文章信息
- 刘成成, 石菊芳, 刘国祥, 唐威, 张歆, 李放, 王乐, 马祎, 苏凯, 赵世俊, 高亦博, 李霓, 陈万青, 吴宁, 代敏.
- Liu Chengcheng, Shi Jufang, Liu Guoxiang, Tang Wei, Zhang Xin, Li Fang, Wang Le, Ma Yi, Su Kai, Zhao Shijun, Gao Yibo, Li Ni, Chen Wanqing, Wu Ning, Dai Min.
- 全球肺癌筛查卫生经济学研究的系统评价
- Cost-effectiveness of lung cancer screening worldwide: a systematic review
- 中华流行病学杂志, 2019, 40(2): 218-226
- Chinese Journal of Epidemiology, 2019, 40(2): 218-226
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2019.02.018
-
文章历史
收稿日期: 2018-08-24
2. 哈尔滨医科大学公共卫生学院 150086;
3. 国家癌症中心/国家肿瘤临床医学研究中心/中国医学科学院北京协和医学院肿瘤医院影像诊断科, 北京 100021;
4. 国家癌症中心/国家肿瘤临床医学研究中心/中国医学科学院北京协和医学院肿瘤医院胸外科, 北京 100021
2. School of Public Health, Harbin Medical University, Harbin 150086, China;
3. Department of Diagnostic Radiology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China;
4. Department of Thoracic Surgery, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China
肺癌已成为全球发病和死亡最高的恶性肿瘤,2018年新发和死亡病例分别为209.4万例和176.1万例[1];作为中国最为常见的恶性肿瘤,新发和死亡病例高达77.4万例和69.1万例[1],且经济负担呈现持续加重趋势[2]。通过肺癌筛查实现早发现、早诊断和早治疗是降低肺癌死亡率的有效途径。自20世纪60年代,欧、美地区率先开展肺癌筛查研究[3];其中,美国肺癌筛查试验(NLST)结果表明,与X线筛查相比,低剂量螺旋CT(LDCT)筛查可使肺癌死亡率下降20%[4]。近年来,各国政府对肺癌防控重视程度不断加大,北美、欧洲和亚洲地区的十余个国家相继开展肺癌筛查试验/项目[5]。然而,不同国家、同一国家的不同肺癌筛查项目实施方案存在差别,目标人群选择、筛查起止年龄设定和筛查技术等均存在差异[5],但何种方案更为经济有效尚不清楚[6-7]。考虑卫生资源的有限性,肺癌筛查在实施时应结合有效经济学证据,从而在全球和我国推广更大范围经济有效的肺癌筛查。因此,本研究采用系统综述的方法,全面了解全球肺癌筛查的卫生经济学评价现状、方法及主要结果,以期在全球范围内探索肺癌筛查是否经济有效,并为我国开展人群特异性的肺癌筛查卫生经济学评价研究提供方向参考。
