |
Johnson AH, Peacock JL, Greenough A, et al. High-frequency oscillatory ventilation for the prevention of chronic lung disease of prematurity[J]. N Eng J Med, 2002, 347(9): 633-642. DOI:10.1056/nejmoa020432 |
| [26] |
Courtney SE, Durand DJ, Asselin JM, et al. High-frequency oscillatory ventilation versus conventional mechanical ventilation for very-low-birth-weight infants[J]. N Eng J Med, 2002, 347(9): 643-652. DOI:10.1056/NEJMoa012750 |
| [27] |
Moriette G, Paris-Llado J, Walti H, et al. Prospective randomized multicenter comparison of high-frequency oscillatory ventilation and conventional ventilation in preterm infants of less than 30 weeks with respiratory distress syndrome[J]. Pediatrics, 2001, 107(2): 363-372. DOI:10.1203/00006450-199904020-01264 |
| [28] |
Plavka R, Kopecky P, Sebroň V, et al. A prospective randomized comparison of conventional mechanical ventilation and very early high frequency oscillatory ventilation in extremely premature newborns with respiratory distress syndrome[J]. Intensive Care Med, 1999, 25(1): 68-75. DOI:10.1007/s001340050789 |
| [29] |
Rettwitz-Volk W, Veldman A, Roth B, et al. A prospective, randomized, multicenter trial of high-frequency oscillatory ventilation compared with conventional ventilation in preterm infants with respiratory distress syndrome receiving surfactant[J]. J Pediatr, 1998, 132(2): 249-254. DOI:10.1016/S0022-3476(98)70440-8 |
| [30] |
Bernstein G, Mannino FL, Heldt GP, et al. Randomized multicenter trial comparing synchronized and conventional intermittent mandatory ventilation in neonates[J]. J Pediatr, 1996, 128(4): 453-463. DOI:10.1016/S0022-3476(96)70354-2 |
| [31] |
Gerstmann DR, Minton SD, Stoddard RA, et al. The Provo multicenter early high-frequency oscillatory ventilation trial:improved pulmonary and clinical outcome in respiratory distress syndrome[J]. Pediatrics, 1996, 98(6 Pt 1): 1044-1057. DOI:10.1159/000437247 |
| [32] |
Keszler M, Modanlou HD, Brudno DS, et al. Multicenter controlled clinical trial of high-frequency jet ventilation in preterm infants with uncomplicated respiratory distress syndrome[J]. Pediatrics, 1997, 100(4): 593-599. DOI:10.1542/peds.100.4.593 |
| [33] |
Kishore MSS, Dutta S, Kumar P. Early nasal intermittent positive pressure ventilation versus continuous positive airway pressure for respiratory distress syndrome[J]. Acta Paediatr, 2009, 98(9): 1412-1415. DOI:10.1111/j.1651-2227.2009.01348.x |
| [34] |
Bhandari V, Gavino RG, Nedrelow JH, et al. A randomized controlled trial of synchronized nasal intermittent positive pressure ventilation in RDS[J]. J Perinatol, 2007, 27(11): 697-703. DOI:10.1038/sj.jp.7211805 |
| [35] |
Zhu XW, Zhao JN, Tang SF, et al. Noninvasive high-frequency oscillatory ventilation versus nasal continuous positive airway pressure in preterm infants with moderate-severe respiratory distress syndrome:a preliminary report[J]. Pediatr Pulmonol, 2017, 52(8): 1038-1042. DOI:10.1002/ppul.23755 |
| [36] |
Nafday SM, Green RS, Lin J, et al. Is there an advantage of using pressure support ventilation with volume guarantee in the initial management of premature infants with respiratory distress syndrome? A pilot study[J]. J Perinatol, 2005, 25(3): 193-197. DOI:10.1038/sj.jp.7211233 |
| [37] |
Dani C, Bertini G, Pezzati M, et al. Effects of pressure support ventilation plus volume guarantee vs. high-frequency oscillatory ventilation on lung inflammation in preterm infants[J]. Pediatr Pulmonol, 2006, 41(3): 242-249. DOI:10.1002/ppul.20350 |
| [38] |
Victor S, Roberts SA, Mitchell S, et al. Biphasic positive airway pressure or continuous positive airway pressure:a randomized trial[J]. Pediatrics, 2016, 138(2): e20154095. DOI:10.1542/peds.2015-4095 |
| [39] |
Bhandari V, Finer NN, Ehrenkranz RA, et al. Synchronized Nasal Intermittent Positive-Pressure Ventilation and Neonatal Outcomes[J]. Pediatrics, 124(2): 517-526. DOI:10.1542/peds.2008-1302 |
| [40] |
