文章信息
- 梁晶晶, 胡艳, 邢艳菲, 马颖, 蒋琳, 刘慧燕, 胡芳, 卢少敏, 林穗方.
- Liang Jingjing, Hu Yan, Xing Yanfei, Ma Ying, Jiang Lin, Liu Huiyan, Hu Fang, Lu Shaomin, Lin Suifang.
- 母亲孕前体质指数及孕期增重与学龄前儿童超重肥胖的关系研究
- Association between both maternal pre-pregnancy body mass index/gestational weight gain and overweight/obesity children at preschool stage
- 中华流行病学杂志, 2019, 40(8): 976-981
- Chinese Journal of Epidemiology, 2019, 40(8): 976-981
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2019.08.019
-
文章历史
收稿日期: 2019-01-08
儿童肥胖已成为世界性公共卫生问题,且发生年龄逐渐前移[1]。其不仅影响儿童的身心健康,也会增加成人期患代谢性疾病的风险[2]。越来越多的研究显示,母亲孕期超重/肥胖和孕期营养过剩可对子代产生影响[3-4]。母亲孕期超重/肥胖和孕期营养过剩可能与子代的肥胖及代谢性疾病密切相关[5-6]。但目前关于母亲孕前BMI和孕期增重对儿童肥胖影响的研究主要集中于新生儿[7-9]和学龄期儿童,学龄前儿童研究较少[10-11],且研究结论尚不一致[12-15]。由于学龄前期是脂肪重聚期,也是儿童肥胖高发期,更是预防后期超重肥胖发生的关键期[1]。因此本研究通过对广州市学龄前儿童进行调查,分析母亲孕前BMI和孕期增重对学龄前儿童超重肥胖的影响。
对象与方法1.研究对象:来源于2016年中国9个城市<7岁儿童单纯性肥胖流行病学调查[1]。于2016年6-11月采用分层整群抽样方法在广州市抽取<7岁儿童10 018名,排除儿童体格检查、母亲孕前BMI和孕期增重等信息不完整及病理性(如甲状腺功能减退、脑垂体病等)和继发性肥胖者(如服用药物后引起的肥胖等)后,本研究最终纳入4 303名3~5岁儿童。本研究已通过广州市妇女儿童医疗中心伦理委员会批准(2017010003)。所有研究对象的监护人均签署知情同意书。
2.研究方法:
(1) 问卷调查:经过统一标准化培训的调查员现场问询逐项填写调查问卷,包括体检、一般情况、个人史及母亲孕产期情况、喂养及饮食习惯、生活习惯、父母及家庭情况等。为检验收集数据的准确性和可靠性,在问卷中采用不同的提问方式在问卷前半部分和后半部分分别设置问题收集孕期增重信息,发现两问题中母亲孕期增重信息一致率超过95%,说明本次调查结果真实可靠。
(2) 体格测量:体重、身高测量严格按照文献[1]进行。体重的读数精确至0.1 kg,身高的读数精确至0.1 cm,受试者脱鞋帽,着轻便衣进行测量,身高和体重均测量2次,取平均值,计算其BMI=体重(kg)/身高(m)2。体检人员均参加统一培训,并考核合格。测量工具统一配置,每次测量前进行校正。
(3) 诊断标准:孕前BMI定义:参照文献[16]将母亲划分为低体重(BMI<18.5 kg/m2)、适宜体重(18.5 kg/m2≤BMI≤23.9 kg/m2)、超重(24.0 kg/m2≤BMI≤27.9 kg/m2)和肥胖(BMI≥28.0 kg/m2)4组,本研究将超重和肥胖合并为超重肥胖组。
孕期增重定义:根据2009年美国医学研究所推荐的增重标准[17],该标准已被证实适合于我国孕妇[18]。具体标准:孕前低体重孕妇适宜增重范围为12.5~18.0 kg,孕前体重正常孕妇适宜增重范围为11.5~16.0 kg,孕前体重超重孕妇适宜增重范围为7.0~11.5 kg,孕前肥胖孕妇适宜增重范围为5.0~9.0 kg。依据该标准,将孕期增重分为增重不足、适宜和过度3类。
学龄前儿童超重和肥胖判定标准:依据2007年WHO推荐的生长发育标准[19],将不同性别及月龄儿童BMI高于P85界定为超重,高于P95界定为肥胖。