资料与方法1.检索方法:以“肺癌”“肺肿瘤”“筛查”“普查”“成本分析”“成本效果”“成本效益”“成本效用”“卫生经济学评价”等主题词在中国知网和万方数据知识服务平台进行检索;以“lung neoplasms”“mass screening”和“economic evaluation”为MESH主题词结合“lung cancer/tumor”“screening”“cost effectiveness analysis”“cost utility analysis”“cost benefit analysis”“cost analysis”“economic evaluations”为自由词在PubMed、EMbase和The Cochrane Library进行检索;检索时限均为建库至2018年6月30日。
2.纳入和排除标准:纳入标准:①基于随机对照试验、横断面研究、队列研究、模型研究等评价肺癌筛查;②报道成本分析、成本效果分析(cost- effectiveness analysis,CEA)、成本效用分析(cost- utility analysis,CUA)或成本效益分析(cost-benefit analysis,CBA)中1种或多种结果[包括检出1例肺癌、挽救1个生命年(life year saved,LYS)、增加1个质量调整生命年(quality adjusted life year,QALY)、避免1例肺癌患者死亡/1个伤残调整生命年(disability adjusted life year,DALY)的成本]及增量成本效果比(incremental cost-effectiveness ratio,ICER)等。排除标准:①无关肺癌筛查,如药物、手术等干预研究;②非卫生经济学评价;③综述、述评等非原创性研究;④重复发表文献;⑤特定疾病人群肺癌LDCT筛查或全身性LDCT筛查;⑥全文非英文或中文。见图 1。

|
| 图 1 肺癌筛查卫生经济学研究文献(截至2018年6月30日)检索流程 |
3.信息摘录:制定文献资料提取表,内容包括①基本信息,包括作者、发表年份、研究开展年份及方法、目标人群、所评价的筛查方案;②卫生经济学评价方法学,包括评价方法、角度、成本收集范围、贴现等;③卫生经济学评价结果:挽救1个LYS、增加1个QALY、避免1例肺癌患者死亡或1个DALY的成本及ICER等。由两名研究人员独立筛选文献、提取资料并交叉核对,如遇分歧则提交小组讨论。
4.质量评价:纳入研究的质量评价采用Drummond等[8]关于卫生经济学研究评价的10条清单项目,对纳入研究参照各条目标准依次评估,每一条目均采用“是”、“否”和“不清楚”回答,并计算所有条目的报道率[是/(是+否+不清楚)]。每一条目≥85%时可认为质量较好,由两名研究人员独立开展报告质量评价,意见出现不一致时,由小组讨论决定。
5.数据处理:成本效果比=成本/效果指标,效果包括挽救1个LYS、避免1例肺癌患者死亡等;成本效用比=成本/效用指标,效用指标包括获得1个QALY和DALY;针对CEA、CUA计算ICER,ICER=(筛查组成本-对照组成本)/(筛查组效果/效用指标值-对照组效果/效用指标值)。以与空白对照组相比的ICER为评价指标,参考WHO卫生经济学评价标准[9],若ICER<人均GDP为非常经济有效;人均GDP<ICER<3倍人均GDP为经济有效;ICER>3倍人均GDP为非经济有效。本研究将纳入研究的货币统一换算为人民币,并计算ICER与当年当地人均GDP比值,作为评价筛查方案经济有效性的指标;并以该比值M(最小值~最大值)表示整体及亚组的最终结果。当年当地人均GDP及汇率均来自世界银行[10],年份与货币呈现年份一致。
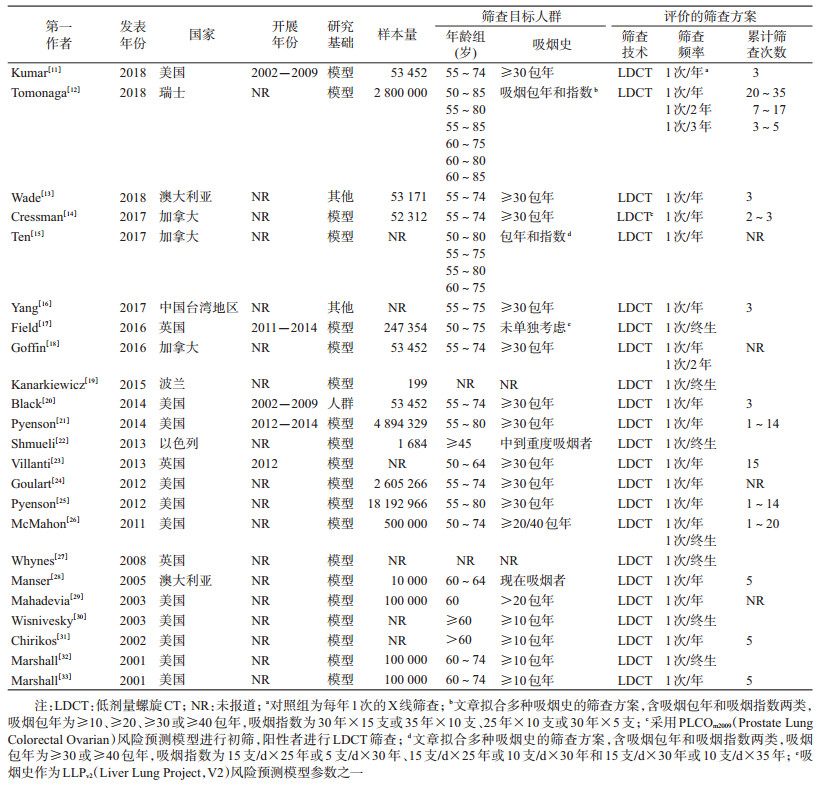
