文章信息
- 黎杨芬, 周书进, 王小娟, 何玥, 沈琳, 黄昕, 文师吾, 谭红专. 2015.
- Li Yangfen, Zhou Shujin, Wang Xiaojuan, He Yue, Shen Lin, Huang Xin, Wen Shiwu, Tan Hongzhuan. 2015.
- 宫内发育迟缓影响因素的研究
- Study on the determinants of intrauterine growth restriction
- 中华流行病学杂志, 2015, 36(8): 807-810
- Chinese Journal of Epidemiology, 2015, 36(8): 807-810
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2015.08.008
-
文章历史
- 投稿日期:2014-12-31
2. 浏阳市妇幼保健院;
3. 中南大学湘雅医院;
4. 长沙市疾病预防控制中心
2. Liuyang Maternal and Child Health Hospital;
3. Xiangya Hospital, Central South University;
4. Changsha Center for Disease Control and Prevention
宫内发育迟缓是导致新生儿发病和死亡的第二大主要原因,仅次于早产[1]。并与多种新生儿合并症存在密切关系[2, 3],宫内发育迟缓与肥胖、心脑血管疾病、糖代谢异常等多种成年期代谢疾病也存在关联[4, 5]。本文回顾性分析了2008年4月至2011年3月湖南省浏阳市14个乡镇单胎妊娠孕妇的孕产妇保健手册和分娩病历资料,探讨母体因素对宫内发育迟缓的影响。 对象与方法
1. 研究对象:采用随机整群抽样方法,从浏阳市37个乡镇中随机抽取14个乡镇,收集所抽乡镇2008年4月1日至2011年3月31日所有产妇的孕期保健手册和分娩病历记录,内容包括姓名、年龄、职业、身高、初诊体重、孕产史等基本信息,以及孕周、新生儿出生体重和分娩情况。排除多胎妊娠、死胎、死产、新生儿出生缺陷和子宫畸形的孕产妇。浏阳市孕产妇系统管理率(95.98%)和孕产妇住院率(97.99%)均较高,保证了资料的代表性和可靠性。
2. 诊断标准和定义:①孕周:按末次月经的第一日算起计算孕周。②宫内发育迟缓:胎儿出生体重低于同孕周正常体重的第10百分位数[6]。③妊娠高血压综合征:包括妊娠期高血压和子痫前期,即妊娠期首次出现血压≥140/90 mmHg(1 mm Hg=0.133 kPa)并于产后12周恢复正常且尿蛋白阴性,或20周后首次出现血压≥140/90 mmHg且尿蛋白≥300 mg/24 h或尿蛋白(+),可伴有上腹部不适、头痛、视力模糊等症状。④孕产妇贫血:妊娠末期检测血常规Hb≥100 g/L为正常,90 g/L≤Hb<100 g/L为轻度贫血,Hb<90 g/L为中重度贫血。⑤孕期增重:根据美国医学研究院(IOM)2009年推荐的孕期体重总增重范围[7],孕妇孕前BMI(kg/m2)<18.5、18.5~24.9、25.0~29.9和≥30推荐的孕期总增重范围分别为12.6~18.0 kg、11.2~15.8 kg、6.8~11.2 kg和5.0~9.0 kg,在孕前BMI(本研究用初诊BMI值代替孕前BMI值)的基础上根据其孕期总增重的水平是否低于或超出该范围,分为增重不足、正常和过高。
3. 统计学分析:采用EpiData 3.0软件建立数据库,采用统一标准录入研究对象的孕期保健手册和分娩病历记录。采用SPSS 19.0软件进行统计学分析,单因素采用χ2检验,检验水准α=0.05,多因素分析采用非条件logistic回归分析(α入=0.05,α出=0.10)。 结 果
1. 一般情况:共收集6 237名分娩孕妇完整的孕产妇孕期保健手册和分娩病历记录,剔除132名多胎妊娠、死胎死产、新生儿出生缺陷和子宫畸形的孕产妇,最后得到6 105人的有效数据(有效率为97.88%)。孕妇年龄17~42岁,平均(24.43±3.82)岁。6 105例单胎活产新生儿中,男性3 261例(53.4%),女性2844例(46.6%),其中宫内发育迟缓患儿528例,发生率为8.65%。
2. 影响因素分析:
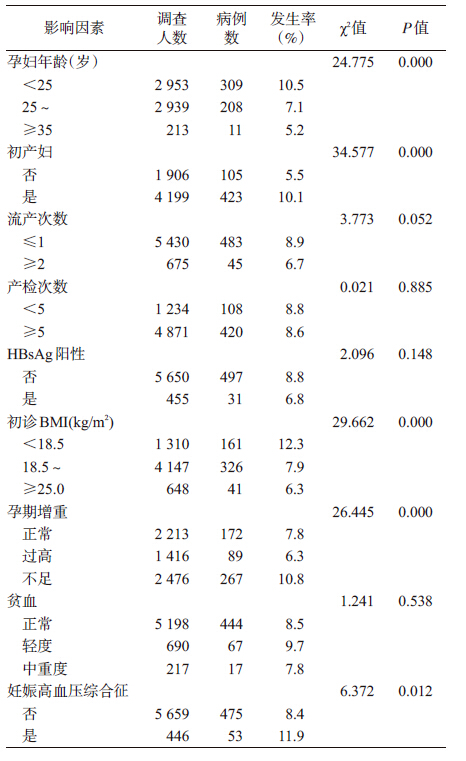