3.统计学分析:采用EpiData 3.0软件进行数据双录入,在录入过程中采用逻辑核查保证数据的真实性;采用SPSS 22.0软件进行统计学分析。采用方差分析和χ2检验比较不同组间相关因素的差异,采用logistic回归分析校正性别、年龄、分娩方式、6月龄内母乳喂养情况、出生胎龄、出生体重、家庭收入和母亲文化水平等因素后[6-11],分析母亲孕前BMI和孕期增重与学龄前儿童超重肥胖的关联,为排除人群特点的影响,据年龄、性别分组进行亚组分析。并进一步以儿童BMI Z值(根据WHO推荐的性别年龄别BMI参考值计算)作为因变量,采用协方差验证两者的关系;将孕前BMI分为低体重、适宜体重和超重肥胖3组,孕期增重分为不足、适宜和过度3组,分析孕前BMI合并孕期增重对子代超重肥胖的影响。以P<0.05为差异有统计学意义。
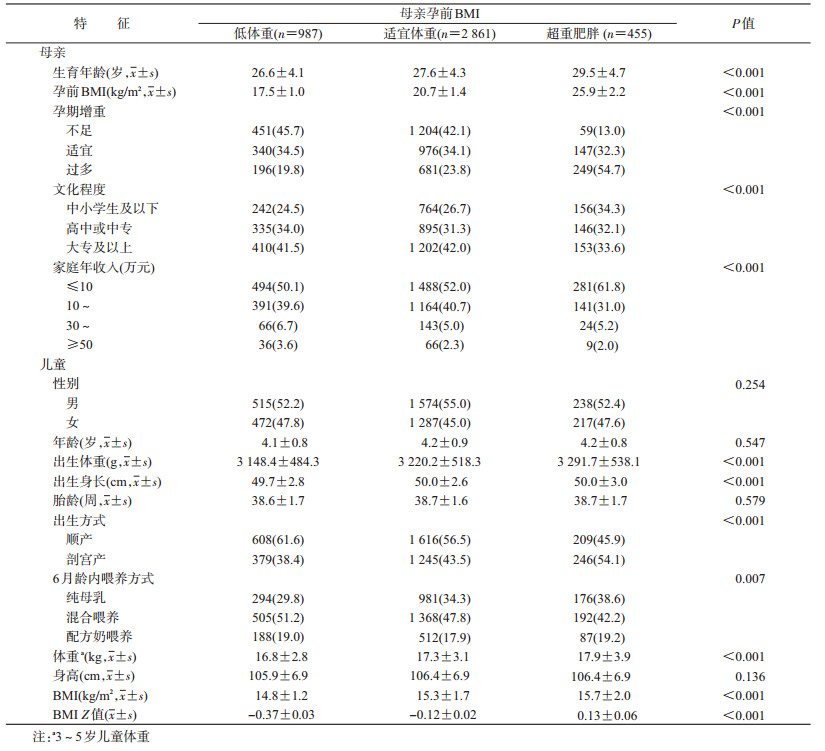
结果1.一般情况:共纳入4 303名3~5岁儿童,年龄为(4.2±0.8)岁,其中男童2 327名,女童1 976名。男童超重肥胖率为13.4%,女童超重肥胖率为8.0%。母亲孕前BMI为(20.5±2.7) kg/m2,孕前低体重987人(占22.9%),适宜体重2 861人(占66.5%),超重肥胖455人(占10.6%)。母亲孕期增重不足1 715人,增重适宜1 463人,增重过度1 125人。与孕前适宜体重者相比,孕前低体重的母亲孕期增重过多者比例较低,而孕前超重肥胖的母亲孕期增重过度者比例较高,差异有统计学意义(P<0.001)。儿童及母亲的其他基本信息见表 1。
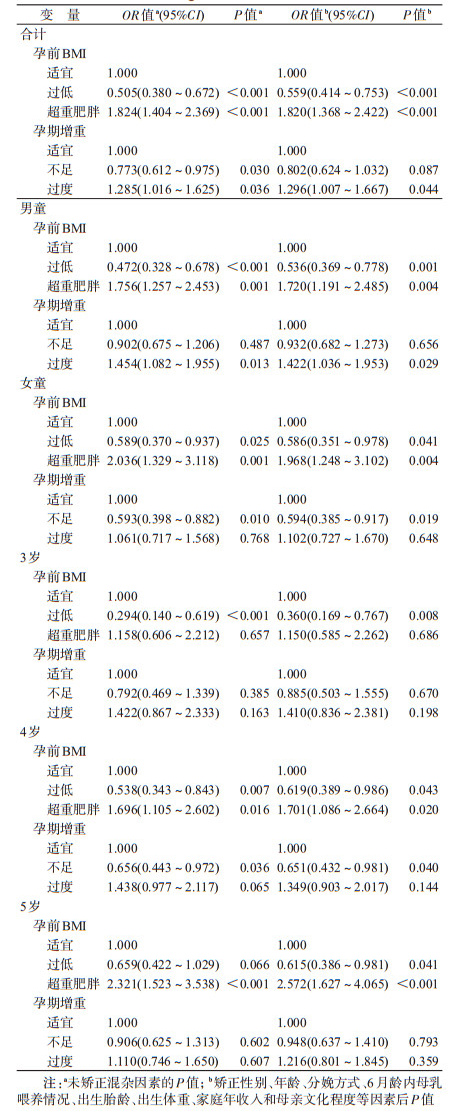
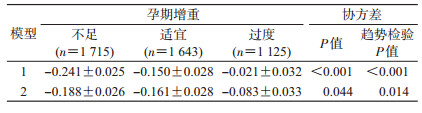
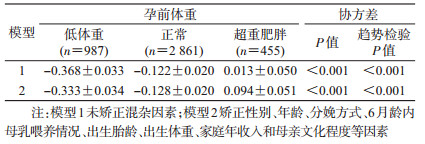
2.孕期BMI及孕期增重与学龄前儿童超重肥胖的关系:多因素logistic回归分析显示,校正性别、年龄、分娩方式、6月龄内母乳喂养情况、出生胎龄、出生体重、家庭年收入和母亲文化程度等因素后,与母亲孕前BMI适宜组相比,母亲孕前BMI过低的儿童发生超重肥胖的风险降低(OR=0.559,95% CI:0.414~0.753),但母亲孕前超重肥胖的儿童发生超重肥胖的风险增加(OR=1.820,95% CI:1.368~2.422)。与母亲孕期增重适宜的儿童相比,母亲孕期增重过度的儿童超重肥胖发生风险增加(OR=1.296,95% CI:1.007~1.667),但母亲孕期增重不足并未降低儿童超重肥胖发生的风险(P=0.087)。根据年龄、性别分组进行敏感性分析得到相似的结果(表 2)。以儿童BMI Z值作为因变量,采用协方差进一步验证了两者的关系,结果与logistic回归分析一致,母亲孕前体重超重肥胖和母亲孕期增重过度均增加儿童BMI Z值(表 3,4)。
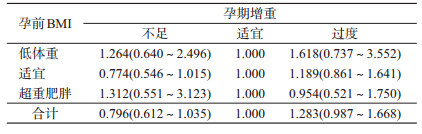
3.母亲孕前BMI合并孕期增重与学龄前儿童超重肥胖的关系:为进一步分析母亲孕前BMI合并孕期增重对学龄前儿童超重肥胖发生的影响,根据母亲孕前BMI分为3组进行分层分析,与母亲孕期增重适宜组相比,母亲孕期增重不足和过度均不增加儿童超重肥胖发生的风险(表 5)。但将两者合并后,与母亲孕前BMI适宜且孕期增重适宜组相比,母亲孕前超重肥胖且孕期增重过度组的儿童发生超重肥胖的风险增加(OR=1.574,95% CI:1.029~2.409),母亲孕前BMI过低且孕期增重不足或孕期增重适宜的儿童发生超重肥胖的风险降低(P<0.05),其他组儿童超重肥胖的发生风险差异无统计学意义(P>0.05),见表 6。
本研究结果显示,母亲孕前超重肥胖和孕期增重过度增加学龄前儿童超重肥胖的风险,与以往研究一致。回顾性调查结果显示,孕前较高的BMI和孕期增重过度是学龄前儿童超重肥胖的危险因素[10-20]。来自马鞍山出生队列的研究显示,母亲孕前超重肥胖是3~6岁学龄前儿童超重肥胖的危险因素(OR=1.92,95% CI:1.43~2.57),孕期增重过度也显著增加了学龄前儿童超重肥胖发生的风险(OR=1.47,95% CI:1.18~1.83)[11]。德国1项包含10 784名3~17岁儿童的队列研究也显示,母亲孕期增重过度增加儿童超重肥胖的风险[21]。