b Key Laboratory of Polymer Ecomaterials, Changchun Institute of Applied Chemistry, Chinese Academy of Sciences, Changchun 130022, China
During the last decades, people have tried to delay the aging of the skin and keep it healthy in various ways. The usual methods are deep cleaning, moisturization, and sun protection, etc. Facial rejuvenation is also regulated by exercise and diet. However, in most cases, these methods failed to efficiently repair the skin or eliminate wrinkles [1]. Therefore, in order to achieve the purpose of facial rejuvenation, modern plastic and aesthetic surgery have been applied to restore tissue defects or change the overall appearance [2]. In 19th century, paraffin was used as facial filler for the first time in skin repair, but this undegradable material caused embolism, granuloma, and many other complications and was finally abandoned as skin filler [3]. In 1981, collagen was officially approved by the United States Food and Drug Administration (FDA) as an injectable skin filler in the plastic and aesthetic surgery field [4]. In 2003, the emergence of hyaluronic acid filler brought a turning point for filler industry, and has guided a new direction for the development of biocompatible and permanent filler since then [5]. At present, there are many kinds of fillers on the market, mainly including fat, collagen, hyaluronic acid, calcium hydroxyapatite, etc. [3]. The problem is that traditional injectable dermal fillers are rapidly metabolized after injection, and therefore they can only perform a temporary repairing effect and require repeated injection. In the meantime, it may increase the risk of inflammation and other adverse effects because of the poor biocompatibility [5-7]. It is still a big challenge to develop dermal fillers with better properties.
Poly(lactic acid) (PLA) is a biocompatible material with excellent mechanical strength, easy processability, and good biodegradability [8-11]. For these reasons, PLA has been widely used in tissue engineering, drug delivery, surgical sutures, and orthopedic repair material [12, 13]. In 2004, poly(L-lactic acid) (PLLA) was approved by the FDA for correction of facial fat atrophy associated with human immuno-deficiency virus (HIV) infection. It was because lactic acid derived from the degradation of PLLA can stimulate collagen formation, which is an important component of skin tissue [2]. It could supplement collagen that gradually loses with age, improve skin quality, and fill the dermatolysis and skin sag. The curative effect of collagen filling can last for two years [14, 15]. Unlike the previous dermal filler, PLLA has been favored in the beauty industry in recent years [16]. PLA is classified into poly(D-lactic acid) (PDLA), PLLA, racemic PLA, and meso-PLA (PDLLA) [17]. The chiral of material has an influential effect on the biological propety. For example, Sarasua et al. explored the effect on cell proliferation by co-culturing the L929 mouse fibroblasts and keratinocytes with PLLA and PDLA scaffold [18]. Interestingly, the results were totally different for different cell lines. L929 mouse fibroblasts proliferated better in PLLA than proliferated in PDLA, but keratinocytes proliferated better in PDLA. Wang et al. prepared three different chiral injectable methoxy poly(ethylene glycol) polyalanine (mPEG–PA) thermosensitive hydrogels, which were injected under the skin of rats to observe inflammation [19]. Studies showed that dextral polyalanine thermogel can induce a controllable level of inflammatory response. It is generally believed that the biocompatibility of L-lactic acid is better because of the lactic acid in organism is L-lactic acid. In the past, most of the biological applications were based on PLLA, and there were few studies on the application of PDLA and PDLLA in biomedical materials.
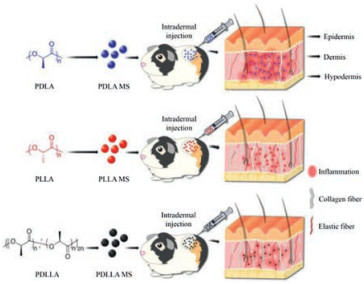
In order to explore the biological functions of different chiral PLA materials as fillers, we prepared chiral PLA microspheres with different particle sizes by emulsion-solvent evaporation method [20, 21], and injected them into the back skin of guinea pigs to observe the skin inflammation and collagen regeneration. The results of tissue sections after 30 days showed that PDLA microsphere (PDLA MS) cause high-grade inflammation and worst collagen regeneration. PDLLA microsphere (PDLLA MS) produced low-grade inflammation, and better effect of stimulating collagen regeneration. In contrast, PLLA microsphere (PLLA MS) produced the least inflammatory reaction in the skin, and the best effect of stimulating collagen regeneration. Moreover, it degraded slowly which could maintain the effect of promoting collagen regeneration for a long time. At the same time, the particle size did not affect the function of the microsphere. In conclusion, all experimental results show that PLLA MS performance is the best as a dermal filler.
