文章信息
- 何欢, 张洪波, 丁凡, 林小杰, 周易, 肖剑, 陈芳, 黄文, 董燕燕, 杨巧红. 2014.
- He Huan, Zhang Hongbo, Ding Fan, Lin Xiaojie, Zhou Yi, Xiao Jian, Chen Fang, Huang Wen, Dong Yanyan, Yang Qiaohong. 2014.
- 上海和成都市HIV阳性MSM人群性传播危险行为及其影响因素
- Risky sexual transmission behavior and its influencing factors among HIV-positive MSM population in Shanghai and Chengdu in China
- 中华流行病学杂志, 2015, 36(3): 254-258
- Chinese Journal of Epidemiology, 2015, 36(3): 254-258
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2015.03.014
-
文章历史
- 投稿日期:2014-08-06
2. 成都同乐健康咨询服务中心;
3. 上海美丽人生健康服务中心;
4. 上海爱的家园互助小组;
5. 安徽医科大学公共卫生学院儿少卫生与妇幼保健学系
2. Chengdu Tongle Health Consulting Service Center;
3. Shanghai Beautiful Life Health Promotion Center;
4. Shanghai Love Home Support Group;
5. Department of Maternal, Child and Adolescent Health, School of Public Health, Anhui Medical University
MSM人群由于多性伴和高危性行为而成为HIV流行的主要人群之一[1,2,3,4]。随着抗病毒治疗的应用,HIV感染者的生存状况得到改善,病死率明显降低,因此预防HIV传播已经成为公共卫生的重点研究领域[5]。HIV阳性MSM人群传播行为是指HIV阳性MSM与HIV阴性或未知HIV感染状况性伴(包括男性和女性)发生性行为时不使用安全套[6]。Morin等[7]在美国的调查显示,有12.7%的HIV阳性MSM在过去3个月至少发生过1次性传播行为;俄罗斯一项研究表明,在已经接受抗病毒治疗的HIV阳性MSM中,有性传播行为的比例约为1/4[8];另有研究认为,性伴告知是有效降低HIV阳性MSM人群传播行为的重要措施[9];泰国的相关研究显示,仅有36%的研究对象将自己的HIV感染状况告知固定性伴[10]。我国既往仅有少数针对HIV阳性MSM高危行为调查[11,12],尚未见针对传播行为的研究。米国栋等[11]对我国部分城市754名HIV阳性MSM的调查显示,无保护肛交行为的报告率高达67.4%;另一项在上海市HIV阳性MSM人群中的调查表明,57.5%的调查对象报告最近6个月有同性肛交行为,13.5%有异性性行为,与男性发生肛交和女性阴道性交行为时不能坚持每次使用安全套者分别占16.0%、3.5%。HIV阳性MSM与男性偶然性伴的高危行为报告率较高,且近1/3的研究对象拥有偶然性伴[12]。
针对我国MSM人群HIV感染者数量持续上升的严峻状况,迫切需要研究确定HIV阳性MSM的传播行为状况,为发展针对性的干预策略提供依据。本研究旨在通过对HIV阳性且有无保护性行为(无保护肛交或阴道性交)的MSM进行调查,描述HIV阳性MSM的无保护性行为中有“继续传播”危险的比例,分析其性传播行为与其健康状况及性伴告知的关系,为在该人群深入进行干预研究奠定基础。 对象与方法
1. 研究对象:于2013年1-7月在上海和成都市将年龄≥18周岁、既往经免疫印迹试验确认HIV阳性且经男男性行为途径感染、最近6个月与男性或女性发生过无保护性行为、居住在上海市或成都市且愿意参加调查并提供书面知情同意者列为研究对象。
2. 调查方法:采用滚雪球的方法在HIV阳性MSM中共招募308名调查对象。由经过统一培训的调查员对调查对象进行一对一匿名问卷调查,调查内容包括研究对象的社会人口学特征、健康状况(感染HIV的时间、病毒载量水平、CD4+T淋巴细胞计数、最近1年患性病状况、抑郁焦虑症状),接受艾滋病相关卫生服务(CD4+T淋巴细胞计数和抗病毒治疗状况)、最近6个月性伴种类及性伴感染状况(拥有男性固定性伴,男性偶然/商业性伴以及女性性伴情况、调查对象自我报告性伴的HIV感染状况等)、最近6个月无保护性行为(与HIV阳/阴性性伴、HIV感染状况未知的性伴发生性行为时不能坚持使用安全套情况)、固定性伴及偶然/商业性伴告知等。