结果1.基本信息及质量评价:截至2018年6月30日,在PubMed、EMbase、The Cochrane Library、中国知网和万方数据知识服务平台进行初检共获得1 542篇文献,经去重、初筛和复筛后纳入23篇文献[11-33]。见图 1、表 1、图 2。17篇文献发表于近10年(2008-2018年)[11-27];22篇文献来自发达国家[11-15, 17-33],仅1篇文献来自中国[16]。1篇文献基于人群随机对照试验进行评价[20],20篇文献完全基于模型进行评价。Drummond等[8]关于卫生经济学研究评价的10条清单评价结果表明,纳入文献整体质量较好,其中9项条目均有报道(报道率≥85%)。

|
| 注:条目1为研究问题是否明确;条目2为各对比组描述是否全面;条目3为效果指标是否详细说明;条目4为成本和效果收集是否全面;条目5为测量成本和效果的单位是否恰当;条目6为成本和效果的收集是否可靠;条目7为是否进行贴现;条目8为是否进行增量分析;条目9为是否进行不确定性分析;条目10为结果和讨论是否涵盖全部相关问题 图 2 纳入研究质量评价 |
2.目标人群和筛查方案:在目标人群选择方面,21项研究以年龄和吸烟史选择LDCT筛查的目标人群[11-18, 20-26, 28-33],2项采用肺癌发病风险预测模型(PLCOm2009[14]和LLPV2[17])进行人群选择。筛查起始年龄以55岁居多(11项)[11-16, 18, 20-21, 24-25];吸烟史多采用吸烟包年(18项)进行量化[11-16, 18, 20-21, 23-26, 29-33],以≥30包年的研究数量最多(12项)[11-16, 18, 20-21, 23-25]。就筛查方案而言,均为组织性筛查,所评价的筛查技术均为LDCT。就筛查频率而言,每年1次(17项)[11-16, 18, 20-21, 23-26, 28-29, 31, 33]和终生1次(7项)[17, 19, 22, 26-27, 30, 32]居多,每年1次LDCT筛查中累计筛查次数以3~5次居多[11-14, 16, 20-21, 25-26, 28, 31, 33]。见表 1。
3.卫生经济学评价方法:纳入研究均明确评价方法,CEA和CUA研究各15项[11-13, 15, 18-21, 24-25, 28, 30-33]和14项[11, 13-14, 16-18, 20, 22-23, 26-29, 32]。20项研究明确评价角度,社会角度仅3项[20, 26, 29]。19项研究已进行贴现[11-16, 18-20, 22, 24, 26-33],贴现率以3%居多(15项)[11-12, 14-16, 18, 20, 22, 26-30, 32-33];15项研究同时对成本和效果进行贴现[11-16, 18, 20, 22, 26-29, 32-33];评价的时间跨度多为终生(11项)[11-12, 15-16, 20-22, 24, 26, 30]。22项研究进行敏感性分析[11-16, 18-33],方法以单因素敏感分析居多(20项)[11-13, 15-16, 18-33]。见表 2。
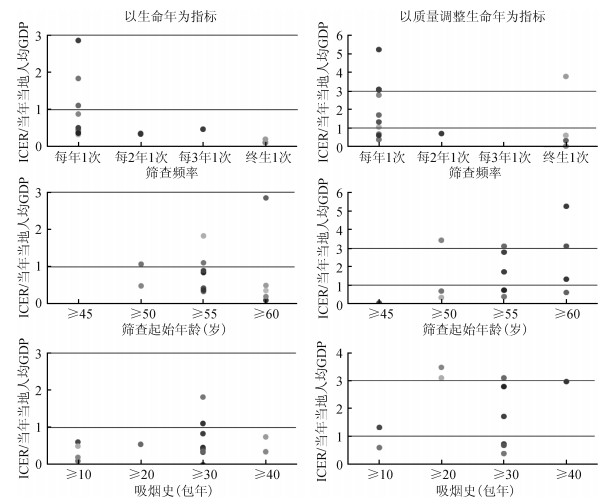
4.卫生经济学评价结果:22项研究可获得以未筛查作为对照组的ICER,其中17项研究报道的ICER值低于3倍当年当地人均GDP,是WHO认为的“经济有效”[9]。针对以未筛查作为对照组的研究进行细化分析,结果如下:就评价指标而言,12项研究报道每挽救1个LYS的成本,其ICER的M(最小值~最大值)为0.42(0.10~2.86),均为经济有效;14项研究报道每挽救1个QALY的成本,ICER值为1.19(0.04~5.24),其中10项研究为经济有效。就筛查频率而言,15项研究评价每年1次的LDCT筛查,其中12项研究报道的ICER值低于3倍当年当地人均GDP,为经济有效;ICER值(每挽救1个LYS和QALY所花费成本)与人均GDP比值分别为0.50(0.33~2.86)和1.72(0.38~5.24)。