文章信息
- 王新玲, 热孜万古丽·乌斯曼, 马福慧, 郭艳英, 艾合买提江·吐呼提, 赵红丽, 木尼拉·阿不都乃依木, 靳晓萍, 王惠丽, 邢淑清. 2015.
- Wang Xinling, Osiman Reziwan, Ma Fuhui, Guo Yanying, Tuhuti Hemai, Zhao Hongli, Abudunaiyimu Munila, Jin Xiaoping, Wang Huili, Xing Shuqing. 2015.
- 新疆乌鲁木齐市常住居民甲状腺功能、甲状腺自身抗体与尿碘变化的分析
- Changes of thyroid function, thyroid antibodies and urinary iodine among permanent residents of Urumqi in Xinjiang
- 中华流行病学杂志, 2015, 36(8): 811-814
- Chinese Journal of Epidemiology, 2015, 36(8): 811-814
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2015.08.009
-
文章历史
- 投稿日期:2014-11-21
2010年我国10城市居民大样本横断面调查显示甲状腺疾病流行趋势明显,尤其临床甲状腺功能减低(临床甲减)和亚临床甲减(亚甲减)例数增加,且与尿碘水平增高相关[1]。美国早在2002年就基于不同性别、年龄、人种等做过一项国家大型营养调查(NHANES Ⅲ)[2]。而甲状腺功能异常预示心血管疾病、高胆固醇血症、甲状腺癌等发病增加[3, 4],鉴于目前甲状腺疾病患病率及危害性显著升高,而公众对诊断知晓率较低,本次调查新疆乌鲁木齐市部分常住居民甲状腺疾病的流行情况,了解甲状腺疾病诊断知晓率、年龄分布的差异,分析甲状腺功能、自身抗体与居民碘营养的变化关系。 对象与方法
1. 调查对象:2013年5月在乌鲁木齐市采用横断面方法随机抽取1 995名常住成年居民,男性606人(30.4%),女性1 389人(69.6%)。年龄18~84岁,平均(46.3±14.2)岁。其中89人为既往已诊断为甲状腺功能异常者,1 906人为健康人群。调查对象排除近期(6个月内)使用碘造影剂和胺碘酮、激素类药物者,以及孕妇、糖尿病患者、肾功能异常者。所有调查对象均签署知情同意书。
2. 调查方法:调查前按统一方法培训现场调查和实验室人员。所有实验室检测项目从采样到结果报告均进行严格的质量控制,每一种指标均有同一名专业人员负责测定,保证实验室各项检测结果准确性。
(1)现场调查:包括体格检查、问卷调查了解甲状腺相关既往病史及家族史。
(2)血甲状腺功能测定:留取静脉血标本5 ml,采用化学发光免疫法(德国罗氏公司Cobas e601全自动电化学发光免疫分析仪)测定促甲状腺素(TSH)、血清游离甲状腺素(FT4)、游离三碘甲状腺原氨酸(FT3)、甲状腺球蛋白抗体(TgAb)、甲状腺过氧化物酶抗体(TPOAb)。
(3)尿碘:采集一次性晨尿10 ml,置于清洁聚乙烯塑料中,密封,4 ℃冷藏,根据《尿中碘的砷铈催化分光光度法》(WS/T 107-2006)检测尿碘[5],尿碘标准物由国家碘缺乏病参照实验室提供。
3. 诊断标准:本次调查确定TSH正常范围为0.64~6.16 μIU/ml,FT4为12~22 pmol/L,FT3为3.1~6.8 pmol/L;TgAb滴度>116 IU/ml为抗体阳性;TPOAb滴度>35 IU/ml为抗体阳性。TSH、FT3、FT4均正常为甲状腺功能正常;TSH值升高及FT4、FT3值正常为亚甲减;TSH值升高,FT4 或FT3值降低为临床甲减;TSH值降低,FT4、FT3值正常为亚临床甲状腺功能亢进(亚甲亢);TSH值降低,FT4或FT3值升高为甲状腺功能亢进(临床甲亢)。依据2001年WHO、联合国儿童基金会(UNICEF)和国际控制碘缺乏病委员会(ICCIDD)共同修订的评价碘营养状态的标准[6]:尿碘<100 μg/L为碘缺乏,100~299 μg/L为碘适宜,≥300 μg/L为碘过量。
4. 统计学分析:所有数据均输入Excel软件数据库,应用SPSS 16.0软件进行统计学分析。使用K-S检验数据分析是否服从正态分布,用x或M表示数据的集中分布趋势,构成比用n(%)表示。正态分布组间比较选用方差分析,非正态分布用非参数秩和检验,率的比较采用χ2检验。以P<0.05为差异有统计学意义。 结 果
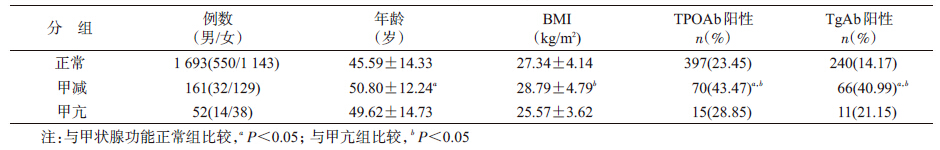
