文章信息
- 王红, 汤颖, 张宇, 许科, 赵景波.
- Wang Hong, Tang Ying, Zhang Yu, Xu Ke, Zhao Jingbo.
- 急性缺血性脑卒中患者入院24小时血压波动最大值对预后的影响
- Effect of maximum blood pressure fluctuation on prognosis of patients with acute ischemic stroke within 24 hours after hospital admission
- 中华流行病学杂志, 2018, 39(5): 682-685
- Chinese Journal of Epidemiology, 2018, 39(5): 682-685
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2018.05.028
-
文章历史
收稿日期: 2017-10-17
2. 150081 哈尔滨医科大学附属第一临床医学院神经内科
2. Department of Neurology, The First Affiliated Hospital, Harbin Medical University, Harbin 150081, China
高血压是急性脑卒中的主要原因。临床上急性期缺血性脑卒中患者入院时80%以上存在血压升高[1-2],且血压水平与其预后相关[3-6]。目前少有对入院时血压按照高血压诊断标准将患者分为正常血压组与高血压组[7],观察24 h动态血压波动最大值与预后关系的对比性研究。为此,本研究监测急性缺血性脑卒中患者入院24 h内血压动态,出院时进行美国国立卫生研究院卒中量表(NIHSS)评分,探讨急性缺血性脑卒中入院时为高血压患者和正常者,其24 h内血压波动最大值对不良预后的影响。
对象与方法1.研究对象:2016年4月至2017年3月在哈尔滨医科大学附属第一医院急诊神经内科连续纳入急性缺血性脑卒中患者。纳入标准:发病24 h内入院,经头颅CT或MRI确诊为急性缺血性脑卒中,并自愿签署知情同意书。排除标准:本次发病前Modified Rankin Scale(MRS)评分≥3;血压监测数据不足24 h者;住院期间死亡;有先天性疾病,或患有心、脑、消化、血液等系统严重疾病,或有精神疾病史者。
2.研究方法:
(1)入院时检查:采用床旁监护仪(日本光电工业株式会社BSM-6701C)测量患者入院24 h内动态血压,每2 h测一次,并记录血压观测值。采用与家属面对面问答方式收集患者性别、年龄、文化程度、体力活动程度等基本人口学资料,以及既往病史(高血压、冠心病、糖尿病、房颤、脑卒中)和行为因素(吸烟和饮酒)数据。测量身体指标(体重、身高),收集临床检验指标(TC、TG、HDL-C、LDL-C、FPG、同型半胱氨酸)。
(2)出院预后评价:出院时采用NIHSS评分,<5为预后良好,≥5为预后不良[8]。
3.统计学分析:采用SAS 9.4软件。计量资料之间比较用t检验,计数资料之间比较用χ2检验。单因素和调整后因素的分析采用非条件logistic回归分析。计算OR值及其95%CI,以P<0.05为差异有统计学意义。
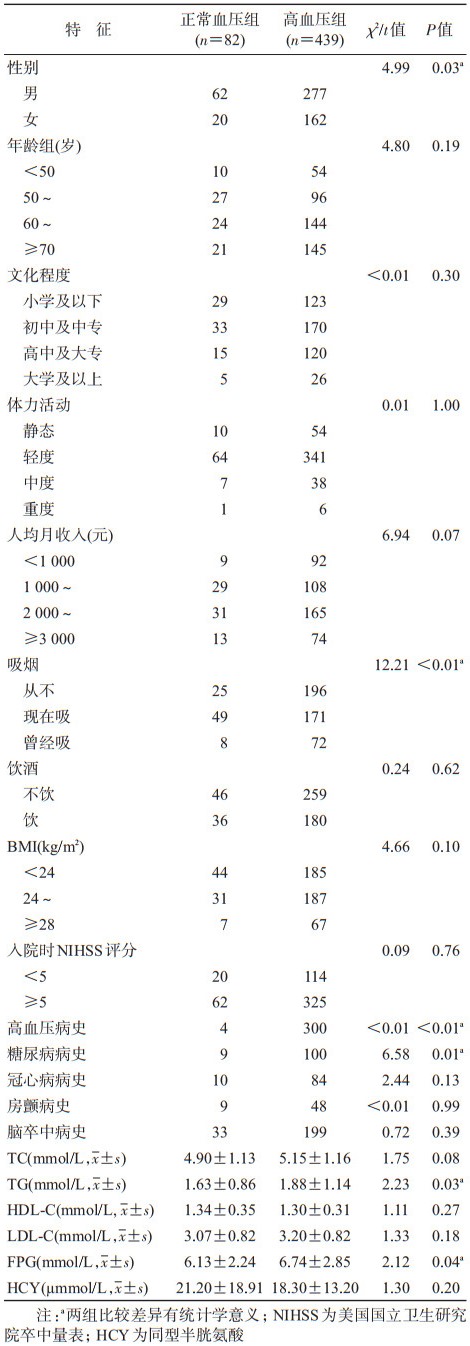
结果1.基本情况:研究期间共收集524例急性缺血性脑卒中,剔除3例低血压,实际纳入521例。根据入院时血压水平和高血压诊断标准[7],将患者分为正常血压组82例和高血压组439例。正常血压组年龄(62±12)岁,男性62例(75.61%);高血压组年龄(64±12)岁,男性277例(63.10%)。见表 1。
2.入院24 h内血压波动最大值:以两组患者入院24 h内动态血压最大值为分析指标,包括收缩压最大值(SBP max)和舒张压最大值(DBP max)。
