文章信息
- 杨涤, 赵红心, 郜桂菊, 魏凯, 张俐, 韩宁, 肖江, 李鑫, 王芳, 梁洪远, 张伟, 吴亮. 2014.
- Yang Di, Zhao Hongxin, Gao Guiju, Wei Kai, Zhang Li, Han Ning, Xiao Jiang, Li Xin, Wang Fang, Liang Hongyuan, Zhang Wei, Wu Liang. 2014.
- HIV/AIDS手术切口愈合与CD4+T淋巴细胞计数的关系
- Relationship between CD4+ T lymphocyte cell count and the prognosis (including the healing of the incision wound) of HIV/AIDS patients who had undergone surgical operation
- 中华流行病学杂志, 2014, 35(12): 1333-1336
- Chinese Journal of Epidemiology, 2014, 35(12): 1333-1336
- http://dx.doi.org/10.3760/cma.j.issn.0254-6450.2014.12.005
-
文章历史
- 投稿日期:2014-06-05
截止2011年底,我国存活HIV/AIDS约78万人[1]。随着HIV感染者逐渐增加,其并发外科疾病也越来越多,手术风险的评估及预后已引起关注。本研究旨在通过分析北京地坛医院5年来HIV/AIDS手术病例,评价手术预后及切口愈合情况与CD4+T淋巴细胞计数的关系。 材料与方法
1. 研究对象:以北京地坛医院2008年1月至2012年12月进行手术治疗的234例HIV/AIDS住院患者为研究对象,所有患者均经省级疾病预防控制中心(CDC)确证为抗HIV-1(+)。
2. 研究方法及相关定义:采用回顾性分析的方法,对患者年龄、性别、发现抗HIV(+)时间、手术前CD4+T淋巴细胞计数、是否为急诊手术、手术部位、切口分类、术后切口愈合级别、切口感染情况、术后并发症及预后进行分析。采用单克隆免疫荧光抗体染色技术,应用流式细胞仪测定外周血CD4+T淋巴细胞计数。所有患者均经严密的术前评估,除外手术禁忌症。切口分类:Ⅰ类为清洁切口,Ⅱ类为可能污染的切口,Ⅲ类为污染切口。切口愈合等级:甲级为愈合优良;乙级为愈合欠佳,但未化脓;丙级为切口化脓,需切开引流。
3. 统计学分析:应用SPSS 17.0软件进行统计学分析。计量正态分布资料用x±s表示,偏态分布资料用M(QR)表示。偏态资料采用Wilcoxon 秩和检验,计数资料采用χ2检验,多组等级资料比较采用Kruskal-Wallis H检验,等级资料的相关分析采用Spearman相关分析。P<0.05为差异有统计学意义。 结果
1. 基本情况:共有234例患者,男性125例,女性109例,性别比为1.15 ∶ 1,年龄9~67(36.17±11.56)岁。发现抗HIV(+)时间为0~204个月。所有患者均于术前1周内检测了CD4+T淋巴细胞计数,CD4+T淋巴细胞计数为14~1 468 cell/μl,M=388.50(230.25~516.75)cell/μl。其中23.93%(56/234)患者CD4+T淋巴细胞计数<200 cell/μl。
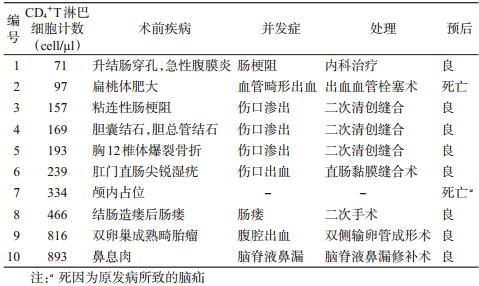
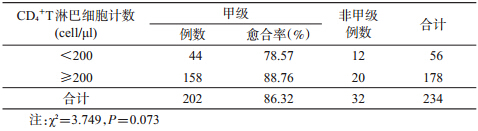
2. 手术情况及预后:急诊手术7.26%(17/234)。涉及23个手术器官,48种疾病。所有患者中,最多为肛肠科手术(24.36%,57/234),其次为妊娠剖宫产术(23.50%,55/234);其余还包括颅脑、颜面五官、肝胆、胃肠、脊柱四肢等部位手术。4.27%(10/234)出现术后并发症,其处理情况及预后见表 1。术后出现并发症与未出现并发症患者的CD4+T淋巴细胞计数(cell/μl)分别为216(142.0~553.5)和396(239.5~541.5),差异无统计学意义(P=0.194),两组患者感染HIV的时间分别为7.5(0.875~36.0)个月和12(2~48)个月,差异无统计学意义(P=0.332)。切口分类:Ⅰ类切口占21.37%(50/234),Ⅱ类切口占 49.57%(116/234),Ⅲ类切口占29.06%(68/234)。切口愈合级别:甲级占86.32%(202/234),乙级占11.97%(28/234),丙级占1.71%(4/234)。甲级与乙、丙级愈合的CD4+T淋巴细胞计数差异无统计学意义(P=0.081)。不同CD4+T淋巴细胞计数水平的患者切口甲级愈合率差异无统计学意义(P=0.073),见表 2。
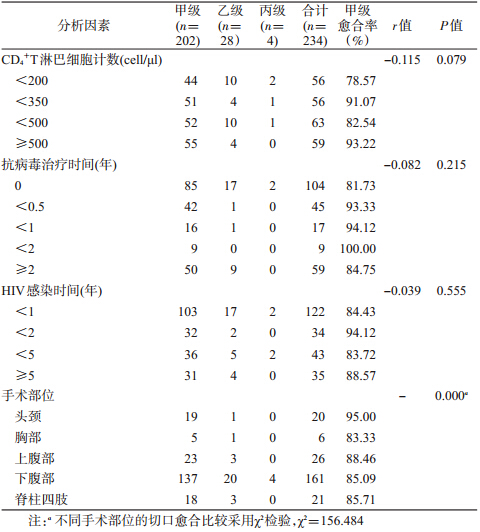
3. HIV/AIDS相关因素与手术切口愈合率的关系:手术切口愈合情况与CD4+T淋巴细胞计数水平、抗病毒治疗时间长短、HIV感染时间无明显相关性(P>0.05)。不同手术部位的切口愈合情况差异有统计学意义(P<0.05),见表 3。