3. 相关定义及标准:①性传播行为是指调查对象与HIV阴性或感染状况未知的性伴发生同性无保护肛交行为或异性无保护阴道性交行为。②性伴告知(将自己感染HIV告知性伴)包括固定性伴告知和偶然/商业性伴告知。每类性伴告知分为:均告知(告知全部性伴)、部分告知(告知部分性伴)和均未告知(未告知任何性伴)。性伴告知时间是指从确诊HIV感染之日起,调查对象在多少天内告知性伴。③抑郁/焦虑症状评定采用流调用抑郁自评量表(Center for Epidemiological Survey,Depression Scale,CES-D)和Zung编制的焦虑自评量表(Self-Rating Anxiety Scale,SAS),分别包括20个项目,询问调查对象最近1周出现每种感受的频度,根据频度依次计分为0、1、2和3分,将每条目得分相加,抑郁量表总得分≥16分者为有抑郁症状;焦虑量表将每个条目得分相加得项目粗分,再将项目粗分乘1.25取整数得标准分,标准分≥50分者为有焦虑症状。
4. 统计学分析:采用EpiData 3.0软件建立数据库,运用SPSS 13.0软件统计分析数据。描述分析有高危性行为的HIV阳性MSM人群社会人口学特征、身体及心理健康状况、性伴种类和性行为状况。采用χ2检验分析调查对象社会人口学特征、健康状况、性伴告知与最近6个月性传播行为的关系。采用非条件logistic回归(逐步回归法,α=0.05)分析MSM人群中HIV感染者最近6个月性传播行为的影响因素。以P<0.05为差异有统计学意义。 结果
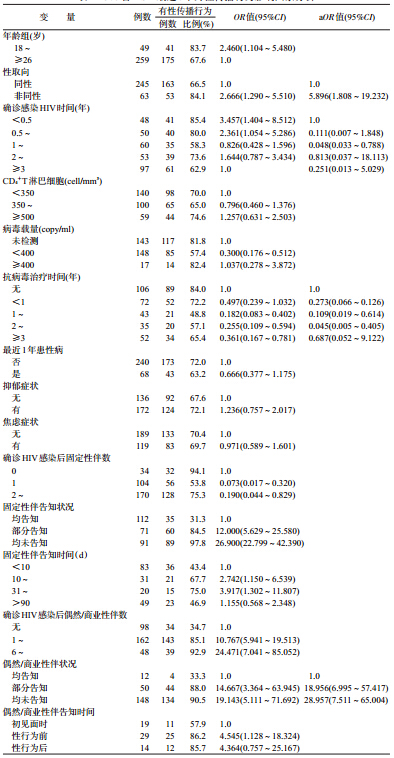
1. 性传播行为的单因素分析:308名调查对象中,最近6个月至少有一次性传播行为报告率为70.1%(216/308)。确认HIV感染后拥有男性固定性伴、男性偶然或商业性伴的比例分别为89.0%(274/308)和68.2%(210/308),其中未告知固定性伴、未告知偶然或商业性伴的比例分别为59.1%(162/274)和94.3%(198/210)。未告知固定性伴者中,91.9%(149/162)最近6个月至少有一次性传播行为,未告知偶然或商业性伴者中相应的比例为89.9%(178/198)。以最近6个月是否报告性传播行为作为结果变量,采用单因素logistic回归方法,分别分析健康状况、接受艾滋病相关服务和性伴告知行为相关变量与HIV传播行为的关系,结果表明,年龄在18~25岁、非同性性取向、确诊感染HIV时间<1年、未接受抗病毒治疗、确诊感染后无固定性伴、确诊感染后未将感染状况告知固定性伴、确诊感染后有偶然/商业性伴、未将感染状况告知偶然/商业性伴均与HIV阳性MSM人群的性传播行为有关(表 1)。
2. HIV传播行为的多因素分析:以调查对象最近6个月是否发生性传播行为为因变量(是=1,否=0),以年龄、性取向、确诊感染HIV时间、抗病毒治疗时间、男性偶然/商业性伴告知等为自变量,进行非条件logistic回归分析(Forward:LR 法)。结果显示,以同性性取向者为参照,非同性性取向者最近6个月至少发生一次性传播行为的危险增加约6倍(aOR=5.896,95% CI:1.808~19.232);以确诊HIV感染<6个月作为参照,确诊感染时间为1~2年者最近6个月至少发生一次性传播行为的危险性降低(aOR=0.048,95% CI:0.033~0.788);以未接受抗病毒治疗为参照,接受抗病毒治疗时间为1~2年者和2~3年者最近6个月至少发生一次性传播行为的危险性均降低(aOR=0.109,95% CI:0.019~0.614和aOR=0.045,95% CI:0.005~0.405);确诊感染后均未将感染状况告知男性偶然/商业性伴者和部分告知者最近6个月至少发生一次性传播行为的危险均高于告知者,分别增加29倍(aOR=28.957,95% CI:7.511~65.004)和19倍(aOR=18.956,95% CI:6.995~57.417),见表 1。 讨论
本研究发现,在上海和成都市调查的308名HIV阳性且无保护性行为的MSM中,最近6个月至少有一次性传播行为者为70.1%,其中≤25岁者该报告率高达83.7%,说明我国HIV阳性的MSM人群无保护性行为中,继续传播行为的比例超过2/3。结合既往研究中HIV阳性MSM无保护性行为的报告率(34%~67%)[11,12],认为我国HIV阳性MSM中具有继续传播行为的比例约为1/4~1/2。美国和英国的横断面研究表明,HIV阳性的MSM具有继续传播行为者比例约为1/4~1/3[13,14,15];Metsch等[16]队列研究显示,MSM在确诊HIV感染6个月后继续传播行为的报告率为27.5%。由此可见,我国HIV阳性MSM中继续传播行为的比例可能高于美国和俄罗斯。
