文章信息
- 宋艺, 万李, 陈双双, 徐永娟, 刘志广, 赵秀芹, 刘海灿, 吴移谋, 万康林, 管茶香, 刘民.
- Song Yi, Wan Li, Chen Shuangshuang, Xu Yongjuan, Liu Zhiguang, Zhao Xiuqin, Liu Haican, Wu Yimou, Wan Kanglin, Guan Chaxiang, Liu Min.
- 中国6个省份结核分枝杆菌耐药状况及影响因素分析
- Analysis on drug resistance of Mycobacterium tuberculosis and influencing factors in six provinces of China
- 中华流行病学杂志, 2016, 37(7): 945-948
- Chinese Journal of Epidemiology, 2016, 37(7): 945-948
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2016.07.008
-
文章历史
- 投稿日期: 2015-11-09
2. 410000 长沙, 中南大学湘雅医学院生理学系;
3. 102206 北京, 中国疾病预防控制中心传染病预防控制所 传染病预防控制国家重点实验室 传染病诊治协同创新中心;
4. 421000 衡阳, 南华大学病原生物学研究所
2. Department of Physiology, Xiangya Medical School, Central South University, Changsha 410000, China;
3. State Key Laboratory of Communicable Disease Prevention and Control, Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, Institute for Communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing 102206, China;
4. Institute of Pathogenic Biology, University of South China, Hengyang 421000, China
结核病现今仍是严重威胁全球卫生安全的重要传染病之一[1, 2]。我国是世界结核病高负担国家,新发活动性肺结核病例数居全球第二位,耐多药结核病(MDR-TB)发病率居世界第三位[3]。在过去10年我国结核病患病率虽有所下降,但耐药结核病的比例却逐渐增加,特别是MDR-TB增加明显[4, 5]。耐药结核病的流行会严重影响其控制效果,因此对耐药结核病的研究有非常重要的意义。
材料与方法1. 试验菌株:从中国CDC传染病预防控制所结核病实验室菌株库中,分别选取国内6省份源于2004-2006年分离自病例的结核分枝杆菌药物敏感性试验结果及其病历资料。结核分枝杆菌共计999株,其中北京107株,吉林343株,新疆205株,陕西144株,湖南102株,河南98株。
2. 研究方法:
(1)病例调查:采用问卷调查方法,调查问卷在查阅文献的基础上结合实际情况制定,内容包括一般人口学信息、病例类型、治疗史、并发症等。调查员由调查地区经过专业培训的省级结核病医院或结核防治所结核病防治人员和医务人员等组成。
(2)菌株鉴定和药物敏感试验:分离菌株标本均由中国CDC传染病预防控制所结核病实验室负责,采用PNB/TCH鉴别培养基和基于改良罗氏固体培养基的比例法分别进行菌种鉴定和4种一线抗结核药物[异烟肼(INH)、利福平(RFP)、链霉素(SM)、乙胺丁醇(EMB)]的药物敏感试验。4种药物培养基内含药浓度分别为0.2、40、4和2 μg/ml[6]。
3. 统计学分析:应用Excel 2003软件整理数据,并建立数据库。SPSS 20.0软件进行统计学分析,计数资料采用 χ2检验,P<0.05为差异有统计学意义。
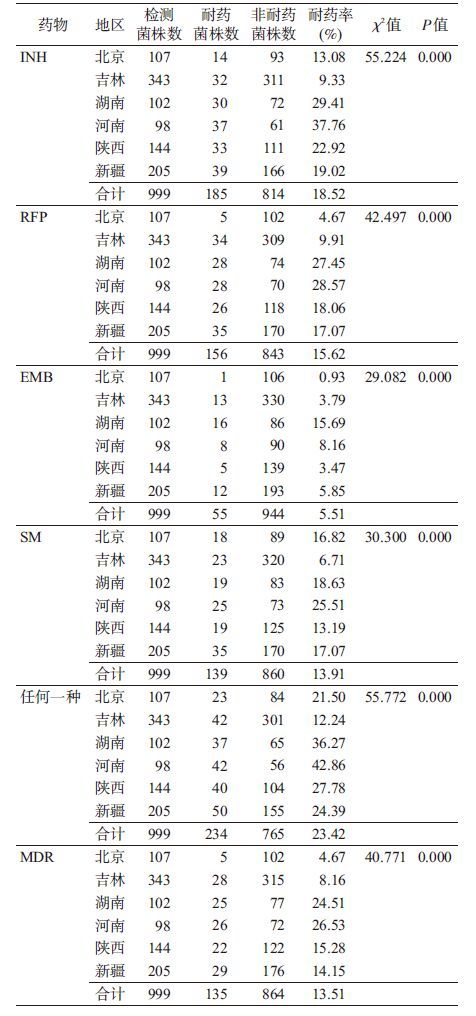