The design concept was shown in Scheme 1. Three chiral PLA materials were prepared by lactide ring opening polymerization. First of all, proton nuclear magnetic resonance (1H NMR) was used to characterize the chemical structure of the polymer. In Fig. 1A, the peak at 1.78 ppm was the characteristic absorption peak of —CH3 in the PLA structural unit, and the peak at 5.34 ppm was attributed to -CH in the PLA structural unit. It proved that three kinds of PLA materials were successfully synthesized. Fig. 1B was the Fourier-transform infrared spectroscopy (FT-IR). The strongest peak is 1758 cm-1, which was the C=O stretching vibration peak. At 3508 cm-1, the peak was the -OH absorption peak of PLA. The peaks at 1455 cm-1 and 1384 cm-1 belonged to the —CH3. —CH stretching and bending vibration peaks were at 2980 cm-1 and 2950 cm-1. At 1214 cm-1, 1135 cm-1, and 1094 cm-1, there were the stretching vibration peak of C—O—C, indicating the existence of ester group. It also shows that the materials we synthesized is PLA. Due to the existence of chiral C atom in the middle of PLA chain, circular dichroism (CD) signal showed that PDLA produced a negative single circular dichroic peak at 240–245 nm, and a positive single circular dichroic peak 250 nm. The circular dichroism of PLLA was opposite to the circular dichroism of PDLA. PDLLA has intermediate value single circular dichroic peak, which proved that three kinds of chiral PLA produce different optical activity (Fig. 1C).
|
Download:
|
| Scheme 1. Schematic illustration of different chiral PLA microspheres used in dermal fillers. | |

|
Download:
|
| Fig. 1. Characterizations of three kinds of PLA with different chiralities. (A) 1H NMR spectra of PDLA, PLLA and PDLLA in deuterated chloroform (CDCl3). (B) FT-IR spectra of PDLA, PLLA and PDLLA. (C) CD spectra of PDLA, PLLA and PDLLA (0.5 mg/mL) in CDCl3 solution at room temperature. | |
The Mn value of polymer was measured by gel permeation chromatography (GPC) showing that the molecular weight of the three polymers was about 1.5 × 104 g/mol. The low polydispersity index (PDI) (PDI = Mw/Mn) also meant that the molecular weight distribution of the polymer was uniform (Table S1 in Supporting information). The above evidences proved that three PLA with different chiralities were successfully synthesized.
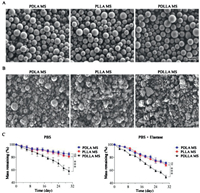
The morphology and particle size of microsphere were characterized by scanning electron microscopy (SEM). In Fig. 2A, the three kinds of microspheres had regular morphology and smooth surface, and the particle size of the microsphere was uniform, which were about 10 μm. The size of microsphere was controlled by stirring speed, PLA concentration, and volume ratio of poly(vinyl alcohol) (PVA): PLA. By controlling these conditions, we prepared three kinds of microspheres with different sizes for each PLA material. The morphology of 5 μm and 20 μm microsphere was shown in Figs. S1 and S2 (Supporting information).
|
Download:
|
| Fig. 2. Performance of three kinds of PLA microsphere. (A) Morphology of PDLA MS, PLLA MS, and PDLLA MS by SEM (10 μm). (B) Morphology of microsphere degraded for 30 days in the elastase group. (C) Microsphere degradation curve. The error bars represent the standard deviation (n = 3; *P < 0.05, **P < 0.01, ***P < 0.001, ns: not significant). | |
The morphology of microsphere degraded on Day 15 and Day 30 were shown in Fig. 2B and Figs. S3-S5 (Supporting information). In the elastase group, we found that three kinds of microspheres had shrinkage or fracture, PDLLA degradation was the most serious, most of the microspheres have agglomerated. In contrast, PDLA MS still maintain a complete shape. From the degradation curve, we can conclude that the mass remaining of PDLA MS, PLLA MS and PDLLA MS in phosphate buffered saline (PBS) group at the end of the degradation experiment were 85.1%, 81.3% and 58.4%, respectively. However, in the elastase group, the degradation rate of microsphere was faster, and the mass remaining of PDLA MS, PLLA MS, and PDLLA MS were 71.3%, 68.0% and 49.6% (Fig. 2C). The results showed that elastase could accelerate the degradation of microsphere. The degradation rate of PLLA was moderate, and PDLLA has the fastest degradation rate due to it is syndiotactic or atactic state which was easier to absorb water [22, 23]. Therefore, because PDLA was difficult to degrade and PDLLA was too fast to degrade, neither was suitable as a dermal filler. But in fact, the degradation of microsphere was not so fast by observing the skin tissue section. Kang et al. injected PLLA microsphere into the skin tissue on the back of mice, and it was observed that the mass of the microsphere decreased to 52.0% after 12 months [24]. This also shows that the degradation of PLA is very slow. Therefore, we suspected that in vitro degradation process, there will be a part of mass loss in each liquid exchange. Thus, the degradation curve showed a faster degradation rate.