Durand DJ, Asselin JM, Hudak ML, et al. Early high-frequency oscillatory ventilation versus synchronized intermittent mandatory ventilation in very low birth weight infants:a pilot study of two ventilation protocols[J]. J Perinatol, 2001, 21(4): 221-229. DOI:10.1038/sj.jp.7210527 |
| [41] |
Wiswell TE, Graziani LJ, Kornhauser MS, et al. Effects of hypocarbia on the development of cystic periventricular leukomalacia in premature infants treated with high-frequency jet ventilation[J]. Pediatrics, 1996, 98(5): 918-924. |
| [42] |
吴丽霞, 董召斌, 张凤琴, 等. 新生儿急性呼吸窘迫综合征的防治进展[J]. 当代医学, 2019, 25(9): 184-186. Wu LX, Dong ZB, Zhang FQ, et al. Progress in prevention and treatment of neonatal acute respiratory distress syndrome[J]. Contemp Med, 2019, 25(9): 184-186. DOI:10.3969/j.issn.1009-4393.2019.09.084 |
| [43] |
冯爱民, 谢秀春, 王苗, 等. 肺表面活性物质联合无创高频振荡通气治疗新生儿呼吸窘迫综合征的效果观察[J]. 河北医学, 2019, 25(3): 551-555. Feng AM, Xie XC, Wang M, et al. Effect of combined treatment of pulmonary surfactant and non-invasive high frequency oscillatory ventilation on neonatal respiratory distress syndrome[J]. Hebei Med, 2019, 25(3): 551-555. DOI:10.3969/j.issn.1006-6233.2019.03.006 |
| [44] |
Neuschwander A, Lemiale V, Darmon M, et al. Noninvasive ventilation during acute respiratory distress syndrome in patients with cancer:Trends in use and outcome[J]. J Crit Care, 2017, 38: 295-299. DOI:10.1016/j.jcrc.2016.11.042 |
| [45] |
Salvo V, Lista G, Lupo E, et al. Comparison of three non-invasive ventilation strategies (NSIPPV/BiPAP/NCPAP) for RDS in VLBW infants[J]. J Matern Fetal Neonatal Med, 2017, 31(4): 1-22. DOI:10.1080/14767058.2017.1357693 |
| [46] |
Schreiber MD, Marks JD. Noninvasive ventilation in the premature newborn-is less always more?[J]. N Engl J Med, 2017, 377(4): 386-388. DOI:10.1056/NEJMe1707439 |
| [47] |
Wang CS, Guo LB, Chi CJ, et al. Mechanical ventilation modes for respiratory distress syndrome in infants:a systematic review and network Meta-analysis[J]. Crit Care, 2015, 19(1): 108. DOI:10.1186/s13054-015-0843-7 |
| [48] |
Isayama T, Iwami H, McDonald S, et al. Association of noninvasive ventilation strategies with mortality and Bronchopulmonary dysplasia among preterm infants[J]. JAMA, 2016, 316(6): 611-624. DOI:10.1001/jama.2016.10708 |
| [49] |
Lemyre B, Davis PG, de Paoli AG, et al. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation[J]. Cochrane Database Syst Rev, 2014(9): CD003212. DOI:10.1002/14651858.CD003212 |
| [50] |
Kieran EA, Walsh H, O'Donnell CPF. Survey of nasal continuous positive airways pressure (NCPAP) and nasal intermittent positive pressure ventilation (NIPPV) use in Irish newborn nurseries[J]. Arch Dis Child Fetal Neonatal Ed, 2011, 96(2): F156. DOI:10.1136/adc.2010.203190 |
| [51] |
Haroon A, Maheen H, Salat MS, et al. Risk factors for intraventricular haemorrhage in preterm infants from a tertiary care hospital of Karachi, Pakistan[J]. J Pak Med Assoc, 2014, 64(10): 1146-1150. |
| [52] |
Tong S, Gower J, Morgan A, et al. Noninvasive positive pressure ventilation in the immediate post-bariatric surgery care of patients with obstructive sleep apnea:a systematic review[J]. Surg Obes Relat Dis, 2017, 13(7): 1227-1233. DOI:10.1016/j.soard.2017.02.009 |
| [53] |
Luna MS, González MS, Cortijo FT. High-frequency oscillatory ventilation combined with volume guarantee in a neonatal animal model of respiratory distress syndrome[J]. Crit Care Res Pract, 2013, 2013: 593915. DOI:10.1155/2013/593915 |
| [54] |
Zhu XW, Shi Y. Clinical settings in a preliminary study:noninvasive high-frequency oscillatory ventilation versus nasal continuous positive airway pressure in preterm infants with moderate-severe respiratory distress syndrome[J]. Pediatr Pulmonol, 2018, 53(4): 389-392. DOI:10.1002/ppul.23882 |
| [55] |
Gebeşçe A, Uslu H, Keleş E, et al. Retinopathy of prematurity:incidence, risk factors, and evaluation of screening criteria[J]. Turk J Med Sci, 2016, 46(2): 315-320. DOI:10.3906/sag-1407-127 |
 2020, Vol. 41
2020, Vol. 41