1. 样本基本特征:按照TSH及FT4、FT3值将新诊断的甲状腺功能异常者分为亚甲减、临床甲减、亚甲亢和甲亢。其中临床甲亢和亚甲亢合并为甲亢组(2.7%),临床甲减和亚甲减合并为甲减组(8.5%)。甲状腺功能正常组的年龄低于甲减组(P<0.001),而与甲亢组及甲亢组与甲减组年龄分布的差异无统计学意义(P>0.05)。甲减组甲状腺自身抗体阳性率明显高于甲亢组(χ2=7.739,P=0.005)和甲状腺功能正常组(χ2=35.526,P<0.001),见表 1。甲状腺功能异常者中均以亚甲减和甲减构成比较高,但不同甲状腺功能异常组间年龄、性别构成比的差异无统计学意义(P>0.05),数据具有均衡可比性。≥60岁组甲状腺功能异常者56例(15.8%),与<60岁组(157例)比较差异有统计学意义(χ2=9.445,P=0.002),见表 2。
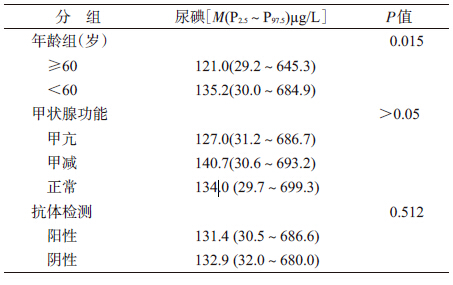
2. 尿碘检测:调查对象尿碘M=134.5(P2.5~P97.5:35.5~637.5)μg/L,其中碘缺乏占32%,碘适宜占58%,碘过量占10%。经秩和检验比较,<60岁人群尿碘M值高于≥60岁人群(P=0.015);甲状腺功能正常组与甲亢、甲减组尿碘水平两两比较的差异均无统计学意义 (P>0.05);抗体阳性组与阴性组比较尿碘水平也无差异(P=0.512),见表 3。
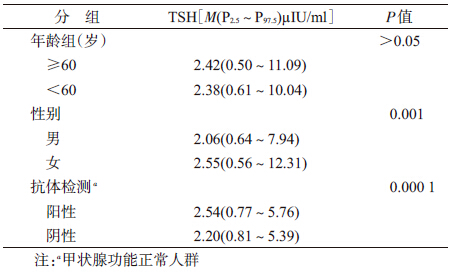
3. 血清TSH变化:调查对象TSH水平不符合正态分布,其M=2.39(P2.5~P97.5:0.59~10.39)μIU/ml,女性高于男性(P<0.001);甲状腺功能正常人群中抗体阳性者的TSH水平明显高于阴性者(表 4)。
新疆为我国碘缺乏地区[7],且既往鲜有大样本甲状腺疾病调查。本次调查发现甲状腺功能异常者占受检健康人群的11.2%(213/1 906),其中亚甲减病例最多(5.7%),临床甲减、亚甲亢和临床甲亢分别占2.7%、2.3%和0.5%;TPOAb和TgAb阳性率分别为23.2%和16.6%,与一些地区患病比例相当[8]。甲减组病例平均年龄和抗体阳性率均高于甲亢组和甲状腺功能正常组,且女性多于男性。表明本次调查结果除甲亢(临床甲亢+亚临床甲亢)外其他各项指标均高于2010年我国10城市居民大样本横断面调查的全国平均水平。
本调查显示居民碘营养状况表现为部分缺乏和过量,但尿碘水平在甲状腺功能正常组与异常组、抗体阳性组与阴性组的差异无统计学意义(P>0.05)。有研究表明高碘摄入可能导致自身免疫性甲状腺疾病、甲亢、甲状腺癌、甲状腺功能低下等,而低碘摄入可能导致甲状腺功能减退[9, 10]。但本次调查结果显示尿碘与TSH及甲状腺自身抗体并无明显的相关性,表明该人群尿碘水平并没有影响甲状腺功能的变化及甲状腺自身抗体的表达,提示该人群碘摄入多数为碘适宜,但不能排除碘摄入水平高低与甲状腺疾病尤其是甲状腺功能和抗体的表达无相关性。<60岁人群尿碘水平明显高于≥60岁人群,这可能与老年人摄碘减少、肾脏排泄功能减退以及甲状腺本身敏感性增加相关。
本文调查人群TSH(M=2.39 μIU/ml)与全国水平相当。随着年龄增长TSH有增高趋势但不明显,女性高于男性。本文甲减人群多集中在≥60岁的老年人群,女性中更明显,与Díez等[11]研究相似。既往研究显示>60岁的女性甲状腺疾病的流行率显著高于≤60岁女性[12, 13]。另据报告显示,甲状腺功能正常人群中当甲状腺自身抗体表达阳性时TSH水平也高于抗体阴性人群[14],本文验证了该观点,可能与甲状腺自身免疫机制相关,是甲减发病前的状态。
综上所述,本次乌鲁木齐市居民甲状腺功能异常患病率、甲状腺自身抗体表达与尿碘水平变化关系的调查表明,该人群碘摄入水平并未影响甲状腺功能变化及甲状腺自身抗体的表达;≥60岁人群甲状腺功能异常明显高于<60岁人群。由于老年人甲状腺功能减低常缺乏典型的临床表现,诊断主要依据甲状腺功能及抗体的测定,建议加强对该人群甲状腺疾病(尤其是亚甲减)的筛查。
| [1] Sun X, Shan Z, Teng W. Effects of increased iodine intake on thyroid disorders [J]. Endocrinol Metab, 2014, 29(3):240-247. |
| [2] Golden SH, Robinson KA, Saldanha I, et al. Prevalence and incidence of endocrine and metabolic disorders in the United States:a comprehensive review[J]. Clin Endocrinol Metab, 2009, 94(6):1853-1878. |
| [3] Razvi S, Weaver JU, Vanderpump MP, et al. The incidence of ischemic heart disease and mortality in people with subclinical hypothyroidism:reanalysis of the Whickham Survey Cohort[J].Clin Endocrinol Metab, 2010, 95(4):1734-1740. |