7项研究评价终生1次LDCT筛查,ICER值与人均GDP比值为0.10(0.10~0.20)和0.47(0.04~3.78),均为经济有效。且终生1次LDCT筛查的经济有效性略优于每年1次。就筛查人群起始年龄而言,5项研究针对≥50岁年龄组的人群进行评价,4项为其经济有效;ICER值与人均GDP比值分别为0.77(0.48~1.07)和0.68(0.33~3.42)。10项研究针对≥55岁年龄组人群进行评价,9项为经济有效;ICER值与人均GDP比值分别为0.63(0.33~1.83)和1.72(0.38~3.10)。7项研究针对≥60岁年龄组人群进行评价,6项为经济有效;ICER值与人均GDP比值分别为0.36(0.10~2.86)和2.21(0.60~5.24)。就筛查人群吸烟史而言,5项研究针对≥10包年吸烟史的人群进行评价,均为经济有效;ICER值与人均GDP比值分别为0.35(0.10~0.61)和0.96(0.60~1.33)。3项研究针对≥20包年吸烟史的人群进行评价,1项为经济有效;ICER值与人均GDP比值分别为0.55和3.29(3.10~3.48)。10项研究针对≥30包年吸烟史的人群进行评价,9项为经济有效;ICER值与人均GDP比值分别为0.46(0.33~1.83)和1.22(0.38~3.10)。3项研究针对≥40包年吸烟史的人群进行评价,均为经济有效;ICER值与人均GDP比值分别为0.55(0.35~0.74)和2.97。见表 2和图 3。
|
| 注:ICER为增量成本效果比 图 3 不同筛查频率、起始年龄及吸烟包年的低剂量螺旋CT肺癌筛查经济有效性 |
本研究系统评价了全球范围内肺癌筛查的卫生经济学评价研究。既往结果提示在结合年龄和吸烟史选择的肺癌高危人群中开展LDCT筛查经济有效,频率以每年1次和终生1次为主,为证据有限的欠发达地区提供了方向参考。若肺癌筛查总预算有限,可优先考虑低频率LDCT肺癌筛查,但筛查起始年龄和吸烟史等细节确定应结合人群特征进行精准评价。
Raymakers等[6]对来自美国和澳大利亚等国家的研究进行系统综述,提示不同研究间结果差异较大,肺癌LDCT筛查经济有效性尚不能判定。Puggina等[7]的纳入研究与Raymakers等[6]的纳入研究大致相同,但结果提示在国家层面实施肺癌LDCT筛查经济有效。本研究纳入研究来自美洲、欧洲及亚洲地区,覆盖人群更为广泛,且依据WHO推荐的卫生经济学评价标准[9]统一对各研究的经济有效性进行量化处理,结果提示在年龄结合吸烟史选择的肺癌高危人群中开展LDCT筛查经济有效,可为肺癌筛查实施的相关决策制定提供方向参考。
不同频次的LDCT肺癌筛查均经济有效,以每年1次和终生1次为主。但每年1次肺癌LDCT筛查累计次数较多,部分研究可高达14~20次[12, 21, 23, 25-26],需支付方持续投入大量经费,带来较重经济负担;若总预算有限,可优先考虑终生1次的低频率LDCT肺癌筛查。不同于其他癌种,肺癌筛查在人群选择层面面临更多挑战,需结合年龄和吸烟史等细节加以限定[5]。但本研究结果提示,在不同起始年龄(≥45、≥50、≥55和≥60岁)及不同吸烟包年(≥10、≥20、≥30和≥40包年)的人群中开展LDCT肺癌筛查均经济有效,但最优起始年龄和吸烟包年尚未可见,未来研究应结合人群特征进行精准评价。此外,Cressman等[14]和Field等[17]基于肺癌风险预测模型进行高危人群选择的肺癌LDCT筛查均经济有效,且ICER值远低于其他研究,分别为0.38和0.33(0.22~0.49);原因可能为风险预测模型可浓缩筛查对象,提升了肺癌LDCT筛查的经济效率,提示未来筛查项目实施时可考虑基于风险预测模型进行人群选择的肺癌LDCT筛查。
