文章信息
- 姜帆, 李素云, 潘璐璐, 王强, 杨孝荣, 张楠, 李慧杰, 韩明奎, 贾崇奇.
- Jiang Fan, Li Suyun, Pan Lulu, Wang Qiang, Yang Xiaorong, Zhang Nan, Li Huijie, Han Mingkui, Jia Chongqi.
- 拒烟自我效能在吸烟危害认知对戒烟成功影响的中介效应分析
- Mediating effect of smoking abstinence self-efficacy on association between awareness of smoking hazard and successful smoking cessation
- 中华流行病学杂志, 2015, 36(10): 1081-1084
- Chinese Journal of Epidemiology, 2015, 36(10): 1081-1084
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2015.10.010
-
文章历史
- 投稿日期: 2015-02-10
烟草应用是目前导致全球可预防死亡的首要死因。我国烟草应用状况十分严峻[1]。特别是农村居民吸烟率和吸烟量均明显高于城市人群[2]。因此在农村地区开展有效的控烟工作迫在眉睫。其中促使吸烟者戒烟是主要控烟策略之一[3]。戒烟是否成功受诸多因素如年龄、婚姻状况、职业、教育程度等影响[4, 5]。 研究表明,吸烟危害认知显著影响吸烟行为,表现为吸烟危害认知水平高者更倾向于戒烟[6],且其戒烟成功的可能性更大[3]。而拒烟自我效能也是影响戒烟成功的重要因素[7, 8],即表现为拒烟自我效能越高,戒烟成功的可能性越大。有研究显示,吸烟危害认知对拒烟自我效能具有正面效应[9]。然而,目前国内外鲜见有关拒烟自我效能在吸烟危害认知中对戒烟成功影响及其程度的研究。为此,本研究假定:①吸烟危害认知水平高者更容易戒烟成功;②吸烟危害认知水平高者拒烟自我效能也高;③拒烟自我效能在吸烟危害认知对戒烟成功的影响中具有中介效应。并据此建立中介效应分析模型,探讨拒烟自我效能在吸烟危害认知对戒烟成功中的中介效应及其程度,为制定控烟干预措施提供理论依据。 对象与方法
1. 研究对象:2013年4-5月以Global adult tobacco survey(GATS) core questionnaire with optional questions[10]为基础设计调查表,在济南市平阴县、临沂市莒南县、济宁市梁山县17个行政村18岁及以上男性人群中,选择曾经戒烟者,由经培训的调查员逐一入户,采用面对面方式进行调查,共得有效问卷1 429份,其中596份现在吸烟者(包括509份现在每日吸烟者及87份现在偶尔吸烟者)及833份戒烟者。本次分析排除现在偶尔吸烟者,采用以社区人群为基础的病例对照研究,以642例自发性戒烟成功者(833例戒烟者减去191例戒烟失败者)为病例组,以700例自发性戒烟失败者(包括现在每日吸烟者509例及戒烟失败者191例)为对照组。本研究通过了山东大学伦理审查委员会批准,并向所有受试者提供了知情同意书。
2. 标准和定义:根据WHO有关吸烟的定义[11]。吸烟者指一生中累计吸烟≥100支(或等量烟草)者;现在吸烟者指达到吸烟者标准,且在调查时仍在吸烟;现在每日吸烟者指达到吸烟者标准,且在调查时每天至少吸1支烟者;现在偶尔吸烟者指达到吸烟者标准,调查时吸烟,但非每天吸烟者;戒烟者指达到吸烟者标准,但调查时已不再吸烟者;戒烟成功者指达到吸烟者标准,但调查时已连续不再吸烟≥2年者[12];戒烟失败者指达到吸烟标准,曾经戒过烟但又复吸,或调查时已连续不再吸烟<2年者。
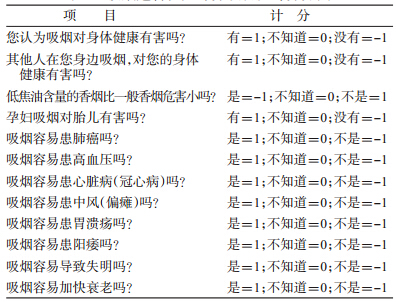
3. 测量方法:吸烟危害认知评分项目及计分方法见表 1,各项目计分合计为认知总分,分数越高,危害认知水平越高。建立中介效应分析模型(图 1)。其中拒烟自我效能调查采用Velicer等设计的拒烟自我效能量表(Smoking Abstinence Self- Efficacy),该量表包含9个条目,分为3个情境维度,分别是积极情境(positive/social situations)、消极情景(negative/affective situations)及习惯情境(habit/addictive situations)。量表每个条目按5点李克特量表等级评分,从“极其想吸”评分为“1”到“根本不想吸”评分为“5”。整个问卷得分(SASET)及其3种情境的得分用于评价拒烟自我效能水平;得分越高表明拒烟自我效能水平越高。本研究总量表具有较好的内部一致性信度(Cronbach’s α=0.884)。
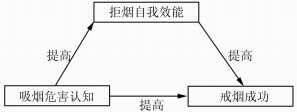 |
| 图 1 中介效应分析模型 |
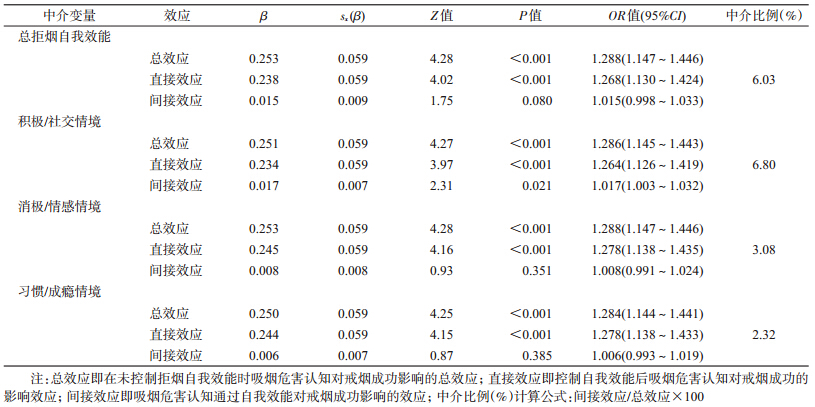
