b ARC Centre of Excellence in Convergent Bio-Nano Science and Technology, Monash Institute of Pharmaceutical Sciences, Monash University, Parkville, VIC 3052, Australia
Resorbable polymers, also named as biodegradable polymers, are a class of polymers that serve a function, and then are gradually biodegraded, metabolized and eliminated under in vivo chemical or enzymatic action in the body [1-5]. Resorbable polymers can be classified into natural polymers (cellulose, starch, chitin, proteins and etc.) and synthetic polymers (saturated aliphatic polyesters, polypropylene fumarate, polyanhydrides, polyorthoesters, poly-phosphazene, their copolymers and etc.) [6-12]. Resorbable natural polymers have attracted many attentions in the field of tissue engineering because they are economical, readily available and non-toxic. However, it should be noted that resorbable natural polymers have many formulation problems such as instability and irreproducibility [13], which limit their application. Resorbable synthetic polymers are modified natural polymers or completely synthesized polymers from a synthetic monomer. Resorbable synthetic polymers have also attracted many attentions in the field of tissue engineering due to their advantages such as the capability to be tailored to have a wide range of properties, predictable lot-to-lot uniformity, controllable formation and mechanical properties, and long shelf time. However, the advantages of resorbable synthetic polymers such as chemical residues in the products and potential toxicity limit their application in the field of tissue engineering.
Resorbable polymers have been widely applied to prepare many types of biomedical materials devices/such as sutures, drug carriers and bone repair devices. In human body, the resorbable polymer can be degraded into small fragments with time. Therefore, these resorbable materials/devices are especially good for in vivo implantation because no secondary surgery is required and immunological reaction is minimized. The resorbable polymer materials/devices can be almost used in every subfield of tissue engineering such as wound closure, orthopedics, dentistry, cardiovascular surgery, bowel surgery, urology, and nerve repair.
One of promising resorbable polymer materials/devices is resorbable polymer nanofiber-based materials/devices, which have high surface-to-volume ratio and often have a porous structure with excellent pore interconnectivity. These structures are suitable for growth and development of different types of cells, which demonstrate their great potential for application in tissue regeneration. Nanofibers were defined as fibers with diameters below 1 μm [14, 15]. Many nanofiber fabrication techniques have been developed such as splitting of bicomponent fibers [16], melt-blowing [17], physical drawing [18], flash-spinning [19], gel (dry-wet) spinning [20], air jet spinning [21], phase separation [22], self-assembling [23], solvent dispersion [24], centrifugal spinning [25], hydrothermal [26], and electrospinning [27]. Among all these techniques, electrospinning is the most applied method due to its advantages such as cheap instruments, simple fabrication, low requirements to materials, capability for industrial productions [28].
Due to the huge advantages of both resorbable polymers and electrospun nanofibers, resorbable polymer electrospun nano-fibers (RPENs) have been widely applied in the field of tissue engineering [29, 30]. In this paper, we will mainly introduce RPENs for tissue engineering. Firstly, the electrospinning technique and electrospun nanofiber architectures are briefly introduced. Sec-ondly, the application of RPENs in the field of tissue engineering is mainly reviewed. Finally, the advantages and disadvantages of RPENs for tissue engineering are discussed.
2. Electrospinning technique and electrospun nanofiber architecturesThe history of electrospinning can be traced back to seventeen century. William Gilbert described the deformation and ejection of a liquid droplet when a piece of electrically charged amber was approaching near the liquid droplet [31]. In 1887, Charles Vernon Boys constructed an electrospinning apparatus comprised of "a small dish, insulated and connected with an electrical machine" [32]. He discovered that fibers could be drawn from a variety of liquid materials (beeswax, shellac, gutta-percha, sealing-wax and collodion) on the edge of the dish. The electrospinning process was firstly patented by John Francis Cooley in 1900 [33] and 1902 [34], and by William James Morton in 1902 [35]. Significant develop-ment of electrospinning started by Anton Formhals, who applied at least 22 patents on electrospinning technique from 1930 to 1944 [36-38]. To better understand the theoretical underpinning of electrospinning, Sir Geoffrey Ingram Taylor developed a mathe-matical model to analyze the shape of the deformation cone that was formed by the liquid droplet under an applied electric field [39]. The deformation cone was lately known as Taylor cone. With the development of nanotechnology, in the early 1990s some research groups reported that a number of organic polymers can be electrospun into nanofibers [40-42]. Especially, D.H. Reneker popularized the name of electrospinning [42, 43]. Since 1995, the theoretical and application researches of electrospinning have been increasing exponentially every year [38, 44, 45].
In a typical electrospinning process [46], a sufficiently high voltage is generally applied to a liquid droplet of polymer solutions or polymer melts, and then the droplet is stretched to form a Taylor cone and a stable liquid jet is ejected from the cone tip because the electrostatic repulsion overcomes the surface tension. Nanofibers are formed when the solvent evaporates or the melt solidifies during the liquid jet travels through the air, and are collected on an electrically grounded target to form electrospun nanofibrous membranes (ENMs) [47]. During the travels, the molecules in the fibers are highly stretched and form high orientation along the fiber axis, which have been prove recently by polarized FT-IR spectroscopy and polarized Raman spectroscopy [48-50]. The high molecular orientation also provides the excellent mechanical performance of electrospun nanofibers [51, 52].
