文章信息
- 程小林, 郭佶伟, 解菁. 2014.
- Cheng Xiaolin, Guo Jiwei, Xie Jing. 2014.
- 瘦素及胰岛素拮抗与多囊卵巢综合征不孕症相关性研究
- Association between levels of serum leptin and insulin resistance in patients with polycystic ovary syndrome
- 中华流行病学杂志, 2014, 35(12): 1389-1391
- Chinese Journal of Epidemiology, 2014, 35(12): 1389-1391
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2014.12.017
-
文章历史
- 投稿日期:2014-09-03
2 湖北省妇幼保健院妇科;
3 华中科技大学同济医学院附属普爱医院临床检验中心
2 Department of Gynecology, Hubei Maternal and Child Health Hospital;
3 Center of Laboratory Medicine, Affiliated Pu'ai Hospital Huazhong Science and Technology University
多囊卵巢综合征(PCOS)是以稀发排卵或无排卵、高雄激素、高胰岛素血症和多囊卵巢为特征的内分泌紊乱的症候群[1]。据文献报道[2, 3],瘦素作为卵巢功能最敏感的内分泌指标之一,其在机体能量平衡和生殖功能调节中发挥重要作用。此外胰岛素抵抗在PCOS的发病中具有重要作用[4]。为此本研究分析PCOS患者与血清瘦素水平及胰岛素抵抗的相关性。 资料与方法
1. 临床资料:选择武汉市普爱医院2005年1月至2012年12月就诊的86例PCOS患者为观察组,以及同期就诊的100例非PCOS健康体检者为对照组。观察组年龄22~38岁,平均(28.3±9.2)岁;对照组年龄21~39岁,平均(28.6±9.4)岁;两组年龄比较,差异无统计学意义(P>0.05)。测量患者身高和体重,并计算BMI,其中BMI≥25 kg/m2为肥胖,BMI<25 kg/m2为非肥胖。86例PCOS患者中,肥胖患者44例,非肥胖者42例;100例对照中,肥胖患者45例,非肥胖者55例。
2. PCOS诊断标准:①存在排卵障碍,稀发排卵或未见排卵;②血液生化检测显示高雄性激素血症,且排除其他疾病可能导致者;③B超检查显示卵巢一侧或两侧各有10个以上直径为2~9 mm的卵泡;均排除肝肾功能异常、心脑血管疾病、糖尿病和近期使用激素类药物。
3. 血液相关指标检测[5, 6]:采集入组患者月经第2~5天内任意一天(闭经患者无限制)清晨、空腹静脉血,2 h内送实验室测定FPG、胰岛素和血清瘦素等指标,FPG采用自动血糖仪测定,胰岛素采用化学发光免疫法测定,血清瘦素采用ELISA测定。胰岛素抵抗指数(IR)=FPG×空腹胰岛素/22.5。
4. 治疗方法:PCOS患者随机分为A组和B组。A组43例,月经第3天口服达英-35(1片/次,1次/日,连续服用21 d,下次月经第3天继续服用第2个疗程);B组43例,口服二甲双胍(每次500 mg,3次/日,1个月为1个疗程)。两组患者均在完成3个疗程后给予促排卵治疗,月经第5天给予口服克罗米酚(每次50 mg,1次/日,连续服用5 d);月经第8天肌肉注射人绝经期促性腺激素(每次150 U,1次/日,5次为1个疗程,下1个疗程从下次月经第5天开始);记录患者排卵和妊娠情况,完成3个疗程后,评价临床疗效。
5. 统计学分析:应用SPSS 13.0软件分析数据,计量数据采用x±s表示,组间数据比较采用t检验;相关性分析采用logistic回归分析;P<0.05为差异有统计学意义。 结果
1. 血清瘦素及其代谢指标分析:两组间及组内肥胖患者瘦素水平明显高于非肥胖者,差异有统计学意义(t=12.032,P<0.001;t=6.847,P<0.001);肥胖患者BMI明显高于非肥胖者,差异有统计学意义(t=12.202,P<0.001;t=13.157,P<0.001);肥胖患者胰岛素水平明显高于非肥胖者,差异有统计学意义(t=6.294,P<0.001;t=14.402,P<0.001);肥胖患者与非肥胖者比较,FPG水平的差异无统计学意义(t=0.216,P=0.415;t=0.292,P=0.386);肥胖患者的IR明显高于非肥胖者,差异有统计学意义(t=5.284,P<0.001;t=23.041,P<0.001)。观察组瘦素水平明显高于对照组相应的肥胖或非肥胖患者,差异有统计学意义(t=12.531,P<0.001;t=6.352,P<0.001);观察组胰岛素水平明显高于对照组相应的肥胖或非肥胖患者,差异有统计学意义(t=11.907,P<0.001;t=12.351,P<0.001);观察组的IR明显高于对照组相应的肥胖或非肥胖患者,差异有统计学意义(t=8.438,P<0.001;t=10.687,P<0.001)。见表 1。
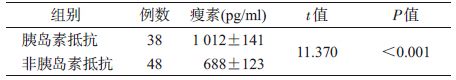