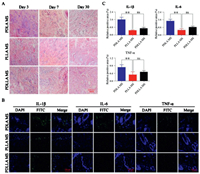
Hematoxylin and eosin (H&E) staining can be used to observe the local inflammatory response and determine the biocompatibility of PLA microsphere. In Fig. 3A, the results showed that no obvious histopathological damage or inflammatory reaction was detected three days after the treatment of PLLA MS, indicating excellent biocompatibility. As comparison, the inflammatory cells in the PDLA MS group were significantly more than those in the PDLLA MS and PLLA MS group, it proved that the inflammatory response in the skin injected by PDLA MS was stronger than that in PDLLA MS and PLLA MS group. After intradermal injection of three kinds of microspheres, immunofluorescence was used to detect the changes of inflammatory factors in tissues surrounding the injection site, including IL-1β, IL-6 and TNF-α. Three inflammatory cytokines were labeled with fluorescein isothiocyanate (FITC)- labeled secondary antibody, and the nucleus were stained with 4', 6-diamidino-2-phenylindole (DAPI). The expression level of IL-1β, IL-6 and TNF-α were evaluated by confocal laser scanning microscope (CLSM). As shown in Fig. 3B, on Day 3, the fluorescence signal of FITC in PDLA MS group was obviously strong, which showed the level of inflammatory response in tissues surrounding of the injected site with PDLA MS was significantly stronger than the level of inflammatory response which injected with PLLA MS or PDLLA MS. The semi-quantitative histograms in Fig. 3C showed that the expression levels of IL-1β, IL-6 and TNF-α around the injected site induced by PDLA MS were 3.2, 2.5 and 2.0 times higher than those of inflammatory factors induced by PLLA MS, and 2.3, 1.9 and 1.4 times higher than those induced by PDLLA MS, respectively. This finding was in consistence with the results in H & E staining, confirming that PLLA MS has good biocompatibility and thus is more suitable as dermal filler. As for PDLLA MS, it caused obvious inflammatory response shortly after the injection, while the inflammation was decreased or disappeared on Day 7 or Day 30 (Figs. S6 and S7 in Supporting information). Nevertheless, due to the rapid degradation rate of PDLLA MS, a large number of PDLLA MS were degraded and absorbed in the skin tissue on Day 30, which could not guarantee the long-term effect. And PDLA MS was easy to cause redness and swelling due to the strong inflammation after injection, the strong inflammation was not conducive to recover which was a major disadvantage of PDLA as a filler.