(1)单因素分析:将孕妇年龄等9个可疑因素纳入分析,进行单因素χ2检验(表 1)。结果显示,孕妇年龄、是否初产妇、初诊BMI、孕期增重和妊娠高血压综合征与宫内发育迟缓的关联有统计学意义(P<0.05)。未发现流产次数、产检次数、HBsAg阳性以及贫血与宫内发育迟缓的发生存在统计学关联(P>0.05)。
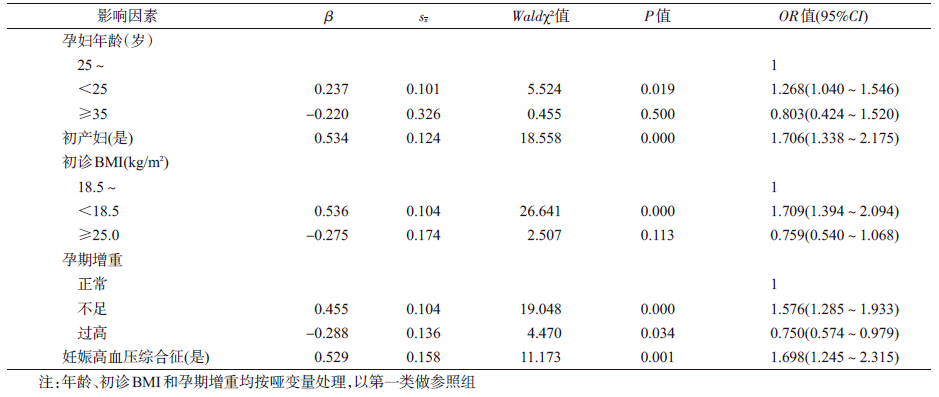
(2)非条件logistic分析:以宫内发育迟缓为应变量,以单因素分析中与宫内发育迟缓有统计学意义或P值接近0.05的6个变量为自变量,进行非条件logistic回归分析。结果显示,孕妇年龄、是否初产妇、初诊BMI、孕期增重和妊娠高血压综合征与宫内发育迟缓存在统计学关联,其中孕妇年龄<25岁、初产妇、初诊BMI<18.5 kg/m2、孕期增重不足以及患妊娠高血压综合征是宫内发育迟缓的危险因素,而孕期增重过高是宫内发育迟缓的保护因素(表 2)。
宫内发育迟缓的发生受到母体与胎儿多方面因素的影响[8],本文主要探讨来自母体方面的因素,包括孕妇社会人口学因素、孕期营养状况、健康状况以及孕期保健水平等。结果显示:孕妇年龄、初产、初诊BMI、孕期增重和妊娠高血压综合征与宫内发育迟缓的发生有关。
以往研究显示,孕妇年龄过小是宫内发育迟缓的危险因素[9],本研究也得到类似结果。由于该年龄人群生殖系统发育不够成熟完善,且生活状态不稳定,甚至有一部分属于未婚或者未成年,往往无法得到很好的孕期保健服务,发生宫内发育迟缓、早产和死胎等的风险高于适龄孕产妇[10]。此外,初产妇发生宫内发育迟缓的危险高于经产妇(OR=1.709),与先前一些研究结果相似[11, 12]。
孕产妇体重一直被认为是影响各种妊娠结局和母儿健康的重要因素[13, 14, 15]。研究显示,孕妇消瘦(初诊BMI<18.5 kg/m2)和孕期增重不足是宫内发育迟缓的危险因素,可能与蛋白质-能量不足、某些重要营养物质缺乏以及血容量不足有关[16]。虽然孕期增重超出IOM推荐范围的孕妇发生宫内发育迟缓的风险略低于增重正常的孕妇(OR=0.75),但是由于孕期增重过度与巨大儿、妊娠期高血压、糖尿病等多种母婴并发症有关[17, 18],因此并不推荐孕期过度增重。
妊娠高血压综合征是孕产妇和围生儿发病和死亡的主要原因[19, 20, 21]。本研究发现合并有妊娠高血压综合征孕妇发生宫内发育迟缓的风险是正常孕妇的1.7倍。Geyl等[22]最近发现,宫内发育迟缓与先兆子痫关系密切。因此,及早发现患有妊娠高血压综合征的孕妇,并加强监测管理,对于降低宫内发育迟缓的发生、改善妊娠结局具有重要意义。
目前关于贫血与宫内发育迟缓的关系还无定论,多数研究认为中重度贫血可通过影响子宫-胎盘供氧等导致宫内发育迟缓的发生[23]。本研究结果显示贫血与宫内发育迟缓并无关联,可能有两方面的原因。一方面,本文贫血诊断是依据妊娠末期Hb浓度,而有研究者认为妊娠晚期贫血与不良妊娠结局并没有关系,主要是孕早期贫血影响胎儿体重[24];另一方面,多种生理、病理原因均可引起Hb浓度下降,不同机制引起的贫血与宫内发育迟缓的关系可能不同。在以后的研究中应区分不同时期与不同类型贫血,分析其与宫内发育迟缓的关系及其机制。
本研究由于资料限制,未考虑孕妇的遗传因素、家庭情况、经济条件、文化程度、社会地位等对宫内发育迟缓的影响。但本文结果仍然为宫内发育迟缓的预防提供了合理可行的建议,即通过孕前或孕早期筛查BMI、监测孕期体重变化并控制体重在适当范围,加强防治妊娠高血压综合征,以减少宫内发育迟缓的发生。
| [1] Phan DA, El KF, Renolleau C, et al. Intrauterine growth retardation and the developing brain[J]. Arch Pediatr, 2013, 20(9):1034-1038. |
| [2] Doi K, Sameshima H, Kodama Y, et al. Perinatal death and neurological damage as a sequential chain of poor outcome[J]. J Matern Fetal Neonatal Med, 2012, 25(6):706-709. |
| [3] Simic KA, Kolundzic Z, Galic S, et al. Language development in preschool children born after asymmetrical intrauterine growth retardation[J]. Eur J Paediatr Neurol, 2012, 16(2):132-137. |