此外,本文纳入的美国研究最多,其时间脉络与政策落地有关。美国的肺癌筛查起于20世纪60年代[34],但对肺癌筛查方案的经济学评价是在2000年后逐渐增多,直到2014年11月N Engl J Med上报道了基于RCT的成本效果评价证据[20](其筛查流行病学效果——LDCT筛查可降低肺癌死亡的研究发表于更早的2011年4月[4])。在经济学证据出现3个月之后(2015年2月),美国联邦政府将每年1次的肺癌LDCT筛查纳入本国医保[35]。本研究结果初步支持肺癌LDCT筛查经济有效,能否结合我国已有肺癌筛查实践进行以人群为基础的高质量经济学评价,目前以中央政府转移支付支持为主的肺癌筛查,走向长期可持续的筹资模式[36],是更长远的课题。
目前,中国大陆地区肺癌筛查卫生经济学评价研究尚处于初级阶段,仅3项研究进行肺癌LDCT筛查的成本分析,未以挽救生命年和质量调整生命年为指标的增量成本效果进行分析[37-39]。既往研究提示,每发现1例肺癌及早期肺癌患者的费用分别为1 163 717~2 375 629元和1 745 575~2 623 090元;早期发现成本系数(EDCI=发现1例早期肺癌患者的费用/当年人均GDP)为32.02~184.4[37-39]。然而,3项研究均基于医院的体检人群进行评价,存在一定的选择偏倚;卫生经济学评价方法学有待完善,评价方法、角度及贴现等需明确;此外,研究均以EDCI作为评价指标,该指标仅可用于不同癌种之间筛查效率的优劣比较,无法判定所评价的筛查方案是否经济有效。因此,依托我国已有肺癌防控基础,参照国际可比指标,收集人群特异性数据,进行多中心现场、高精度模型的卫生经济学评价是当下的工作重点。
本研究在方法学及结果外推层面存在局限性。方法学层面,未检索经济学评价特异性数据库,存在漏检可能;其次,因篇幅所限,在吸烟史层面仅对吸烟包年进行亚组分析。结果外推层面,①纳入研究多基于欧、美地区开展,筛查项目的人群参与率、依从性及医疗资源配置与欠发达地区存在较大差异[40];②人群研究证据匮乏(仅一项研究[20]基于肺癌筛查的随机对照试验),多基于模型开展,伴随较多不确定性[8];③肺癌LDCT筛查的流行病学效果,如筛查组和未筛查组的不同分期肺癌患者占比、肺癌发病及死亡状况等,多来自美国NLST[11-14, 16, 18, 24]和SEER数据库[21, 29-30, 32-33],缺少亚洲地区人群的流行病学效果数据。即便如此,本研究对全球肺癌LDCT筛查经济学评价研究进行综述,其经济学评价研究的方法学及结果对证据匮乏的欠发达地区仍有一定借鉴意义。
综上所述,发达国家证据提示,在肺癌高危人群中开展每年1次和终生1次的LDCT肺癌筛查更倾向于经济有效。欠发达地区可结合当地卫生资源现状借鉴已有证据,预算有限时可考虑低频LDCT肺癌筛查,但筛查起始年龄和吸烟史等细节确定应结合人群特征进行精准评价。我国肺癌筛查卫生经济学评价研究尚不成熟,基于我国目前肺癌防控基础,亟待开展我国人群特异性的肺癌筛查卫生经济学评价研究,其结果对我国甚至全球肺癌防控具有重要意义。
利益冲突 所有作者均声明不存在利益冲突
| [1] |
Ferlay J, Ervik M, Lam F, et al. Global cancer observatory: cancer today. Lyon, France: international agency for research on cancer[EB/OL].[2018-09-22]. https://gco.iarc.fr/today.