提示孕前BMI和孕期增重过度均是影响学龄前儿童超重肥胖的重要因素。然而,也有一些研究显示了不一致的结果。Li等[15]对1 739名来自美国某出生队列的儿童从2岁追踪到12岁,显示母亲孕期增重过度(高于20.43 kg),与子代生命早期超重发生相关(OR=1.7,95% CI:1.0~2.9),但与儿童晚期超重的发生并无关联(OR=0.8,95% CI:0.3~2.1)。Crozier等[22]的研究显示,孕期增重与子代出生时脂肪含量相关,与6岁时脂肪含量呈弱相关,但与4岁时的脂肪含量无关。可能由于孕期增重主要通过出生体重间接影响后代的体重状态[23]。本研究矫正了出生体重等因素后仍显示孕期BMI和孕期增重对学龄前儿童超重肥胖的影响,提示宫内营养暴露与儿童超重肥胖密切相关。宫内营养过剩不仅很容易导致胎儿增长过度,产生巨大儿,增加儿童期超重肥胖的风险;而且可通过改变胎儿下丘脑食欲控制中枢的发育,脂肪细胞代谢,胰岛素和瘦素的分泌等途径影响胎儿能量平衡系统,使儿童更容易受到肥胖环境的影响,增加在儿童时期发生超重肥胖的风险[24-25]。遗传因素和家庭环境也在其中起着重要作用。一方面,儿童遗传母亲的肥胖易感性基因,更容易发生肥胖[26]。另一方面,超重肥胖的母亲可能具有高能量饮食,低水平体力活动等不健康的生活方式,也对儿童的生活环境造成影响,增加肥胖风险[27]。
另外,本研究结果还显示,以母亲孕前BMI正常且孕期增重适宜组作为参照组,母亲孕前超重肥胖且孕期增重过度组儿童发生超重肥胖的风险更高,与马鞍山出生队列研究结果一致[11]。但我们根据母亲孕前BMI分为3组进行分层分析时,结果却显示母亲孕期增重不足和过度均不增加儿童超重肥胖发生的风险。Lawlor等[13]和Branum等[14]也认为在母亲孕期增重过度与后代超重肥胖的关系中,只有在那些孕前超重肥胖的孕妇中孕期增重过度才与后代超重肥胖密切相关,提示母亲孕前超重肥胖较孕期增重对儿童超重肥胖的影响更大[12]。
本研究存在局限性。首先本研究是一项横断面研究,收集的产前和产后的信息为回顾性信息,可能存在回顾偏倚,对结果产生影响。但研究显示母亲对于孕期、分娩、胎龄、出生体重和母乳喂养回忆的信效度足于进行流行病学的研究[28],且本研究在问卷设计中,采用不同问题收集孕期增重情况,信息准确率超过95%,故认为收集的信息可用于本研究。其次,本研究中未考虑母亲及儿童饮食和体力活动等生活方式的影响,而家庭共享的生活方式与儿童超重肥胖的发生相关。最后,本研究人群仅来自于广州,作为经济水平较发达的地区,在某种程度上影响了结论的外推。
综上所述,母亲孕前超重肥胖和孕期增重过度均增加学龄前儿童超重肥胖的风险,且母亲孕前BMI的影响更大。随着全面二胎政策的实施,高龄产妇也越来越多,而高龄妇女较高的超重肥胖率进一步加大了这种风险。因此,应加强孕妇健康教育、合理控制孕前体重及孕期增重,以减少对子代的不良影响。
利益冲突 所有作者均声明不存在利益冲突
| [1] |
首都儿科研究所, 九市儿童体格发育调查协作组. 2016年中国九城市七岁以下儿童单纯性肥胖流行病学调查[J]. 中华儿科杂志, 2018, 56(10): 745-752. Capital Institute of Pediatrics, The Coordinating Study Group of Nine Cities on the Physical Growth and Development of Children. A national epidemiological survey on obesity of children under seven years of age in nine cities of China in 2016[J]. Chin J Pediatr, 2018, 56(10): 745-752. DOI:10.3760/cma.j.issn.0578-1310.2018.10.006 |
| [2] |
The GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years[J]. N Engl J Med, 2017, 377: 13-27. DOI:10.1056/NEJMoa1614362 |
| [3] |