正常血压组SBP max的均值、标准差和中位数分别为146.6、20.4、146.5 mmHg(1 mmHg=0.133 kPa)(正态性检验:W=0.97,P=0.101 6);DBP max分别为90.0、13.0、89.5 mmHg(正态性检验;W=0.99,P=0.838 2)。高血压组SBP max的均值、标准差和中位数分别为173.8、23.3、171.0 mmHg(正态性检验:W=0.98,P<0.000 1);DBP max分别为100.1、15.5、98.0 mmHg(正态性检验:W=0.98,P<0.000 1)。
3.入院24 h内血压波动最大值与出院预后的关系:
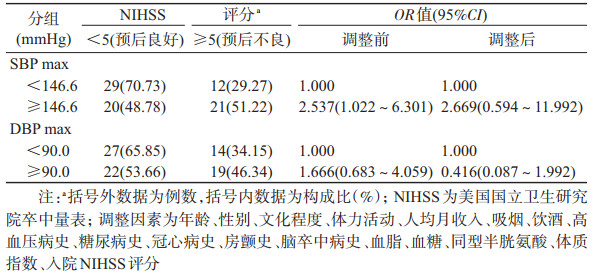
(1)正常血压组:由于24 h的SBP max和DBP max均服从正态分布(均P>0.05),以SBP max均值146.6 mmHg为界和DBP max均值90.0 mmHg为界进行分组。以SBP max<146.6 mmHg为基准,调整年龄、性别、文化程度、体力活动、人均月收入、吸烟、饮酒、高血压病史、糖尿病史、冠心病史、房颤史、脑卒中病史、血脂、血糖、同型半胱氨酸、BMI、入院NIHSS评分等因素后,SBP max≥146.6 mmHg与出院预后不良的OR值(95%CI)为2.669(0.594~11.992)。以DBP max<90.0 mmHg为基准,调整上述因素后,DBP max ≥90.0 mmHg与出院预后不良的OR值(95%CI)为0.416(0.087~1.992),见表 2。
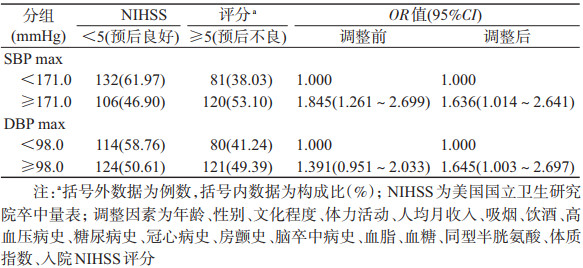
(2)高血压组:由于24 h的SBP max和DBP max均不服从正态分布(均P<0.05),以SBP max中位数171.0 mmHg为界和DBP max中位数98.0 mmHg为界进行分组。以SBP max<171.0 mmHg为基准,调整上述因素后,SBP max≥171.0 mmHg与出院预后不良的OR值(95%CI)为1.636(1.014~2.641);以DBP max<98.0 mmHg为基准,调整上述因素后,DBP max≥98.0 mmHg与出院预后不良的OR值(95%CI)为1.645(1.003~2.697),见表 3。
本研究急性缺血性脑卒中患者中,有83.78%在入院时血压超过高血压诊断标准,与文献报道一致[2]。Buratti等[9]分析89例伴有颈内动脉闭塞的缺血性脑卒中患者发病48 h内的血压,发现SBP和DBPmax、极值、标准差和变异系数在3个月预后良好和预后不良组的差异有统计学意义(均P<0.05),证实伴有颈内动脉闭塞的缺血性脑卒中患者急性期血压最大值与临床不良预后相关,但血压测量采用的是标准水银血压计,而未采用血压监护仪自动监测血压。挪威学者研究了127例溶栓治疗的急性缺血性脑卒中患者,分析溶栓前血压和溶栓后24 h血压波动最大值与3个月预后的关系,发现溶栓前、后SBP升高可增加预后不良的风险,即每升高10 mmHg,OR值(95%CI)分别为1.27(1.03~1.52)、1.22(1.00~1.44);而溶栓前、后的DBP升高未增加预后不良风险,即每升高10 mmHg,OR值(95%CI)分别为1.03(0.97~1.36)、1.16(0.99~1.46)[10]。2017年希腊研究者针对217例急性缺血性脑卒中伴有大血管闭塞的患者,观察机械取栓后的血压水平对早期预后影响,发现术后24 h的SBP max每增加10 mmHg,其3个月死亡风险越大,OR值(95%CI)为1.49(1.18~1.88),而DBP max增加10 mmHg,并未增大3个月死亡的风险,OR值(95%CI)为1.26(0.94~1.69)[11]。韩国一项涉及1 161例缺血性脑卒中患者发病后72 h血压变异与早期神经功能恶化关系的研究,发现SBP均值、最小值、最大值及DBP max均与早期神经恶化独立相关,调整潜在的混杂因素后,血压变异参数每增加1个标准差,早期神经功能恶化的风险增加14%~21%[12]。