结 果1. 菌株耐药性检测: 结果显示(表1),分离自6省份999株结核分枝杆菌总体耐药率和耐多药(MDR)率分别为23.42%和13.51%。分离自北京、吉林、湖南、河南、陕西、新疆的菌株耐药率分别21.50%、12.24%、36.27%、42.86%、27.78%、24.39%,MDR率分别为4.67%、8.16%、24.51%、26.53%、15.28%、14.15%,各省份菌株单种药物耐药率、总体耐药率和MDR率差异均有统计学意义(P=0.000)。
2. 单因素分析:
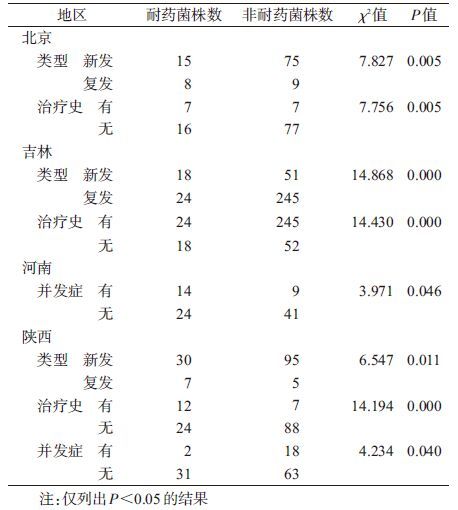
(1)耐药影响因素:选取结核病患者性别、年龄、病例类型、治疗史、并发症5个因素进行分析(表2)。北京和吉林的结核病患者新发、复发类型及有无治疗史与耐药结核病有明显相关性,结果有统计学意义(P<0.05);河南的结核病患者有无并发症与耐药结核病有明显相关性,结果有统计学意义(P<0.05);陕西的结核病患者新发、复发类型,有无治疗史及有无并发症与耐药结核病有明显相关性,结果有统计学意义(P<0.05);而湖南和新疆的结核病患者上述耐药影响因素的单因素分析结果均无统计学意义(P>0.05)。
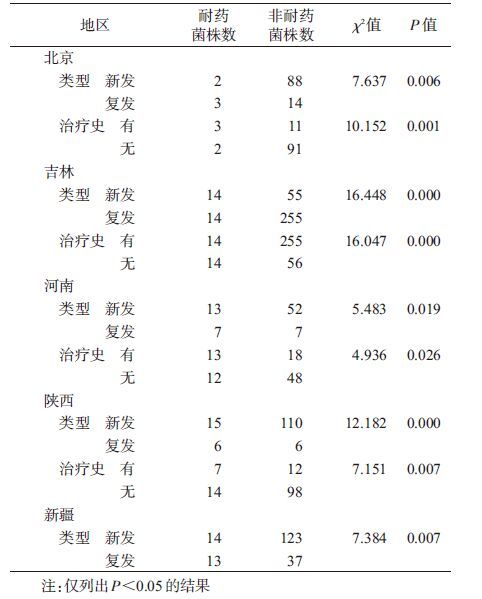
(2)MDR影响因素:选取相同的5个影响因素,分析结果显示北京、吉林、河南和陕西结核病患者新发、复发类型及有无治疗史与MDR-TB有明显相关性,结果有统计学意义(P<0.05);新疆结核病患者新发、复发类型与MDR-TB有明显相关性,结果有统计学意义(P<0.05);湖南结核病患者单因素分析结果无统计学意义(P>0.05)。见表3。
本研究参考我国耐药结核病相关危险因素的研究结果,对北京等6省份分离自病例的结核分枝杆菌耐药率及因素进行分析。结果显示,各省份分离的菌株之间无论是单种药物耐药率、总体耐药率,还是MDR率的差异均有统计学意义(P<0.05)。影响菌株耐药的单因素分析显示,不同省份菌株耐药及产生MDR-TB的影响因素不同,同文献报道一致[7]。除地理位置、气候条件、社会经济和文化等影响耐药性的因素外,还包括新发、复发病例类型和有无治疗史[3, 8]。结合文献研究结果[9, 10, 11, 12, 13, 14],提示上述影响因素对耐药及MDR-TB的产生有着非常重要的意义。
目前普遍认为“治疗史”是结核分枝杆菌产生耐药性的危险因素之一[9, 10, 11, 12, 13, 14],本研究分析结果显示该因素与耐药或MDR-TB的产生具有明显的相关性(P<0.05)。由于结核病治疗时间至少需要6个月,这使结核分枝杆菌有足够的时间和机会产生耐药性。本文分析还显示,河南、陕西结核病患者有无并发症与耐药结核病的产生有关,但结核病的并发症较多,因此具体判断哪些并发症可能产生影响还有待进一步分析。
综上所述,我国结核病耐药状况依旧严峻,不同地区结核分枝杆菌产生耐药的影响因素存在差异,因此对耐药结核病的预防控制必须针对不同的危险因素采取相应措施,以此取得更好的预防控制效果。
利益冲突 无
| [1] WHO. Global tuberculosis report,2015[EB/OL].[2015-10-30]. http://apps.who.int/iris/bitstream/I0665/191102/9789241565059-eng.pdf?ua=1. |
| [2] Goldberg DE,Siliciano RF,Jacobs WR Jr. Outwitting evolution:fighting drug-resistant TB,malaria,and HIV[J]. Cell,2012,148(6):1271-1283. DOI:10.1016/j.cell.2012.02.021. |
| [3] WHO. Multidrug and extensively drug-resistant TB (M/XDR-TB):2010 global report on surveillance and response[R]. Geneva:WHO,2010. |
| [4] Chiang CY,Centis R,Migliori GB. Drug-resistant tuberculosis:past,present,future[J]. Respirology,2010,15(3):413-432. DOI:10.1111/j.1440-1843.2010.01738.x. |