HIV阳性MSM继续传播HIV需具备两个条件,即有“性传播行为”和体内具有可传播的HIV病毒载量。相关研究认为,前者对HIV传播的贡献高于后者,两者共同作用可使HIV传播概率达到28.9%[17]。有研究发现,MSM在确认感染HIV的第一年中发生性传播行为比例最高(44.7%)[18];美国新确诊的HIV感染者占HIV阳性MSM的比例不足7%,而对“MSM社区病毒载量水平”的贡献超过1/3[19]。因此,“发现并及早进行抗病毒治疗”被认为是有效减少HIV传播的干预策略[20]。本研究发现,确诊感染HIV时间<6个月者和未接受抗病毒治疗者,性传播行为的报告率均很高(分别为85.4%和84.0%);还发现病毒载量水平越高者性传播行为的报告率越高。这些结果提示,在HIV感染早期,HIV阳性MSM体内的病毒载量处于高水平,由于未及早进行抗病毒治疗使其体内病毒得到有效抑制,加之传播性行为的广泛存在,可能是我国MSM人群HIV感染率居高不下的重要原因。
性伴告知可能成为影响HIV继续传播的另一重要因素。HIV阳性MSM未将自己的感染状况告知性伴,增加性伴在不知情的状况下发生高危性行为的危险性,从而成为促进HIV继续传播的危险因素[21,22]。本研究发现,仅有40.9%的研究对象将自己的HIV感染状况告诉全部固定性伴,有5.7%的研究对象进行了偶然性伴告知,均低于西方国家水平(69%~75%)[23,24]。尤其值得注意的是,本研究中将自己HIV感染状况告知固定性伴或偶然性伴者,其最近6 个月至少发生一次传播性行为报告率约为30%,而未告知性伴者传播性行为的报告率超过90%;多因素分析进一步证实,与告知全部偶然性伴者相比,均未告知和部分告知者发生性传播行为的危险性分别增加到29倍和19倍。有研究认为,在与性伴发生性行为时,如果性伴不表明自己的HIV感染状况或者不要求使用安全套,HIV阳性MSM会假定性伴也是HIV感染者;同样,在HIV阴性的MSM中也存在类似的性伴感染状况假定现象[25]。因此,促进HIV阳性MSM进行性伴告知可能会减少传播行为,从而降低二代传播。
本研究采用滚雪球方法招募研究对象,限制了研究样本对目标人群的代表性,可能影响研究结果外推;另外,行为资料是通过调查对象自我报告获得,可能存在社会期望偏倚,因此本研究结果可能低估HIV阳性MSM人群中继续传播行为。
综上所述,在HIV阳性且有无保护性行为的MSM人群中,性传播行为比例超过2/3,感染HIV半年内且未接受抗病毒治疗和未进行性伴告知者是性传播行为干预的重点对象,因此,需要针对上述人群特点,建立综合干预策略遏制HIV阳性MSM继续进行二代传播。
| [1] Xu J,Han DL,Liu Z,et al. The prevalence of HIV infection and the risk factors among MSM in 4 cities,China[J]. Chin J Prev Med,2010,44(11):975-980. (in Chinese) 许娟,韩德林,刘征,等. 中国四座城市男男性行为人群HIV感染状况及危险因素[J]. 中华预防医学杂志,2010,44(11):975-980. |
| [2] Wei S, Zhang H,Wang J,et al. HIV and syphilis prevalence and associated factors among young men who have sex with men in 4 cities in China[J]. AIDS Behav,2013,17(3):1151-1158. |
| [3] Song DD,Zhang HB,Wang J,et al. The prevalence of HIV infection and sexual behaviors among men who have sex with men and women in Chengdu and Guangzhou,China[J]. Chin J Epidemiol,2012,33(4):368-373. (in Chinese) |
| [4] Chinese Center for Disease Control and Prevention. The report of the national AIDS epidemic and prevention and control work in December,2013[J]. Chin J AIDS STD,2013,20(2):75. (in Chinese) 中国疾病预防控制中心性病艾滋病预防控制中心. 2013年12月全国艾滋病性病疫情及主要防治工作进展[J]. 中国艾滋病性病杂志,2013,20(2):75. |
| [5] van de Ven P,Prestage G,Crawford J,et al. Sexual risk behavior increases and is associated with HIV optimism among HIV- negative and HIV-positive gay men in Sydney over the 4 year period to February 2000[J]. AIDS,2000,14:2951-2953. |