van Dijk SJ, Tellam RL, Morrison JL, et al. Recent developments on the role of epigenetics in obesity and metabolic disease[J]. Clin Epigenetics, 2015, 7: 66. DOI:10.1186/s13148-015-0101-5 |
| [4] |
Kaar JL, Crume T, Brinton JT, et al. Maternal obesity, gestational weight gain, and offspring adiposity:the exploring perinatal outcomes among children study[J]. J Pediatr, 2014, 165(3): 509-515. DOI:10.1016/j.jpeds.2014.05.050 |
| [5] |
Archer E. The childhood obesity epidemic as a result of nongenetic evolution:the maternal resources hypothesis[J]. Mayo Clin Proc, 2015, 90(1): 77-92. DOI:10.1016/j.mayocp.2014.08.006 |
| [6] |
Goldstein RF, Abell SK, Ranasinha S, et al. Association of gestational weight gain with maternal and infant outcomes:a systematic review and Meta-analysis[J]. JAMA, 2017, 317(21): 2207-2225. DOI:10.1001/jama.2017.3635 |
| [7] |
Zhang WW, Niu FH, Ren XY. Association of maternal pre- pregnancy body mass index and gestational weight gain with Chinese infant growth[J]. J Paediatr Child Health, 2019, 55(6): 673-679. DOI:10.1111/jpc.14274 |
| [8] |
林友结, 蔡倩莹, 徐云云, 等. 母亲孕前体质指数和孕期体重增加及其交互作用对新生儿出生体重的影响[J]. 中华流行病学杂志, 2018, 39(6): 770-775. Lin YJ, Cai QY, Xu YY, et al. Association and interaction of pre-pregnant body mass index and gestational weight gain of women on neonatal birthweight[J]. Chin J Epidemiol, 2018, 39(6): 770-775. |
| [9] |
Zhao R, Xu L, Wu ML, et al. Maternal pre-pregnancy body mass index, gestational weight gain influence birth weight[J]. Women Birth, 2018, 31(1): e20-25. DOI:10.1016/j.wombi.2017.06.003 |
| [10] |
Wang J, Liu EQ, Wang Y, et al. Association of early pregnancy body mass index and children's birth weight with risk of being overweight in childhood[J]. Am J Hum Biol, 2018, 30(5): e23174. DOI:10.1002/ajhb.23174 |
| [11] |