本课题组前期研究中,观察急性期缺血性脑卒中患者住院6 d血压波动最大值与出院预后的关系[13],认为与SBP max(140~159 mmHg)相比,160~179 mmHg和≥180 mmHg均增加了出院预后不良的风险,OR值(95%CI)为2.51(1.30~4.85)及2.68(1.27~5.65)。与DBP max(<90 mmHg)相比,100~109 mmHg和≥110 mmHg均增加了出院预后不良的风险,OR值(95%CI)为1.92(1.00~3.67)及2.78(1.35~5.69)。明确了缺血性脑卒中急性期入院血压波动最大值是预后不良的一个预测因素。
本研究存在不足。如研究对象均来自同一医院,存在选择性偏倚;血压对缺血性脑卒中预后的影响还取决于脑卒中分型;由于正常血压组的样本量较少,经分组后分析得出的结果仍需要大样本加以验证。
总之,本研究结果提示急性缺血性脑卒中患者入院时存在高血压,其SBP和DBP波动最大值均与出院预后不良有关。可见入院时血压水平是临床关注点,尤其入院时血压水平超过诊断标准者,更需要密切关注血压波动的最大值。
利益冲突: 无
| [1] | Willmot M, Leonardibee J, Bath PM. High blood pressure in acute stroke and subsequent outcome:a systematic review[J]. Hypertension, 2004, 43(1): 18–24. DOI:10.1161/01.HYP.0000105052.65787.35 |
| [2] | Tikhonoff V. Blood pressure as a prognostic factor after acute stroke[J]. Lancet Neurol, 2009, 8(10): 938–948. DOI:10.1016/S1474-4422(09)70184-X |
| [3] | Mustanoja S, Putaala J, Gordin D, et al. Acute-phase blood pressure levels correlate with a high risk of recurrent strokes in young-onset ischemic stroke[J]. Stroke, 2016, 47(6): 1593–1598. DOI:10.1161/STROKEAHA.116.012944 |
| [4] | Maïer B, Gory B, Taylor G, et al. Mortality and disability according to baseline blood pressure in acute ischemic stroke patients treated by thrombectomy:a collaborative pooled analysis[J]. J Am Heart Assoc, 2017, 6(10): e006484. DOI:10.1161/JAHA.117.006484 |
| [5] | Kakaletsis N, Ntaios G, Milionis H, et al. Prognostic value of 24-h ABPM in acute ischemic stroke for short-, medium-, and long-term outcome:a systematic review and meta-analysis[J]. Int J Stroke, 2015, 10(7): 1000–1007. DOI:10.1111/ijs.12609 |
| [6] | Ritter MA, Kimmeyer P, Heuschmann PU, et al. Blood pressure threshold violations in the first 24 hours after admission for acute stroke:frequency, timing, predictors, and impact on clinical outcome[J]. Stroke, 2009, 40(2): 462–468. DOI:10.1161/STROKEAHA.108.521922 |
| [7] |