| [4] Crume TL, Scherzinger A, Stamm E, et al. The long-term impact of intrauterine growth restriction in a diverse U.S. cohort of children:the EPOCH study[J]. Obesity(Silver Spring), 2014, 22(2):608-615. |
| [5] Longo S, Bollani L, Decembrino L, et al. Short-term and long-term sequelae in intrauterine growth retardation (IUGR)[J]. J Matern Fetal Neonatal Med, 2013, 26(3):222-225. |
| [6] American College of Obstetricians and Gynecologists. ACOG Practice bulletin no. 134:fetal growth restriction[J]. Obstet Gynecol, 2013, 121(5):1122-1133. |
| [7] Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight Gain During Pregnancy:Reexamining the Guidelines[Z]. Washington (DC):National Academies Press (US), 2009. |
| [8] Nardozza LM, Araujo JE, Barbosa MM, et al. Fetal growth restriction:current knowledge to the general Obs/Gyn[J]. Arch Gynecol Obstet, 2012, 286(1):1-13. |
| [9] Bakker R, Steegers EA, Biharie AA, et al. Explaining differences in birth outcomes in relation to maternal age:the Generation R Study[J]. BJOG, 2011, 118(4):500-509. |
| [10] Arkan DC, Kaplanoglu M, Kran H, et al. Adolescent pregnancies and obstetric outcomes in southeast Turkey:data from two regional centers[J]. Clin Exp Obstet Gynecol, 2010, 37(2):144-147. |
| [11] Campbell MK, Cartier S, Xie B, et al. Determinants of small for gestational age birth at term[J]. Paediatr Perinat Epidemiol, 2012, 26(6):525-533. |
| [12] Padonou G, Le Port A, Cottrell G, et al. Prematurity, intrauterine growth retardation and low birth weight:risk factors in a malaria-endemic area in southern Benin[J]. Trans R Soc Trop Med Hyg, 2014, 108(2):77-83. |
| [13] Rab A, Szentpeteri I, Kornya L, et al. Placental gene expression patterns of epidermal growth factor in intrauterine growth restriction[J]. Eur J Obstet Gynecol Reprod Biol, 2013, 170(1):96-99. |
| [14] Ensenauer R, Chmitorz A, Riedel C, et al. Effects of suboptimal or excessive gestational weight gain on childhood overweight and abdominal adiposity:results from a retrospective cohort study[J]. Int J Obes (Lond), 2013, 37(4):505-512. |
