文章信息
- 于冬妮, 鲜彤章, 王丽娟, 程博, 孙明晓, 郭立新.
- Yu Dongni, Xian Tongzhang, Wang Lijuan, Cheng Bo, Sun Mingxiao, Guo Lixin.
- 北京市城区858例中老年体检人群体成分和静息代谢率分析
- Analysis of body composition and resting metabolic rate of 858 middle-aged and elderly people in urban area of Beijing
- 中华流行病学杂志, 2018, 39(5): 686-688
- Chinese Journal of Epidemiology, 2018, 39(5): 686-688
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2018.05.029
-
文章历史
收稿日期: 2017-10-11
2. 100730 北京医院 营养科;
3. 100081 北京怡德医院
2. Department of Nutrition, National Center of Gerontology, Beijing Hospital, Beijing 100730, China;
3. Beijing Eden Hospital, Beijing 100081, China
生物电阻抗法(bioelectrical impedance analysis,BIA)是近年发展的一项人体成分测量技术,利用人体脂肪组织、去脂组织、体内水分等不同成分的导电性差异测定体成分的含量[1]。人体从中年期开始,组织结构和生理功能开始出现自然衰退,而身体成分的改变常被临床忽视。本研究采用BIA对健康体检中老年人群进行体成分检测,旨在了解北京市城区中老年人超重/肥胖率,探讨其体成分随年龄改变的特点。
对象与方法1.研究对象:2014年11月至2015年12月在北京医院体检的中老年人858例,年龄51~99岁,其中男性760例,女性98例。
2.研究方法:采用韩国Inbody 720人体成分分析仪直接获取研究对象体重、身高、骨骼肌、体脂肪、体脂百分比、内脏脂肪面积等数据,并在空腹(或禁食2 h)及安静状态下,采用美国森迪斯公司Vmax Encore 29n代谢车测量静息代谢率。
3.超重/肥胖判定:采用《中国成人超重和肥胖症预防控制指南》推荐的标准,即BMI 24.0~27.9 kg/m2为超重,≥28 kg/m2为肥胖[2]。
4.统计学分析:采用EpiData 3.1软件建立数据库,进行双录入和逻辑核查。利用SPSS 17.0软件进行描述性统计分析,率的比较采用χ2检验。多组均数的比较采用方差分析,组间两两比较采用LSD-t检验,P<0.05判定为差异有统计学意义。
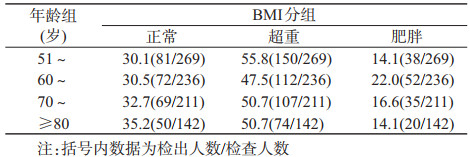
结果1.超重/肥胖率:858名中老年人BMI为16.0~36.9 kg/m2。BMI正常组272人,超重组441人,肥胖组145人。超重率为51.4%,肥胖率为16.9%。女性超重率为26.5%,肥胖率为14.3%,均明显低于男性超重率54.6%和肥胖率17.2%(P<0.001)。51~岁组超重率最高,为55.8%,60~岁组肥胖率最高,为22.0%(表 1);但不同年龄组的超重率和肥胖率的差异无统计学意义(P=0.219)。
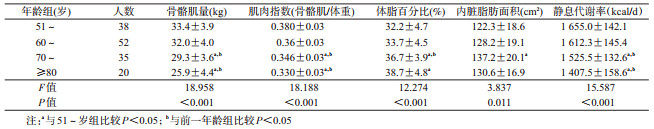
2.不同年龄组体成分和静息代谢率比较:按BMI分为正常、超重和肥胖组,不同年龄段体成分和静息代谢率测量结果见表 2~4。BMI 3个组的骨骼肌量、肌肉指数、体脂百分比、内脏脂肪面积、静息代谢率在不同年龄段的差异均有统计学意义(肥胖组各年龄段内脏脂肪面积比较P=0.011,其余均为P<0.001)。在BMI正常组,以51~岁组为对照,≥80岁组的骨骼肌量、肌肉指数、静息代谢率显著减少(P<0.05),而体脂百分比和内脏脂肪面积明显增多(P<0.05)。超重组和肥胖组中70~岁组骨骼肌量、肌肉指数、静息代谢率开始出现显著减少(P<0.05),≥80岁组减少更加显著,而70~岁组体脂百分比和内脏脂肪面积明显增多(P<0.05)。
本研究结果显示,北京市城区858名中老年体检人群超重和肥胖率分别为51.7%和16.8%,其中男性患病率明显高于女性(P<0.001)。可能与城区居民体力活动及运动较少等因素有关。
BMI仍是目前诊断超重/肥胖的主要指标[3-4]。但BMI仅涉及身高与体重,会低估老年人肌肉和脂肪的变化对疾病的影响[5]。BIA和双能X线吸收测量法(DEXA)是目前常用于体成分分析的主要方法[6]。DEXA是评价体成分的金标准,但测试费用昂贵,测试时间长;而BIA具有操作简单、成本低廉、测试速度快等优点,是一种快速、非损伤测量身体成分的方法,可用于大规模流行病学调查,且已有研究证实BIA和DEXA的检查结果相关性好[7-8]。
本研究结果显示,中老年人的骨骼肌量、肌肉指数随年龄增加而减少,可能与肌肉分解增加且合成减少有关,与国外相关研究结果一致[9-10]。由于老年人常有厌食,胃底下降松驰和胆囊收缩素增加引起的早饱、脂肪摄入量增加、瘦素水平增加、老年男性睾酮水平下降均可引起老年人厌食,导致食物摄入减少,蛋白质摄入不足,所以老年人的肌肉合成减少。同时,由于脂肪组织产生的细胞因子增加和肥胖机体的慢性低水平炎症反应,肌肉的分解增加。研究中还发现随年龄增加,中老年人基础代谢率也逐渐下降,这可能与骨骼肌丢失有关。有研究表明,少肌型肥胖患者的致残和死亡风险更高[11-13]。
本研究还发现无论是体重正常组还是超重组、肥胖组,体脂百分比均随年龄的增加而增多。与体重正常的中老年人相比,超重/肥胖人群更早出现肌肉减少和内脏脂肪增加的现象。中老年人随着年龄的增加,体力活动日趋减少,体内脂肪氧化降低导致餐后能量消耗减少,更易导致脂肪堆积。需要注意的是,肥胖组中≥80岁人群内脏脂肪面积较70~岁组并无明显变化。可能的解释是,内脏脂肪面积较大的肥胖者更易患心脑血管病、肿瘤等,其预期寿命较低;高龄老年者患消耗性疾病或营养不良疾病的可能性更大,其内脏脂肪面积甚至可能出现下降。
总之,应重视体成分和静息代谢率的检测,并根据检测指标有针对性进行个体化饮食和运动指导,达到减脂增肌的目的。
利益冲突: 无
| [1] | Lafargue AL, Cabrales LB, Larramendi RM. Bioelectrical parameters of the whole human body obtained through bioelectrical impedance analysis[J]. Bioelectromagnetics, 2002, 23(6): 450–454. DOI:10.1002/bem.10034 |
| [2] |
中国肥胖问题工作组. 中国成人超重与肥胖症预防与控制指南(节录)[J]. 营养学报, 2004, 26(1): 1–4.