|
| [2] |
Shi JF, Wang L, Wu N, et al. Clinical characteristics and medical service utilization of lung cancer in China, 2005-2014:overall design and results from a multicenter retrospective epidemiologic survey[J]. Lung Cancer, 2019, 128: 91-100. DOI:10.1016/j.lungcan.2018.11.031 |
| [3] |
Zhao SJ, Wu N. Early detection of lung cancer:low-dose computed tomography screening in China[J]. Thorac Cancer, 2015, 6(4): 385-389. DOI:10.1111/1759-7714.12253 |
| [4] |
The National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening[J]. N Engl J Med, 2011, 365(5): 395-409. DOI:10.1056/NEJMoa1102873 |
| [5] |
Pinsky PF. Lung cancer screening with low-dose CT:a world-wide view[J]. Transl Lung Cancer Res, 2018, 7(3): 234-242. DOI:10.21037/tlcr.2018.05.12 |
| [6] |
Raymakers AJN, Mayo J, Stephen L, et al. Cost-effectiveness analyses of lung cancer screening strategies using low-dose computed tomography:a systematic review[J]. Appl Health Econ Health Policy, 2016, 14(4): 409-418. DOI:10.1007/s40258-016-0226-5 |
| [7] |
Puggina A, Broumas A, Ricciardi W, et al. Cost-effectiveness of screening for lung cancer with low-dose computed tomography:a systematic literature review[J]. Eur J Public Health, 2016, 26(1): 168-175. DOI:10.1093/eurpub/ckv158 |
| [8] |
Drummond MF, Sculpher MJ, Torrance GW, et al. Methods for the Economic Evaluation of Health Care Programmes[M]. 3rd ed. Oxford: Oxford University Press, 2005.
|
| [9] |
WHO. Making Choices in Health:who Guide to Cost-Effectiveness analysis[M]. Geneva: World Health Organization, 2003.
|
| [10] |
World Bank. Official exchange rate[EB/OL].[2018-06-23]. http://www.worldbank.org/.