| [15] Gaillard R, Steegers EA, Franco OH, et al. Maternal weight gain in different periods of pregnancy and childhood cardio-metabolic outcomes. The Generation R Study[J]. Int J Obes (Lond), 2014, 39(4):677-685. |
| [16] Neggers Y, Goldenberg RL. Some thoughts on body mass index, micronutrient intakes and pregnancy outcome[J]. J Nutr, 2003, 133(5 Suppl 2):S1737-1740. |
| [17] Gaillard R, Durmus B, Hofman A, et al. Risk factors and outcomes of maternal obesity and excessive weight gain during pregnancy[J]. Obesity (Silver Spring), 2013, 21(5):1046-1055. |
| [18] Johnson J, Clifton RG, Roberts JM, et al. Pregnancy outcomes with weight gain above or below the 2009 Institute of Medicine guidelines[J]. Obstet Gynecol, 2013, 121(5):969-975. |
| [19] Salmani D, Purushothaman S, Somashekara SC, et al. Study of structural changes in placenta in pregnancy-induced hypertension[J]. J Nat Sci Biol Med, 2014, 5(2):352-355. |
| [20] Milnerowicz-Nabzdyk E, Zimmer M, Tlolka J, et al. Umbilical cord morphology in pregnancies complicated by IUGR in cases of tobacco smoking and pregnancy-induced hypertension[J]. Neuro Endocrinol Lett, 2010, 31(6):842-847. |
| [21] Macdonald-Wallis C, Tilling K, Fraser A, et al. Associations of blood pressure change in pregnancy with fetal growth and gestational age at delivery:findings from a prospective cohort[J]. Hypertension, 2014, 64(1):36-44. |
| [22] Geyl C, Clouqueur E, Lambert J, et al. Links between preeclampsia and intrauterine growth restriction[Z]. 2014:42, 229-233. |
| [23] Kozuki N, Lee AC, Katz J. Moderate to severe, but not mild, maternal anemia is associated with increased risk of small-for-gestational-age outcomes[J]. J Nutr, 2012, 142(2):358-362. |
| [24] Scholl TO. Iron status during pregnancy: setting the stage for mother and infant[J]. Am J Clin Nutr, 2005, 81(5):1218-1222. |
 2015, Vol. 36
2015, Vol. 36