| [6] Blumenthal J,Haubrich R,Jain S,et al. Factors associated with high transmission risk and detectable plasma HIV RNA in HIV-infected MSM on ART[J]. Int J STD AIDS,2014,DOI:10.1177/0956462413518500. |
| [7] Morin SF,Steward WT,Charlebois ED,et al. Predicting HIV transmission risk among HIV-infected men who have sex with men findings from the healthy living project[J]. J Acquir Immune Defic Syndr,2005,40(2):226-235. |
| [8] Yuri A, Amirkhanian JA,Kelly AV,et al. People with HIV in HAART-Era Russia:transmission risk behavior prevalence,antiretroviral medication-taking,and psychosocial distress[J]. AIDS Behav,2011,15:767-777. |
| [9] McFarland W,Chen YH,Raymond HF,et al. HIV seroadaptation among individuals,within sexual dyads,and by sexual episodes,men who have sex with men,San Francisco,2008[J]. AIDS Care,2011,23:261-268. |
| [10] Sirivongrangson P,Lolekha R,Charoenwatanachokchai A,et al. HIV risk behavior among HIV-infected men who have sex with men in Bangkok,Thailand[J]. AIDS Behav,2011,DOI:10.1007/s10461-011-9884-3. |
| [11] Mi GD, Xu J,Dou Z,et al. Prevalence of unprotected anal intercourse and its associated factors among MSM living with HIV in China[J]. Chin J AIDS STD,2010,16(3):255-258. (in Chinese) 米国栋,徐杰,斗智,等. MSM中HIV感染者无保护性肛交行为及影响因素分析[J]. 中国艾滋病性病,2010,16(3):255-258. |
| [12] He H, Wang M, Zhang HB,et al. The unprotected sexual behaviors and its influencing factors among HIV-infected men who have sex with men in Shanghai,China[J]. Chin J Prev Med,2012,46(11):977-982. (in Chinese) 何欢,汪敏,张洪波,等. 男男性行为人群HIV感染者无保护性行为状况及其影响因素分析[J]. 中华预防医学,2012,46(11):977-982. |
| [13] Safren SA,O'Cleirigh C,Skeer M, et al. Demonstration and evaluation of a peer-delivered,Individually-tailored,HIV prevention intervention for HIV-infected MSM in their primary care setting[J]. AIDS Behav,2011,15:949-958. |
| [14] Crepaz N,Marks G,Liau A,et al. Prevalence of unprotected anal intercourse among HIV-diagnosed MSM in the United States:a meta-analysis[J]. AIDS,2009,23:1617-1629. |