4. 统计学分析:分类资料组间比较采用确切概率的χ2检验。计量资料的组间比较,若方差齐同,采用单因素方差分析;若方差不齐,则采用Kruskal- Wallis秩和检验。以基于KHB方法[13]的logistic回归分析评估拒烟自我效能在吸烟危害认知对戒烟成功影响中的中介效应。吸烟危害认知对戒烟影响的总效应(在没有控制中介变量拒烟自我效能时,自变量吸烟危害认知对因变量戒烟是否成功的影响效应)可分为直接效应(控制了中介变量拒烟自我效能后,自变量吸烟危害认知对因变量戒烟是否成功的影响效应)和间接效应即中介效应(自变量吸烟危害认知通过中介变量拒烟自我效能对因变量戒烟是否成功的影响效应)。所有统计学分析均采用Stata/SE 13.1统计软件(Stata Corporation,College Station,TX,USA)。显著性检验均为双侧检验,P<0.05为差异有统计学意义。 结果
1. 一般特征:除职业外,戒烟成功者与戒烟失败者两组人群的年龄、开始吸烟年龄、教育程度、婚姻状况、拒烟自我效能及吸烟危害认知的差异均有统计学意义(表 2)。
2. 中介效应分析:控制年龄、开始吸烟年龄、职业、教育程度及婚姻状况混杂因素后,吸烟危害认知对戒烟成功的效应显著(P<0.001),对吸烟危害的认知度越高,越容易成功戒烟(OR=1.288,95%CI:1.147~1.446),拒烟自我效能的中介效应占吸烟危害认知对戒烟成功影响总效应的6.03%,吸烟危害认知对戒烟成功的直接效应占总效应的93.97%,且在拒烟自我效能3种特定的情境下,吸烟危害认知度越高,越容易成功戒烟(积极/社交情境:OR=1.286,95%CI:1.145~1.443,P<0.001;消极/情感情境:OR=1.288,95%CI:1.147~1.446,P<0.001,习惯/成瘾情境:OR=1.284,95%CI:1.144~1.441,P<0.001),3种情境下的中介效应占吸烟危害认知对戒烟成功总效应的比例分别为6.80%、3.08%和2.32%(表 3)。
本研究探讨拒烟自我效能在吸烟危害认知对戒烟成功的中介效应。结果显示,拒烟自我效能在吸烟危害认知对戒烟成功的总效应中具有部分中介效应(6.03%),而吸烟危害认知对戒烟成功的直接效应占主要地位(93.97%)。该结果在实际生活中可能具有合理性。据以往研究及本研究表明,影响戒烟的主要因素是患病或担心自己患病[14, 15]。由此可推断,如果吸烟者患病,无论拒烟自我效能高低,均倾向于戒烟。
本研究结果还表明,拒烟自我效能在积极/社交(6.80%)、消极/情感(3.08%)和习惯/成瘾(2.32%)3种特定情境下吸烟危害认知对戒烟成功影响的中介效应也较小。许多研究表明,成瘾或消极情感(焦虑和抑郁)是导致吸烟欲望增加的危险因素[16, 17]。因此,在成瘾或消极情境下,即使高危害认知水平的吸烟者,其拒烟自我效能可能依然较低。另外,在我国尤其是农村,吸烟作为一种社交手段,在人际交往中已极普遍[18]。因此,在积极情境(与朋友聚会及配偶或好友是吸烟者)下,即使吸烟者对烟草危害认知水平较高,由于社交需要,其拒烟自我效能可能依然较低。
本研究存在不足。首先,分析数据源自被调查者的自我报告,可能存在选择和回忆偏倚;其次,调查对象均为农村居民,因其对吸烟危害的认知水平有差异,因此本文结果是否适用于城市居民仍需进一步探讨。由于戒烟是否成功受很多因素影响,故仍有许多未调查的因素可能影响本文结果。
尽管如此,本文仍表明,拒烟自我效能在吸烟危害认知对戒烟成功的影响中具有部分中介效应。而提高吸烟者的危害认知水平不仅直接促使其戒烟成功,还可通过增大其拒烟自我效能,促使其戒烟成功。
(感谢调查地区卫生局、疾病预防控制中心及其他有关机构在调查中给予的大力支持与帮助)
| [1] Zhang H,Cai BQ. The impact of tobacco on lung health in China[J]. Respirology,2003,8(1):17-21. |
| [2] Yang GH,Ma JM,Liu N,et al. Smoking and passive smoking in Chinese,2002[J]. Chin J Epidemiol,2005,26(2):77-83. (in Chinese)杨功焕,马杰民,刘娜,等. 中国人群2002年吸烟和被动吸烟的现状调查[J]. 中华流行病学杂志,2005,26(2):77-83. |
| [3] Feng GZ,Jiang Y,Li Q,et al. Individual-level factors associated with intentions to quit smoking among adult smokers in six cities of China:findings from the ITC China Survey[J]. Tob Control,2010,19 Suppl 2:i6-11. |
| [4] Tejada CAO,Ewerling F,Dos Santos AMA,et al. Factors associated with smoking cessation in Brazil[J]. Cad Saúde Pública,2013,29(8):1555-1564. |
| [5] Yang T,Abdullah ASM,Mustafa J,et al. Factors associated with smoking cessation among Chinese adults in rural China[J]. Am J Health Behav,2009,33(2):125-134. |