| [5] Akachi Y,Zumla A,Atun R. Investing in improved performance of national tuberculosis programs reduces the tuberculosis burden:analysis of 22 high-burden countries,2002-2009[J]. J Infect Dis,2012,205 Suppl 2:S284-292. DOI:10.1093/infdis/jis189. |
| [6] 陈明亭,万康林. 结核病实验室技术手册[M]. 北京:科学出版社,2011. Chen MT,Wan KL. The technical manual of tuberculosis laboratory[M]. Beijing:Science Press,2011. |
| [7] Zhao YL,Xu SF,Wang LX,et al. National survey of drug-resistant tuberculosis in China[J]. N Engl J Med,2012,366(23):2161-2170. DOI:10.1056/NEJMoa1108789. |
| [8] He GX,Zhao YL,Jiang GL,et al. Prevalence of tuberculosis drug resistance in 10 provinces of China[J]. BMC Infect Dis,2008,8(1):166. DOI:10.1186/1471-2334-8-166. |
| [9] Espinal MA,Laserson K,Camacho M,et al. Determinants of drug-resistant tuberculosis:analysis of 11 countries[J]. Int J Tuberc Lung Dis,2001,5(10):887-893. |
| [10] Lomtadze N,Aspindzelashvili R,Janjgava M,et al. Prevalence and risk factors for multidrug-resistant tuberculosis in the Republic of Georgia:a population-based study[J]. Int J Tuberc Lung Dis,2009,13(1):68-73. |
| [11] Aguiar F,Vieira MA,Staviack A,et al. Prevalence of anti-tuberculosis drug resistance in an HIV/AIDS reference hospital in Rio de Janeiro,Brazil[J]. Int J Tuberc Lung Dis,2009,13(1):54-61. |
| [12] Clark CM,Li J,Driver CR,et al. Risk factors for drug-resistant tuberculosis among non-US-born persons in New York city[J]. Int J Tuberc Lung Dis,2005,9(9):964-969. |
| [13] Boonsarngsuk V,Tansirichaiya K,Kiatboonsri S. Thai drug-resistant tuberculosis predictive scores[J]. Singapore Med J,2009,50(4):378-384. |
| [14] Kliiman K,Altraja A. Predictors of extensively drug-resistant pulmonary tuberculosis[J]. Ann Intern Med,2009,150(11):766-775. DOI:10.7326/0003-4819-150-11-200906020-00004. |
 2016, Vol. 37
2016, Vol. 37