|
| [11] |
Kumar V, Cohen JT, van KD, et al. Risk-targeted lung cancer screening:a cost-effectiveness analysis[J]. Ann Intern Med, 2018, 168(3): 161-169. DOI:10.7326/M17-1401 |
| [12] |
Tomonaga Y, Ten HK, Frauenfelder T, et al. Cost-effectiveness of low-dose CT screening for lung cancer in a European country with high prevalence of smoking-A modelling study[J]. Lung Cancer, 2018, 121: 61-69. DOI:10.1016/j.lungcan.2018.05.008 |
| [13] |
Wade S, Weber M, Caruana M, et al. Estimating the cost-effectiveness of lung cancer screening with low-dose computed tomography for high-risk smokers in Australia[J]. J Thorac Oncol, 2018, 13(8): 1094-1105. DOI:10.1016/j.jtho.2018.04.006 |
| [14] |
Cressman S, Peacock SJ, Tammemägi MC, et al. The cost-effectiveness of high-risk lung cancer screening and drivers of program efficiency[J]. J Thorac Oncol, 2017, 12(8): 1210-1222. DOI:10.1016/j.jtho.2017.04.021 |
| [15] |
Ten HK, Tammemägi MC, Bondy SJ, et al. Performance and cost-effectiveness of computed tomography lung cancer screening scenarios in a population-based setting:a microsimulation modeling analysis in Ontario, Canada[J]. PLoS Med, 2017, 14(2): e1002225. DOI:10.1371/journal.pmed.1002225 |
| [16] |
Yang SC, Lai WW, Lin CC, et al. Cost-effectiveness of implementing computed tomography screening for lung cancer in Taiwan[J]. Lung Cancer, 2017, 108: 183-191. DOI:10.1016/j.lungcan.2017.04.001 |
| [17] |
Field JK, Duffy SW, Baldwin DR, et al. UK lung cancer RCT pilot screening trial:baseline findings from the screening arm provide evidence for the potential implementation of lung cancer screening[J]. Thorax, 2016, 71(2): 161-170. DOI:10.1136/thoraxjnl-2015-207140 |
| [18] |
Goffin JR, Flanagan WM, Miller AB, et al. Biennial lung cancer screening in canada with smoking cessation-outcomes and cost-effectiveness[J]. Lung Cancer, 2016, 101: 98-103. DOI:10.1016/j.lungcan.2016.09.013 |
| [19] |
Kanarkiewicz M, Szczńsny TJ, Krysiński J, et al. Cost-effectiveness analysis of lung cancer screening with low-dose computerised tomography of the chest in Poland[J]. Contemp Oncol, 2015, 19(6): 480-486. DOI:10.5114/wo.2015.56656 |
| [20] |
Black WC, Gareen IF, Soneji SS, et al. Cost-effectiveness of ct screening in the national lung screening trial[J]. N Engl J Med, 2014, 371(19): 1793-1802. DOI:10.1056/NEJMoa1312547 |
| [21] |
Pyenson BS, Henschke CI, Yankelevitz DF, et al. Offering lung cancer screening to high-risk medicare beneficiaries saves lives and is cost-effective:an actuarial analysis[J]. Am Health Drug Benefits, 2014, 7(5): 272-282. |
| [22] |
Shmueli A, Fraifeld S, Peretz T, et al. Cost-effectiveness of baseline low-dose computed tomography screening for lung cancer:the Israeli experience[J]. Value Health, 2013, 16(6): 922-931. DOI:10.1016/j.jval.2013.05.007 |
| [23] |
Villanti AC, Jiang YD, Abrams DB, et al. A cost-utility analysis of lung cancer screening and the additional benefits of incorporating smoking cessation interventions[J]. PLoS One, 2013, 8(8): e71379. DOI:10.1371/journal.pone.0071379 |
| [24] |
Goulart BHL, Bensink ME, Mummy DG, et al. Lung cancer screening with low-dose computed tomography:costs, national expenditures, and cost-effectiveness[J]. J Natl Compr Canc Netw, 2012, 10(2): 267-275. DOI:10.6004/jnccn.2012.0023 |
| [25] |
Pyenson BS, Sander MS, Jiang YD, et al. An actuarial analysis shows that offering lung cancer screening as an insurance benefit would save lives at relatively low cost[J]. Health Affairs, 2012, 31(4): 770-779. DOI:10.1377/hlthaff.2011.0814 |
| [26] |