| [6] Sansone GC,Raute LJ, Fong GT,et al. Knowledge of health effects and intentions to quit among smokers in India:Findings from the Tobacco Control Policy (TCP) India Pilot Survey[J]. Int J Environ Res Public Health,2012,9(2):564-578. |
| [7] Schnoll RA,Martinez E,Tatum KL,et al. Increased self-efficacy to quit and perceived control over withdrawal symptoms predict smoking cessation following nicotine dependence treatment[J]. Addict Behav,2011,36(1/2):144-147. |
| [8] Woodruff SI, Conway TL,Edwards CC. Sociodemographic and smoking-related psychosocial predictors of smoking behavior change among high school smokers[J]. Addict Behav,2008,33(2):354-358. |
| [9] Shadel WG,Cervone D. Evaluating social-cognitive mechanisms that regulate self-efficacy in response to provocative smoking cues:an experimental investigation[J]. Psychol Addict Behav,2006,20(1):91-96. |
| [10] Global Tobacco Surveillance System (GTSS). Global adult tobacco survey (GATS):core questionnaire with optional questions[EB/OL].[2015-01-25]. 2008. http://www.cdc.gov/tobacco/global/gots/. |
| [11] WHO. Guidelines for controlling and monitoring the tobacco epidemic[M]. Geneva:World Health Organization,1998. |
| [12] Qian JC, Cai M, Gao J,et al. Trends in smoking and quitting in China from 1993 to 2003:National Health Service Survey Data[J]. Bull World Health Organ,2010,88(10):769-776. |
| [13] Kohler U,Karlson KB, Holm A. Comparing coefficients of nested nonlinear probability models[J]. Stata J,2006,11(3):420-438. |
| [14] Curry SJ,Grothaus L,McBride C. Reasons for quitting:intrinsic and extrinsic motivation for smoking cessation in a population-based sample of smokers[J]. Addict Behav,1997,22(6):727-739. |
| [15] Yang GH,Ma JM,Chen AP,et al. Smoking cessation in China:findings from the 1996 national prevalence survey[J]. Tob Control,2001,10(2):170-174. |
| [16] Morissette SB, Tull MT, Gulliver SB, et al. Anxiety, anxiety disorders,tobacco use,and nicotine:a critical review of interrelationships[J]. Psychol Bull,2007,133(2):245-272. |
| [17] Haukkala A, Uutela A,Vartiainen E, et al. Depression and smoking cessation:the role of motivation and self-efficacy[J]. Addict Behav,2000,25(2):311-316. |
| [18] Rich ZC,Xiao SY. Tobacco as a social currency:cigarette gifting and sharing in China[J]. Nicotine Tob Res,2012,14(3):258-263. |
 2015, Vol. 36
2015, Vol. 36