邵婷.孕前BMI和孕期增重与新生儿出生体重及学龄前儿童超重肥胖关联的随访研究[D].合肥: 安徽医科大学, 2016. Shao T. Pre-pregnancy BMI and gestational weight gain: longitudinal relation with birth weight and offspring obesity[D]. Hefei: Anhui Medical University, 2016. |
| [12] |
Santos S, Monnereau C, Felix JF, et al. Maternal body mass index, gestational weight gain, and childhood abdominal, pericardial, and liver fat assessed by magnetic resonance imaging[J]. Int J Obes (Lond), 2018, 43(3): 581-593. DOI:10.1038/s41366-018-0186-y |
| [13] |
Lawlor DA, Lichtenstein P, Fraser A, et al. Does maternal weight gain in pregnancy have long-term effects on offspring adiposity?A sibling study in a prospective cohort of 146 894 men from 136 050 families[J]. Am J Clin Nutr, 2011, 94(1): 142-148. DOI:10.3945/ajcn.110.009324 |
| [14] |
Branum AM, Parker JD, Keim SA, et al. Prepregnancy body mass index and gestational weight gain in relation to child body mass index among siblings[J]. Am J Epidemiol, 2011, 174(10): 1159-1165. DOI:10.1093/aje/kwr250 |
| [15] |
Li CY, Goran MI, Kaur H, et al. Developmental trajectories of overweight during childhood:role of early life factors[J]. Obesity, 2007, 15(3): 760-771. DOI:10.1038/oby.2007.585 |
| [16] |
Chen C, Lu FC. The guidelines for prevention and control of overweight and obesity in Chinese adults[J]. Biomed Environ Sci, 2004, 17(Suppl 1): 1-36. |
| [17] |
Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines, Rasmussen KM, Yaktine AL. Weight gain during pregnancy:reexamining the guidelines[M]. Washington, DC: National Academies Press, 2009: 254.
|
| [18] |
Goldstein RF, Abell SK, Ranasinha S, et al. Gestational weight gain across continents and ethnicity:systematic review and Meta- analysis of maternal and infant outcomes in more than one million women[J]. BMC Med, 2018, 16: 153. DOI:10.1186/s12916-018-1128-1 |
| [19] |
World Health Organization. The WHO Child Growth Standards[R]. Geneva: WHO, 2015.