The standard laboratory setup of electrospinning technique generally consists of three major modules (Fig. S1 in Supporting information): (i) a spinneret module which is typically consisted of a syringe loaded into a syringe pump. The syringe pump is comprised of a motor control system and a syringe pump control; (ii) a high voltage power generator; and (iii) an electrically grounded target/collector such as a Ti alloy stick loaded in a constant speed electric mixer. A polymer solution or polymer melt is put into the syringe and the liquid jet is ejected from the syringe needle tip at a constant speed by the syringe pump [53]. A sufficiently high voltage produced by the power generator is connected to the syringe needle, and then a Taylor cone is formed and a stable liquid jet is ejected from the cone tip. Nanofibers are formed during the jet travels through the air. Finally, the grounded target/collector collects the nanofibers to form ENMs on the surface of the target/collector [54].
Because the production of standard laboratory setup cannot satisfy the requirements of industrial application, many scaling-up multiple-jet electrospinning techniques have been developed such as multiple-needle electrospinning [55], needleless rotating spinneret electrospinning (ball spinneret, cylinder spinneret, cone spinneret, beaded chain spinneret, disc spinneret, spiral coil spinneret and etc.) [56], needleless stationary spinneret electro-spinning (magnet field-assisted electrospinning, gas-blowed bubble electrospinning, conical wire coil spinneret electrospin-ning, plate edge spinneret electrospinning, bowl spinneret electro-spinning and etc.) [56]. These developments provide the scaling-up possibility of ENM fabrication and can promote the industrial application of electrospinning techniques and their products.
The electrospinning process and its products can be affected by many factors [57-59]: (i) polymer properties such as polymer species, polymer architecture and molecular weight and its distribution; (ii) solution properties such as solvent species, polymer concentration, viscosity, conductivity, elasticity, surface tension and electric potential; (iii) spinneret shape and size such as syringe needle gauge, disc diameter and thickness; (iv) shape and size of the grounded collector/target such as rod, plate, disk and liquid; (v) electrospinning operational parameters such as the distance from the spinneret to the collector/target, the operational speed of spinneret and collector/target, syringe pump speed and electrical potential; (vi) ambient parameters such as air velocity in the chamber, humidity and temperature.
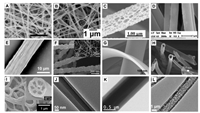
The products of electrospinning techniques, ENMs, can be classified into many types depending on different classification methods. Based on the chemical composition, electrospun nano-fibers can be classified into inorganic [60, 61], organic [62-64], carbonaceous [65, 66], and inorganic-organic hybrid nanofibers [67]. Based on the nanofiber shape, electrospinning nanofibers can be classified into round nanofibers [68], beaded nanofibers [69], porous nanofibers [70], side-by-side nanofibers [57], grooved nanofibers [71], nanograin nanofibers [72], nanobelt nanofibers [73], hollowed nanofibers [74, 75], multichannel nanofibers [76], bilayer core-shell nanofibers [67, 77, 78], trilayer core-shell nano-fibers [79, 80], and complex nanofibers such as porous core-shell nanofibers [81] (Fig. 1). Based on the orientation of nanofibers, ENMs can be classified into ENMs consist of random-distributed nanofibers [82], aligned nanofibers [82, 83], crimped nanofibers [80, 84] and etc. Based on the difference of the collector, the products can be classified into plate ENMs, layer-by-layer stacked films [85, 86], electrospun nanofibrous balloon ENMs [68], electro-spun nanofibrous bundles [87], twisted nanofibrous bundles [88] and etc.
|
Download:
|
| Fig. 1. Typical electrospun nanofiber shapes. (A) Round nanofibers [68], (B) beaded nanofibers [69], (C) porous nanofibers [70], (D) side-by-side nanofibers [57], (E) grooved nanofibers [71], (F) nanograin nanofibers [72], (G) nanobelt nanofibers [73], (H) hollowed nanofibers [74], (I) multichannel nanofibers [76], (J) bilayer core-shell nanofibers [67], (K) trilayer core-shell nanofibers [79] and (L) porous core-shell nanofibers [81]. (A–I) are SEM images and (J–L) are TEM images. Reprinted with permission [57, 68-73, 81]. Copyright 2011, 2012, 2013, 2014, 2015, 2016, Elsevier Publisher. Reprinted with permission [74]. Copyright 2016, Wiley Publisher. Reprinted with permission [76]. Copyright 2015, RSC Publisher. Reprinted with permission [67, 79]. Copyright 2014, 2015, ACS Publisher. | |
So far, ENMs have been extensively explored in the fields of tissue engineering [89-95], drug delivery [96-100], energy storage [101-106], food science [107-109], filtration [110-113], hydrogel [114-116], sponges [117-120], sensors [121-124], wall-less reactor [125], catalyst [126-128], responsive fibers and their actuators [129-132], oil/water separation [133-137], superhydrophilic/ superhydrophobic membranes [138-140], reinforcements [141, 142], etc. The interested readers may consult these reviews or articles for details.