McMahon PM, Kong CY, Bouzan C, et al. Cost-effectiveness of computed tomography screening for lung cancer in the United States[J]. J Thorac Oncol, 2011, 6(11): 1841-1848. DOI:10.1097/JTO.0b013e31822e59b3 |
| [27] |
Whynes DK. Could CT screening for lung cancer ever be cost effective in the United Kingdom?[J]. Cost Eff Resour Alloc, 2008, 6: 5. DOI:10.1186/1478-7547-6-5 |
| [28] |
Manser R, Dalton A, Carter R, et al. Cost-effectiveness analysis of screening for lung cancer with low dose spiral CT (computed tomography) in the Australian setting[J]. Lung Cancer, 2005, 48(2): 171-185. DOI:10.1016/j.lungcan.2004.11.001 |
| [29] |
Mahadevia PJ, Fleisher LA, Frick KD, et al. Lung cancer screening with helical computed tomography in older adult smokers:a decision and cost-effectiveness analysis[J]. JAMA, 2003, 289(3): 313-322. DOI:10.1001/jama.289.3.313 |
| [30] |
Wisnivesky JP, Mushlin AI, Sicherman N, et al. The cost-effectiveness of low-dose CT screening for lung cancer:preliminary results of baseline screening[J]. Chest, 2003, 124(2): 614-621. DOI:10.1378/chest.124.2.614 |
| [31] |
Chirikos TN, Hazelton T, Tockman M, et al. Screening for lung cancer with CT:a preliminary cost-effectiveness analysis[J]. Chest, 2002, 121(5): 1507-1514. DOI:10.1378/chest.121.5.150 |
| [32] |
Marshall D, Simpson KN, Earle CC, et al. Economic decision analysis model of screening for lung cancer[J]. Eur J Cancer, 2001, 37(14): 1759-1767. DOI:10.1016/S0959-8049(01)00205-2 |
| [33] |
Marshall D, Simpson KN, Earle CC, et al. Potential cost-effectiveness of one-time screening for lung cancer (LC) in a high risk cohort[J]. Lung Cancer, 2001, 32(3): 227-236. DOI:10.1016/S0169-5002(00)00239-7 |
| [34] |
Brett GZ. The value of lung cancer detection by six-monthly chest radiographs[J]. Thorax, 1968, 23(4): 414-420. DOI:10.1136/thx.23.4.414 |
| [35] |
The centers for medicare & medicaid services. Reminder-Beneficiary Cost-Sharing for Medicare-Covered Preventive Services Under the Affordable Care Act[EB/OL]. (2010-02-15)[2018-08-20]. http://www.doc88.com/p-747822958320.html.
|
| [36] |
徐望红, 石菊芳, 刘国祥, 等. 癌症筛查筹资的国际比较及启示[J]. 中国卫生经济, 2018, 37(7): 88-92. Xu WH, Shi JF, Liu GX, et al. International comparison and enlightenment of the financing for cancer screening[J]. Chin Health Econ, 2018, 37(7): 88-92. DOI:10.7664/CHE20180723 |
| [37] |
张春芳, 曾强, 王维民, 等. 体检人群肺癌筛查低剂量螺旋CT检出率与成本分析[J]. 中华肿瘤防治杂志, 2015, 22(4): 247-251. Zhang CF, Zeng Q, Wang WM, et al. Detection rates and cost of lung cancer screening with low-dose helical computed tomography among physical examination people[J]. Chin J Cancer Prev Treat, 2015, 22(4): 247-251. DOI:10.3969/j.issn.1005-9202.2016.16.083 |
| [38] |
房芳, 王松, 刘玉莹. 低剂量螺旋CT在中老年体检人群肺癌筛查的检出率与成本分析[J]. 中国老年学杂志, 2016, 36(16): 4042-4044. Fang F, Wang S, Liu YY. Detection rates and cost analysis of lung cancer screening with low-dose helical computed tomography among the elderly people with physical examination[J]. Chin J Gerontology, 2016, 36(16): 4042-4044. DOI:10.3969/j.issn.1005-9202.2016.16.083 |
| [39] |
严华芳, 宋晓瑛, 闵佩红. 低剂量螺旋CT对成人肺癌的临床筛选价值及成本分析[J]. 现代仪器与医疗, 2017, 23(5): 8-10. Yan HF, Song XY, Min PH. Clinical selection performance and cost analysis of lung cancer screening with low-dose helical computed tomography among adults[J]. Modern Instruments Med Treatment, 2017, 23(5): 8-10. DOI:10.11876/mimt201705004 |
| [40] |
Sivaram S, Majumdar G, Perin D, et al. Population-based cancer screening programmes in low-income and middle-income countries:regional consultation of the International Cancer Screening Network in India[J]. Lancet Oncol, 2018, 19(2): E113-122. DOI:10.1016/S1470-2045(18)30003-2 |
 2019, Vol. 40
2019, Vol. 40