China's Working Group on Obesity. Guidelines for prevention and control of overweight and obesity in Chinese adults[J]. Acta Nutr Sin, 2004, 26(1): 1–4. DOI:10.3321/j.issn:0512-7955.2004.01.001 |
| [3] |
王醴湘, 樊萌语, 余灿清, 等. 中国成年人体质指数与主要慢性病死亡风险的前瞻性研究[J]. 中华流行病学杂志, 2017, 38(2): 205–211.
Wang LX, Fan MY, Yu CQ, et al. Association between body mass index and both total and cause-specific mortality in China:findings from data through the China Kadoorie Biobank[J]. Chin J Epidemiol, 2017, 38(2): 205–211. DOI:10.3760/cma.j.issn.0254-6450.2017.02.014 |
| [4] |
中华医学会内分泌学分会肥胖学组. 中国成人肥胖症防治专家共识[J]. 中华内分泌代谢杂志, 2011, 27(9): 711–717.
Obesity group of Endocrinology Society, China Medical Association. Consensus on adult obesity prevention and control in China[J]. Chin J Endocrinol Metab, 2011, 27(9): 711–717. DOI:10.3760/cma.j.issn.1000-6699.2011.09.003 |
| [5] |
徐丹凤, 孙建琴. 老年人少肌性肥胖的研究进展[J]. 中华老年医学杂志, 2013, 32(9): 1017–1020.
Xu DF, Sun JQ. Research progress of sarcopenic obesity in older adults[J]. Chin J Geriatr, 2013, 32(9): 1017–1020. DOI:10.3760/cma.j.issn.0254-9026.2013.09.027 |
| [6] | Garvey WT, Mechanick JI, Brett EM, et al. American association of clinical endocrinologists and american college of endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity[J]. Endocr Pract, 2016, 22(Suppl 3): S1–203. DOI:10.4158/EP161365.GL |
| [7] | Bedogni G, Malavolti M, Severi S, et al. Accuracy of an eight-point tactile-electrode impedance method in the assessment of total body water[J]. Eur J Clin Nutr, 2002, 56(11): 1143–1148. DOI:10.1038/sj.ejcn.1601466 |
| [8] |
陈敏, 白慧婧, 王纯, 等. 上海地区老年人肌少症骨骼肌质量诊断标准建立和流行病学调查[J]. 中华老年医学杂志, 2015, 34(5): 483–486.
Chen M, Bai HJ, Wang C, et al. Establishment of muscle mass diagnostic standard of sarcopenia using a bioelectrical impedance analysis and epidemiological investigation of the elderly in Shanghai[J]. Chin J Geriatr, 2015, 34(5): 483–486. DOI:10.3760/cma.j.issn.0254-9026.2015.05.007 |
| [9] | Horber FF, Gruber B, Thomi F, et al. Effect of sex and age on bone mass, body composition and fuel metabolism in humans[J]. Nutrition, 1997, 13(6): 524–534. DOI:10.1016/S0899-9007(97)00031-2 |
| [10] | Beaufrère B, Morio B. Fat and protein redistribution with aging:metabolic considerations[J]. Eur J Clin Nutr, 2000, 54(Suppl 3): S48–53. DOI:10.1038/sj.ejcn.1601025 |
| [11] | Roubenoff R. Sarcopenic obesity:the confluence of two epidemics[J]. Obes Res, 2004, 12(6): 887–888. DOI:10.1038/oby.2004.107 |
| [12] | Baumgartner RN, Wayne SJ, Waters DL, et al. Sarcopenic obesity predicts instrumental activities of daily living disability in the elderly[J]. Obes Res, 2004, 12(12): 1995–2004. DOI:10.1038/oby.2004.250 |
| [13] | Scott D, Sanders KM, Aitken D, et al. Sarcopenic obesity and dynapenic obesity:5-year associations with falls risk in middle-aged and older adults[J]. Obesity, 2014, 22(6): 1568–1574. DOI:10.1002/oby.20734 |
 2018, Vol. 39
2018, Vol. 39