随着高效抗反转录病毒治疗的实施,HIV/AIDS存活期逐渐延长,其合并外科疾病的人数也明显增多,大部分需要手术解决,其中一部分需要急诊手术[2, 3, 4, 5, 6]。目前这类患者在寻求手术治疗时遇到了诸多困难:其中很大原因是部分医生对患者进行手术存在顾虑,除担心医护人员的HIV职业暴露外,还担心患者术中或术后感染,影响手术效果,或增加患者感染率及死亡率,而不愿施行手术。
本研究显示,234例手术患者病变部位广泛,疾病种类较多,仅内科治疗不能解决所有问题,具有较严重的手术适应症。所有患者中,最多为肛肠科手术,这与目前我国的HIV感染途径以男男性行为传播比例的上升有关[1],易出现肛周尖锐湿疣、肛周脓肿有关。其次为妊娠剖宫产术,显示较多的HIV/AIDS有生育需求。为减少分娩过程中的母婴传播机会,尽可能采取剖宫产术[7]。
CD4+T淋巴细胞计数<200 cell/μl意味着机体处于极低的免疫状态,进入艾滋病阶段,易出现多种机会性感染及严重的HIV 相关并发症[7, 8]。本研究中的患者CD4+T淋巴细胞计数M仅为388.5 cell/μl,近1/5的患者CD4+T淋巴细胞计数<200 cell/μl,最少的1例仅为14 cell/μl,但术后极少数患者出现并发症。死亡病例中,1例因血管畸形出血,另1例因严重颅高压脑疝,均与低CD4+T淋巴细胞计数无直接关系。出现术后并发症与未出现术后并发症的患者,其CD4+T淋巴细胞计数水平差异无统计学意义, 提示手术预后不能以CD4+T淋巴细胞计数水平预测。本研究显示,Ⅱ类和Ⅲ类切口占绝大部分,而大部分切口为甲级愈合,丙级愈合仅4例(1.71%),总体术后预后良好。多项研究显示,对HIV/AIDS施行手术,其中CD4+T淋巴细胞计数最低为1 cell/μl,术后均未出现严重并发症及机会性感染[9, 10, 11, 12]。来自撒哈拉以南的Meta分析结果也显示,尚不能证实HIV感染者进行手术可能会增加切口感染率[13]。目前,低CD4+T淋巴细胞计数对切口愈合及死亡率是否存在影响尚有争议[14, 15, 16],本研究显示,不同CD4+T淋巴细胞计数水平的切口甲级愈合率差异无统计学意义(P>0.05)。评价HIV/AIDS的免疫水平及感染时间和抗病毒治疗时间的长短等相关因素与手术切口愈合情况也无明显相关性,因此,这些指标并不能作为手术禁忌症进行术前评价。但不同的手术部位,其切口的愈合情况可能不同,统计结果显示,头颈部手术甲级愈合率更高,而下腹部多为丙级愈合,可能与切口污染相关。
| [1] Ministry of Health of the People's Republic of China, The United Nations Joint Programme on HIV/AIDS,WHO. Estimation for HIV/AIDS epidemic situation in China,2011[EB/OL]. (2012-01-29)[2014-10-05]. (in Chinese)中华人民共和国卫生部,联合国艾滋病规划署,世界卫生组织. 2011年中国艾滋病疫情估计[EB/OL]. (2012-01-29)[2014-10-05]. http://ncaids.chinacdc.cn/fzdt/zxdd/201201/t20120129_1745902.htm. |
| [2] Liu BC, Wang M,Song YZ,et al. Research on the risk factors of perioperative for the patients with HIV/AIDS[J]. Chin J Crit Care Med,2012,32(1):14-17. (in Chinese)刘宝池,王盟,宋言峥,等. 艾滋病病毒感染患者围手术期脓毒症的危险因素及治疗研究[J]. 中国急救医学,2012,32(1):14-17. |
| [3] Li Z. Perioperctive management of HIV infection/AIDS in gynecological and obstetric patients[J]. J South Med Univ,2011,31(9):1629-1631. (in Chinese)李征. 妇产科HIV感染/AIDS患者的围手术期处理[J]. 南方医科大学学报,2011,31(9):1629-1631. |
| [4] Quintas RC, de França ER,de Petribú KC,et al. Treatment of facial lipoatrophy with polymethylmethacrylate among patients with human immunodeficiency virus/acquired immunodeficiency syndrome(HIV/AIDS):impact on the quality of life[J]. Int J Dermatol,2014,53(4):497-502. |
| [5] Gathogo EN,Hamzah L,Hilton R,et al. Kidney transplantation in HIV-positive adults: the UK experience[J]. Int J STD AIDS,2014,25(1):57-66. |