|
Download:
|
| Fig. 3. Histopathological and immunofluorescence assessments of inflammatory response. (A) H & E staining of the skin at the injection site of PDLA MS, PLLA MS, and PDLLA MS. (B) Immunofluorescence determination of skin inflammatory factors on Day 3 after microsphere injection. Green fluorescence showed FITC labeled inflammatory factors and blue fluorescence showed nuclei. (C) Semi-quantitative analyses of IL-1β, IL-6 and TNF-α. Data are presented as mean ± standard deviation (n = 3; *P < 0.05, **P < 0.01, ***P < 0.001, ns: not significant). | |
Collagen fibers are the most widely distributed fiber in connective tissue. In order to evaluate the effect of chiral PLA microspheres on collagen regeneration, collagen in the sections were observed under the optical microscope. Masson staining is an authoritative and classic technique for the staining of collagen fiber. It is frequently used in the analysis of collagen and smooth muscle. Collagen fiber, mucus, and cartilage were stained blue, and cytoplasm, muscle, cellulose, and glia were stained red. Nucleus was stained blue purple [25]. By using picrosirius red staining, different types of collagen fibers can be distinguished according to their specific forms and distinct colors under polarized light. For example, type Ⅰ collagen fibers are densely arranged showing red and yellow colors, while type Ⅲ collagen fibers exhibits threadlike structure in green color [26]. As shown in Figs. S8 and S9 (Supporting information), on three days and seven days after injection of microsphere, the collagen fibers were arranged neatly and densely, with no significant difference among the three groups. However, on Day 30, the collagen fibers in the control group were messy and sparse, and the collagen loss was very serious. On the contrary, the collagen fibers in the PLLA MS groups still remained normal arrangement. Meanwhile, the collagen density of PDLA MS and PDLLA MS group was significantly sparse than that of PLLA MS group. Nevertheless, the results of PDLLA MS group stimulation of collagen regeneration were better than that in PDLA MS group (Fig. 4A). Similar results were shown in optical photo of tissue sections stained with picrosirius red. Three days after injection, a large amount of type Ⅰ collagen fibers (red and yellow) were observed in all the groups (Fig. S10 in Supporting information). On Day 7, collagen fibers turned darker and sparse. Specifically, type Ⅲ collagen fiber was generated in PLLA MS group which was showing green in Fig. S11 (Supporting information). This difference was enlarged on Day 30, when new collagens were still much more than those in PDLLA MS and PDLA MS group (Fig. 4B). The content of type Ⅰ collagen in the PLLA group was still 84.7%, and type Ⅲ collagen was 15.1%. Total of type Ⅰ and type Ⅲ collagen were 1.4 times than the collagen in the PDLA group, and 1.1 times than the collagen in the PDLLA group (Fig. 4C). Which showed that PLLA MS has the most obvious effect on stimulating collagen regeneration, and it is indeed suitable for usage as dermal filler in comparison with the other two chiralities.

|
Download:
|
| Fig. 4. Histological analysis of collagen regeneration. (A) Masson staining and (B) Picrosirius red staining of the skin at the injection site of three kinds of PLA microsphere on Day 30. Type Ⅰ collagen fibers are red or yellow, type Ⅲ collagen fibers are green. (C) Semi-quantitative analyses of type Ⅰ and type Ⅲ collagen fibers. Data are presented as mean ± standard deviation (n = 3; *P < 0.05, **P < 0.01, ***P < 0.001, ns: not significant). | |
At the same time, to verify whether the microsphere with different particle sizes have any difference in collagen regeneration, we injected three chiral PLA microspheres with different particle sizes into the skin of guinea pigs in the same way. The particle sizes were 5 μm, 10 μm and 20 μm, respectively. It can be seen from Figs. S12-S15 (Supporting information), even though the particle size of microspheres is different, collagen regeneration in the PLLA MS group is still the best, and there is no significant difference between the different particle sizes of the same material. The results proved that particle size did not make a difference to the ability to stimulate collagen regeneration.
In summary, chiral injectable PLA microspheres with different particle sizes were prepared to verify the functions of dermal filler. After intradermal injection of these microspheres in guinea pigs, we found that PLLA MS groups showed less inflammation in the skin compared with PDLA MS and PDLLA MS groups, which could prove that PLLA MS has better biocompatibility than PDLA MS and PDLLA MS. Additionally, Masson staining and picrosirius red staining revealed that PLLA MS conducted the strongest stimulation toward the regeneration of collagen fibers in the skin, which is an important factor as a filler. Meanwhile, the effect of different microsphere sizes on collagen regeneration was not significant. Therefore, compared with PDLA MS and PDLLA MS, PLLA MS is a skin filling material with lower cost, lower side reaction, better filling effect and excellent collagen stimulating effect. Furthermore, PLLA MS can contain collagen and other substances that are beneficial to skin repair and collagen regeneration, which can be released slowly through PLLA degradation to achieve better cosmetic effect. In brief, PLLA MS is a valuable and superior dermal filler.
Declaration of competing interestThe authors declare no competing financial interest.
AcknowledgmentsThis research was financially supported by the National Natural Science Foundation of China (Nos. 51703012 and 51603204) and the Science and Technology Development Program of Jilin Province (No. 20190701004GH).