中国高血压防治指南修订委员会. 中国高血压防治指南2010[J]. 中华高血压杂志, 2011, 19(8): 701–742.
Writing Group of Chinese Guidelines for the Management of Hypertension. 2010 Chinese guidelines for the management of hypertension[J]. Chin J Hyperten, 2011, 19(8): 701–742. DOI:10.16439/j.cnki.1673-7245.2011.08.009 |
| [8] | Ruuskanen EI, Laihosalo M, Kettunen J, et al. Predictors of discharge to home after thrombolytic treatment in right hemisphere infarct patients[J]. J Cen Nerv Sym Dis, 2010, 2(2): 73–79. DOI:10.4137/JCNSD.S6411 |
| [9] | Buratti L, Cagnetti C, Balucani C, et al. Blood pressure variability and stroke outcome in patients with internal carotid artery occlusion[J]. J Neurol Sci, 2014, 339(1-2): 164–168. DOI:10.1016/j.jns.2014.02.007 |
| [10] | Idicula TT, Waje-Andreassen U, Brogger J, et al. The effect of physiologic derangement in patients with stroke treated with thrombolysis[J]. J Stroke Cerebrovasc Dis, 2008, 17(3): 141–146. DOI:10.1016/j.jstrokecerebrovasdis.2008.01.010 |
| [11] | Goyal N, Tsivgoulis G, Pandhi A, et al. Blood pressure levels post mechanical thrombectomy and outcomes in large vessel occlusion strokes[J]. Neurology, 2017, 89(6): 540–547. DOI:10.1212/WNL.0000000000004184 |
| [12] | Chung JW, Kim N, Kang J, et al. Blood pressure variability and the development of early neurological deterioration following acute ischemic stroke[J]. J Hyperten, 2015, 33(10): 2099–2106. DOI:10.1097/HJH.0000000000000675 |
| [13] |
杨晓珊, 王宁宁, 张洪召, 等. 缺血性脑卒中患者急性期血压最大值与预后关系的研究[J]. 中华流行病学杂志, 2015, 36(6): 649–652.
Yang XS, Wang NN, Zhang HZ, et al. Effect of maximum blood pressure when discharged from the hospital on the prognosis among patients with acute ischemic stroke[J]. Chin J Epidemiol, 2015, 36(6): 649–652. DOI:10.3760/cma.j.issn.0254-6450.2015.06.024 |
 2018, Vol. 39
2018, Vol. 39