2. 血清瘦素水平分析:PCOS胰岛素抵抗与非胰岛素抵抗患者血清瘦素水平比较见表 2。
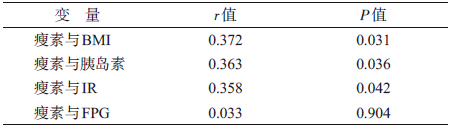
3. 血清瘦素与各指标相关性分析:PCOS患者血清瘦素与各指标的相关性见表 3。
4. 临床疗效分析:B组患者排卵率(58.1%,25/43)明显高于A组(27.9%,12/43),差异有统计学意义(χ2=8.017,P=0.005);B组患者妊娠率(25.6%,11/43)明显高于A组(9.3%,4/43),差异有统计学意义(χ2=3.957,P=0.047)。 讨论
PCOS患者若持续无排卵,则会使子宫内膜过度增生,从而增加子宫内膜癌的风险[7]。大量研究表明[8, 9, 10],胰岛素抵抗在PCOS的形成和进展过程中起着重要作用,但其具体作用机制尚未明确。瘦素是由脂肪组织分泌的一种蛋白质类激素,其在下丘脑-垂体-性腺轴代谢性信号的调节中发挥重要作用,与肥胖、胰岛素表达和高雄激素水平有密切关系,可影响生殖功能;其水平可随BMI值减小而下降,本研究结果表明瘦素与BMI呈正相关同文献报道[11]。有文献认为PCOS患者血清瘦素明显升高,且肥胖患者高于非肥胖者[12]。本研究结果也显示肥胖PCOS患者血清瘦素明显高于非肥胖PCOS患者。PCOS患者机体外周组织可对胰岛素起拮抗作用,引起高胰岛素血症发生,血清瘦素和胰岛素间可能存在互相调节作用,胰岛素可促进瘦素分泌,而瘦素的分泌与胰岛素的分泌相平行,从而形成一种互助关系,共同参与PCOS的进展。
本研究结果表明,PCOS患者中不论肥胖患者还是非肥胖者,其血清瘦素和胰岛素水平均明显高于相同体重的健康妇女(P<0.05)。logistic回归分析显示,PCOS患者血清瘦素水平与BMI、胰岛素和IR呈正相关,表明瘦素水平与胰岛素抵抗有明显关系,高瘦素水平可影响瘦素信号传导和破坏脂肪-胰岛素轴,导致机体代谢紊乱,发生高胰岛素血症,并产生严重的恶性循环[13]。PCOS不孕症患者的临床治疗结果表明,二甲双胍治疗者排卵率和妊娠率明显提高,可增加其受孕率,可能是二甲双胍具有抑制肝糖原分解为葡萄糖,提高外周组织对胰岛素的敏感性,从而达到改善卵巢排卵能力,最终提高妊娠率[14]。PCOS不孕症患者应加强瘦素和胰岛素检测,对两指标水平明显升高者,可给予二甲双胍治疗,从而提高临床妊娠成功率。
总之,血清瘦素与BMI、胰岛素和IR存在明显相关性,在PCOS的形成和进展过程中发挥重要作用,可作为诊断PCOS的辅助手段,但由于其在PCOS进展中的作用机制尚未明确,还有待进一步研究。通过二甲双胍调节外周组织对胰岛素的敏感性,可有效提高PCOS不孕症患者排卵率和妊娠率,值得临床应用。
[本研究为2004年武汉市卫生局基金(武卫[2004]241)资助]
| [1] Gong CX,Li YC,Wu D,et al. Research progress on nosogenesis of polycystic ovary syndrome and adolescent polycystic ovary [J]. Chin J Pediatrics,2012,50(6):535-541. (in Chinese)巩纯秀,李豫川,吴迪,等. 多囊卵巢综合征发病机制研究及青春期多囊卵巢综合征研究进展[J]. 中华儿科杂志,2012,50(6):535-541. |
| [2] Sang M,Hu M,Li W,et al. New research progress on insulin and kaohsiung hormones of polycystic ovary syndrome [J]. J Endocrine Surg,2011,5(6):711-717. (in Chinese)桑敏,胡敏,李威,等. 胰岛素与多囊卵巢综合征高雄激素血症的新研究进展[J]. 中华内分泌外科杂志,2011,5(6):711-717. |
| [3] Dayer D,Nikbakht R,Kadkhodai EM. Comparison of leptin concentrations between infertile women with polycystic ovary syndrome and fertile women [J]. Iran J Reprod Med,2013,11(12):1033-1034. |
| [4] Li GH,Fan L,Zhang L,et al. Clinical characteristics and perinatal outcomes of non-overweight/obese pregnant women with polycystic ovary syndrome [J]. National Med J Chin,2011,91(39):328-330. (in Chinese)李光辉,范玲,张莉,等. 非超重/肥胖多囊卵巢综合征合并妊娠孕妇的临床特点及围产结局[J]. 中华医学杂志,2011,91(39):328-330. |