| [6] Deneve JL,Shantha JG,Page AJ,et al. CD4 count is predictive of outcome in HIV-positive patients undergoing abdominal operations[J]. Am J surg,2010,200(6):694-699. |
| [7] Hoffmann C,Rockstroh JK. HIV 2010[M]. Hamburg:Medizin Fokus Verlag,2010:131,456. |
| [8] Egger M,May M,Chene G,et al. Prognosis of HIV -1-infected patients starting HAART:a collaborative analysis of prospective studies[J]. Lancet,2002,360:119-129. |
| [9] Qian NP,Ma C,Feng XL,et al. Effect of T lymphocyte of subset on the postoperative complication of HIV/AIDS patients[J]. Chin J Coal Industry Med,2010,13(11):1663. (in Chinese)钱南平,马超,冯秀岭,等. T淋巴细胞亚群对HIV/AIDS患者术后并发症的影响[J]. 中国煤炭医学杂志,2010,13(11):1663. |
| [10] Zheng G,Cheng YD,Cun XH,et al. The characteristics of surgery on HIV/AIDS patients[J]. J Kunming Med University,2010(5):146-148. (in Chinese)郑刚,成永达,寸新华,等. 艾滋病患者外科手术80例体会[J].昆明医学院报,2010(5):146-148. |
| [11] Zhang LS,Cai C,Ni ZL,et al. Clinical analysis on 12 HIV/AIDS patients with otolaryngology surgery[J]. Chin J Exp Clin Infect Dis:Electronic ed,2012,6(2):147-150. (in Chinese)张立松,蔡超,倪志立,等. 12例耳鼻咽喉手术的HIV/AIDS患者临床分析[J]. 中华实验和临床感染病杂志:电子版,2012,6(2):147-150. |
| [12] Yang YL, Jiang R,He TW,et al. Retinal detachment in patients with acquired immunodeficiency syndrome[J]. Chin J Ocul Traum Occupat Eye Dis,2011,33(4):282-285. (in Chinese)杨娅玲,江睿,何太雯,等. AIDS/HIV感染合并视网膜脱离[J].中华眼外伤职业眼病杂志,2011,33(4):282-285. |
| [13] Kigera JW, Straetemans M, Vuhaka SK, et al. Is there an increased risk of post-operative surgical site infection after orthopaedic surgery in HIV patients?A systematic review and meta-analysis[J]. PLoS One,2012,7(8):e42254. |
| [14] Bates J,Mkandawire N,Harrison WJ. The incidence and consequences of early wound infection after internal fixation for trauma in HIV-positive patients[J]. J Bone Joint Surg Br,2012,94(9):1265-1270. |
| [15] Nagasaka S,Yazaki H,Ito H,et al. Effect of CD4+ T-lymphocyte count on hospital outcome of elective general thoracic surgery patients with human immunodeficiency virus[J]. Gen Thorac Surg,2011,59(11):743-747. |
| [16] Deneve JL,Shantha JG,Page AJ,et al. CD4 count is predictive of outcome in HIV-positive patients undergoing abdominal operations[J]. Am J Surg,2010,200(6):694-699.. |
 2014, Vol. 35
2014, Vol. 35