| [4] Spencer CA. Clinical review: clinical utility of thyroglobulin antibody (TgAb) measurements for patients with differentiated thyroid cancers (DTC)[J]. Clin Endocrinol Metab, 2011, 96(12):3615-3627. |
| [5] Ministry of Health of the People's Republic of China. WS/T 107-2006 Method for determination of iodine in urine by As3+-Ce4+ catalytic spectrophotometry[S]. Beijing:People's Medical Publishing House, 2006. (in Chinese). 中华人民共和国卫生部. WS/T 107-2006 尿中碘的砷铈催化分光光度法[S]. 北京:人民卫生出版社, 2006. |
| [6] WHO/UNICEF/ICCIDD. Assessment of the iodine deficiency disorders and monitoring their elimination[S]. Geneva:WHO, 2001. |
| [7] Zhang L, Wang FR, Ma PJ, et al. Monitoring results of iodine deficiency disorders in Xinjiang Uyghur Autonomous Region in 2011 [J]. Chin J Endemiol, 2014, 33(1):68-71. (in Chinese) 张玲, 王锋锐, 马品江, 等. 2011年新疆碘缺乏病监测结果分析[J]. 中华地方病学杂志, 2014, 33(1):68-71. |
| [8] Delitala AP, Pilia MG, Ferreli L, et al. Prevalence of unknown thyroid disorders in a Sardinian cohort[J]. Eur J Endocrinol, 2014, 171(1):143-149. |
| [9] Laurberg P, Jorgensen T, Perrild H, et al. The Danish investigation on iodine intake and thyroid disease, DanThyr:status and perspectives[J]. Eur J Endocrinol, 2006, 155(2):219-228. |
| [10] Teng W, Shan Z, Teng X, et al. Effect of iodine intake on thyroid diseases in China[J]. N Engl J Med, 2006, 354(26):2783-2793. |
| [11] Díez JJ, Molina I, Ibars MT. Prevalence of thyroid dysfunction in adults over age 60 years from an urban community[J]. Exp Clin Endocrinol Diab, 2003, 111(8):480-485. |
| [12] van de Ven AC, Netea-Maier RT, de Vegt F, et al. Associations between thyroid function and mortality:the influence of age[J]. Eur J Endocrinol, 2014, 171(2):183-191. |
| [13] Bremner AP, Feddema P, Leedman PJ, et al. Age-related changes in thyroid function:a longitudinal study of a community-based cohort[J]. Clin Endocrinol Metab, 2012, 97(5):1554-1562. |
| [14] Surks MI, Hollowell JG. Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population:implications for the prevalence of subclinical hypothyroidism[J].Clin Endocrinol Metab, 2007, 92(12):4575-4582. |
 2015, Vol. 36
2015, Vol. 36