| [15] Williamson LM,Dodds JP,Mercey DE,et al. Sexual risk behavior and knowledge of HIV status among community samples of gay men in the UK[J]. AIDS,2008,22:1063-1070. |
| [16] Metsch LR,Pereyra M,Messinger S,et al. HIV transmission risk behaviors among HIV-infected persons who are successfully linked to care[J]. HIV/AIDS CID,2008,47(15):577-584. |
| [17] Hall HI,Holtgrave DR,Tang T,et al. HIV transmission in the United States:considerations of viral load,risk behavior,and health disparities[J]. AIDS Behav,2013. DOI:10.1007/s10461- 013-0426-z. |
| [18] Volz EM,Ionides E,Romero-Severson EO,et al. HIV-1 transmission during rarly infection in men who have sex with men:a phylodynamic analysis[J]. PLoS Med,2013,10(12):e1001568. |
| [19] Krentz HB,Gill MJ. The effect of churn on “Community Viral Load” in a well-defined regional Population[J]. J Acquir Immune Defic Syndr,2013,64(2):190-196. |
| [20] Peterson JL,Miner MH,Brennan DJ,et al. HIV treatment optimism and sexual risk behaviors among HIV positive African American men who have sex with men[J]. AIDS Educat Prev,2012,24(2):91-101. |
| [21] Wei CY,Lim SH, Guadamuz TE,et al. HIV disclosure and sexual transmission behaviors among an internet sample of HIV- positive men who have sex with men in Asia:implications for prevention with positives[J]. AIDS Behav,2011. DOI :10.1007/s10461-011-0105-x. |
| [22] McFarland W,Chen YH,Raymond HF,et al. HIV seroadaptation among individuals,within sexual dyads,and by sexual episodes,men who have sex with men,San Francisco,2008[J]. AIDS Care,2011,23:261-268. |
| [23] Hart TA,Wolitski RJ,Purcell DW,et al. Partner awareness of the serostatus of HIV-seropositive men who have sex with men:impact on unprotected sexual behavior[J]. AIDS Behav,2005,9:155-166. |
| [24] Rietmeijer CA,Lloyd LV,McLean C. Discussing HIV serostatus with prospective sex partners:a potential HIV prevention strategy among high-risk men who have sex with men[J]. Sex Transm Dis,2007,34:215-219. |
| [25] Parsons JT,Severino J,Nanin J,et al. Positive,negative,unknown:assumption of HIV status among HIV-positive men who have sex with men[J]. AIDS Educat Prev,2006,18:139-149. |
 2015, Vol. 36
2015, Vol. 36