| [5] Jin HL,Wang XJ. Research progress of polycystic ovary syndrome with insulin,leptin and androgen [J]. Fudan Unive J Med Sci,2010,37(2):236-242. (in Chinese)金华良,王兴娟. 胰岛素、瘦素、雄激素与多囊卵巢综合征发病机制研究进展[J]. 复旦学报:医学版,2010,37(2):236-242. |
| [6] Zhao QH,Shi H,Yang J,et al. Correlation between ultrasound parameters and hormone level in patients with polycystic ovary and polycystic ovary syndrome[J]. Chin J Genl Pract,2014,13(1):127-131. (in Chinese)赵庆红,石华,杨菁,等. 多囊卵巢与多囊卵巢综合征的超声特征和激素水平相关性分析[J]. 中华全科医师杂志,2014,13(1):127-131. |
| [7] Zou YJ, Yang J,Yin TL. Research progress on aetiology of polycystic ovary syndrome [J]. Chin J Obstet Gynecol,2012,47(1):64-66. (in Chinese)邹宇洁,杨菁,尹太郎. 多囊卵巢综合征病因学的研究进展[J]. 中华妇产科杂志,2012,47(1):64-66. |
| [8] Chakrabarti J. Serum leptin level in women with polycystic ovary syndrome:correlation with adiposity,insulin,and circulating testosterone[J]. Ann Med Health Sci Re,2013,3(2):191-196. |
| [9] Li L,Lee KJ,Choi BC,et al. Relationship between leptin receptor and polycystic ovary syndrome[J]. Gene,2013,527(1):71-74. |
| [10] Xie YN,Wang L,Ma RX. Differences in endocrine and metabolic parameters in polycystic ovary syndrome patients with and without subclinical hypothyroidism[J]. Chin J Endocrinol Metab,2014,30(3):204-207. (in Chinese)谢艳妮,王娈,马瑞欣. 多囊卵巢综合征伴或不伴亚临床甲状腺功能减退症患者内分泌代谢指标差异研究[J]. 中华内分泌代谢杂志,2014,30(3):204-207. |
| [11] Xi J, Sun DW,Zhang M,et al. Research on the correlation between insulin resistance and serum preptin in polycystic ovary syndrome [J]. Chin J Clinicans,2011,5(3):143-145. (in Chinese)奚杰,孙大伟,张敏,等. 多囊卵巢综合征患者血清preptin与胰岛素抵抗相关性研究[J]. 中华临床医师杂志,2011,5(3):143-145. |
| [12] Li J,Xu C, Zhang HJ, et al. Association of obesity and hyperandrogenemia with insulin resistance in women with polycystic ovary syndrome [J]. Chin J Endocrinol Metab,2011,27(9):209-211. (in Chinese)李晋,徐呈,张惠杰,等. 多囊卵巢综合征患者肥胖和高雄激素血症与胰岛素抵抗的相关性[J]. 中华内分泌代谢杂志,2011,27(9):209-211. |
| [13] Jeon YE,Lee KE,Jung JA,et al. Kisspeptin,leptin,and retinol- binding protein 4 in women with polycystic ovary syndrome [J]. Gynecol Obstet Invest,2013,75(4):268-274. |
| [14] Yuan J. Efficacy of weight loss training and oral intake of metformin in obese women with polycystic ovary syndrome [J]. J Endocrine Surg,2014,8(3):112-114. (in Chinese)袁晶. 减重训练及口服二甲双胍对肥胖型多囊卵巢综合征的疗效[J]. 中华内分泌外科杂志,2014,8(3):112-114. |
 2014, Vol. 35
2014, Vol. 35