|
| [20] |
陈欣妍.乌鲁木齐市高新区学龄前儿童超重肥胖及其早期危险因素的调查研究[D].乌鲁木齐: 新疆医科大学, 2017. Chen XY. Investigation of overweight and obesity and its early risk factors in preschool children of high-tech zone in Urumqi[D]. Urumqi: Xinjiang Medical University, 2017. |
| [21] |
von Kries R, Ensenauer R, Beyerlein A, et al. Gestational weight gain and overweight in children:Results from the cross-sectional German KiGGS study[J]. Int J Pediatr Obes, 2011, 6(1): 45-52. DOI:10.3109/17477161003792564 |
| [22] |
Crozier SR, Inskip HM, Godfrey KM, et al. Weight gain in pregnancy and childhood body composition:findings from the Southampton Women's Survey[J]. Am J Clin Nutr, 2010, 91(6): 1745-1751. DOI:10.3945/ajcn.2009.29128 |
| [23] |
Hinkle SN, Sharma AJ, Swan DW, et al. Excess gestational weight gain is associated with child adiposity among mothers with normal and overweight prepregnancy weight status[J]. J Nutr, 2012, 142(10): 1851-1858. DOI:10.3945/jn.112.161158 |
| [24] |
Oken E, Gillman MW. Fetal origins of obesity[J]. Obes Res, 2003, 11(4): 496-506. DOI:10.1038/oby.2003.69 |
| [25] |
Bouret SG. Early life origins of obesity:role of hypothalamic programming[J]. J Pediatr Gastroenterol Nutr, 2009, 48(Suppl 1): S31-38. DOI:10.1097/MPG.0b013e3181977375 |
| [26] |
Li AH, Teo KK, Morrison KM, et al. A genetic link between prepregnancy body mass index, postpartum weight retention, and offspring weight in early childhood[J]. Obesity, 2017, 25(1): 236-243. DOI:10.1002/oby.21707 |
| [27] |
Campbell MK. Biological, environmental, and social influences on childhood obesity[J]. Pediatr Res, 2016, 79(1/2): 205-211. DOI:10.1038/pr.2015.208 |
| [28] |
Tomeo CA, Rich-Edwards JW, Michels KB, et al. Reproducibility and validity of maternal recall of pregnancy-related events[J]. Epidemiology, 1999, 10(6): 774-777. |
 2019, Vol. 40
2019, Vol. 40