Appendix A. Supplementary dataSupplementary material related to this article canbefound, in the online version, at doi:https://doi.org/10.1016/j.cclet.2020.03.071.
| [1] |
T.K. Hamilton, Clin. Dermatol. 27 (2009) S13-S22. DOI:10.1016/j.clindermatol.2008.12.001 |
| [2] |
D. Vleggaar, Dermatol. Surg. 31 (2005) 1511-1518. DOI:10.2310/6350.2005.31236 |
| [3] |
T.C. Kontis, A. Rivkin, Facial Plast. Surg. 25 (2009) 67-72. DOI:10.1055/s-0029-1220645 |
| [4] |
T.C. Kontis, JAMA Facial Plast. Surg. 15 (2012) 1-7. |
| [5] |
E. Haneke, J. Cosmet. Dermatol. 5 (2006) 157-167. DOI:10.1111/j.1473-2165.2006.00243.x |
| [6] |
E.M. Ferneini, D. Beauvais, S.I. Aronin, J. Oral Maxillofac. Surg. 75 (2017) 160-166. DOI:10.1016/j.joms.2016.09.004 |
| [7] |
W.I. Choi, Y. Hwang, A. Sahu, et al., Biomater. Sci. 6 (2018) 2627-2638. DOI:10.1039/C8BM00524A |
| [8] |
J. Wang, W. Xu, S. Li, et al., J. Biomed. Nanotechnol. 14 (2018) 2102-2113. DOI:10.1166/jbn.2018.2624 |
| [9] |
Q. Chen, Y. Yang, X. Lin, et al., Chem. Commun. 54 (2018) 5369-5372. DOI:10.1039/C8CC02791A |
| [10] |
Y. Yu, Q. Xu, S. He, et al., Coord. Chem. Rev. 387 (2019) 154-179. DOI:10.1016/j.ccr.2019.01.020 |
| [11] |
S. Gao, G. Tang, D. Hua, et al., J. Mater. Chem.B: Mater. Biol. Med. 7 (2019) 709-729. DOI:10.1039/C8TB02491J |
| [12] |
J. Ding, J. Zhang, J. Li, et al., Prog. Polym. Sci. 90 (2019) 1-34. DOI:10.1016/j.progpolymsci.2019.01.002 |
| [13] |
S. Li, S. Dong, W. Xu, et al., Adv. Sci. 5 (2018) 1700527. DOI:10.1002/advs.201700527 |
| [14] |
C. Bartus, C. William Hanke, E. Daro-Kaftan, Dermatol. Surg. 39 (2013) 698-705. DOI:10.1111/dsu.12128 |
| [15] |
D. Vleggaar, Plast. Reconstr. Surg. 118 (2016) 46S-54S. |
| [16] |
G.J. Moyle, L. Lysakova, S. Brown, et al., HIV Med. 5 (2004) 82-87. DOI:10.1111/j.1468-1293.2004.00190.x |
| [17] |
P. Van Wouwe, M. Dusselier, E. Vanleeuw, et al., ChemSusChem 9 (2016) 907-921. DOI:10.1002/cssc.201501695 |
| [18] |
J.R. Sarasua, N. Lopez-Rodriguez, E. Zuza, et al., J. Mater. Sci-Mater. M. 22 (2011) 2513-2523. DOI:10.1007/s10856-011-4425-1 |
| [19] |
Y. Wang, Z. Jiang, W. Xu, et al., ACS Appl. Mater. Interfaces 11 (2019) 8725-8730. DOI:10.1021/acsami.9b01872 |
| [20] |
W. Zhang, W. Xu, C. Ning, et al., Biomaterials 181 (2018) 378-391. DOI:10.1016/j.biomaterials.2018.07.051 |
| [21] |
H. Zhang, J. Xu, Drug Deliv. 23 (2016) 248-253. DOI:10.3109/10717544.2014.909909 |
| [22] |
S.H. Lee, I.Y. Kim, W.S. Song, Macromol. Res. 22 (2014) 657-663. DOI:10.1007/s13233-014-2107-9 |
| [23] |
F. Iñiguez-Franco, R. Auras, G. Burgess, et al., Polymer 99 (2016) 315-323. DOI:10.1016/j.polymer.2016.07.018 |
| [24] |
S.W. Kang, E.R. Cho, O. Jeon, et al., J. Biomed. Mater. Res. Part B: Appl. Biomater. 80B (2007) 253-259. DOI:10.1002/jbm.b.30591 |
| [25] |
Y.Y. Guo, C. Xu, Y. Fang, et al., Mol. Carcinog. 58 (2019) 1481-1491. DOI:10.1002/mc.23029 |
| [26] |
T.R. Kwon, J. Seok, J.H. Jang, et al., Eur. J. Pharm. Biopharm. 105 (2016) 69-74. DOI:10.1016/j.ejpb.2016.05.014 |
 2021, Vol. 32
2021, Vol. 32 