3. Application of resorbable polymer electrospun nanofibers for tissue engineeringAmong the different fabrication techniques for scaffolds in tissue engineering [143, 144], electrospinning is given priority because it possesses unique properties such as high surface-to-volume ratio, porosity, stability, permeability and morphological similarity to that of extra cellular matrix. RPENSs have been widely used in every subfield of tissue engineering. In this section, the application of RPENSs in the field of tissue engineering is reviewed and discussed. Though many nanofiber types of electrospun nanofibers have been developed (Fig. 1), only round nanofibers (most of the literatures in below section) and core-shell nanofibers [145-149] have been applied in tissue engineering until now.
3.1. Bone tissue engineeringBone is an essential supportive rigid organ in the human body [150]. It serves to support and protect the various organs, to produce blood cells, to act as mineral reservoir for calcium and maintains acid–base balance, and to enable human mobility. Natural bone consists of about 70 wt% hydroxyapatite nanocrystals and 30 wt% collagen fibrils [151]. Bone defects may cause decreased mobility, chronic pain, depression, sleep loss, and limitation in quotidian activities [152]. Bone defect repair is a major challenge in orthopedics, dentistry, and cranio-facial surgery. In current clinical treatments of bone defects, autologous bones or commercial artificial bones are implanted into the defect sites and effective treatment efficacy is obtained. However, autologous bones have several disadvantages including limited autologous bone availability, the need for additional surgery, the formation of donor site bone defects, possible blood loss and infection, impracticability for osteoporosis patients and etc. Commercial artificial bones also have many disadvantages including poor biomechanical strength, low shaping ability, excessive osteoconduction and etc. Therefore, many novel scaffolds such as 3D printing artificial bones [153] and RPEN scaffolds (RPENSs) have been developed for bone tissue engineering.
A large number of RPENSs have been developed for bone regeneration by using natural and synthetic resorbable polymers such as chitosan, collagen, alginate, PCL, PLA, PLGA, and their mixtures with other substances [154, 155]. Bone tissue engineering involves scaffolds, cells and growth factors to promote the regeneration of fractured or damaged bones with efficient mineralization. The ideal bone repair scaffolds have suitable mechanical properties and appropriate osteogenic differentiation ability. Therefore, bioactive substances such as inorganics (hy-droxyapatite and etc.) and/or growth factors (bone morphogenetic protein-2 and etc.) have been applied to be combined with RPENSs for bone regenerations. The application of RPENSs for bone tissue engineering can be classified into three types: (i) Bioactive substances are loaded into the nanofibers. Generally, bioactive substances are mixed with polymers and then the mixed polymer solution is applied for the electrospinning process. The bioactive substances are uniformly distributed into the nanofibers. The bioactive substances can be gradually delivered at the implanta-tion sites in the human body with the degradation of RPENSs. It is especially useful for the long-term treatment of bone injury. This is the most explored way to fabricate biomaterials for bone tissue engineering. Typical examples include hydroxyapatite-blended chitosan RPENSs [156], hydroxyapatite-blended collagen RPENSs [157], hydroxyapatite-blended gelatin RPENSs [158], hydroxyapa-tite-blended poly(lactic acid) RPENSs [159]. For the bioactive substance, nanoparticle encapsulation prior to the electrospinning processs is an efficient way to increase their stability. (ii) Bioactive substances are immobilized onto the nanofibers. RPENSs are firstly fabricated by the electrospinning process and then the bioactive substances are immobilized onto the RPENSs [160]. Ngiam et al. [161] prepared nano-hydroxyapatite on PLGA and PLGA/collagen nanofibers by a chemical deposition method. The fabricated RPENSs had a positive modulation on early osteoblast capture on the scaffolds. Cho et al. [162] prepared BMP-2 immobilized PLLA RPENSs inspired by polydopamine for bone regeneration. BMP-2 is immobilized on PLLA RPENSs by polydopamine-mediated chemi-cal modification. (iii) The bioactive substances are encapsulated into nano- and micro-materials prior to scaffolds fabrication. The encapsulation can increase the stability of the bioactive sub-stances. Li et al. [163] prepared BMP-2-cencapsulated bovine serum albumin nanoparticles, and then the mixture solution of the nanoparticles, dexamethasone, and polymers was applied to prepare RPENSs for bone repair. Ding et al. [163] developed a RPENS-microbeads alternating multilayer scaffolds for bone repair. Stem cells and BMP2 are simultaneously loaded into the microbe-ads. The composite scaffold showed an outstanding osteogenic effect in vitro and in vivo. (iii) Bioactive substances are encapsulat-ed by RPENSs. RPENs are fabricated into a balloon shape and the bioactive substances are encapsulated into the balloon-shape RPENs. Sun et al. [68] designed a balloon-shape P(DLLA-CL) RPENS for the treatment of vertebral compression fractures (Fig. 2). The RPENSs can be inflated by injecting calcium phosphate cement to restore the height of fractured vertebral body. Moreover, the shortcomings of calcium phosphate cement such as water-induced collapsibility and cement leakage could be prevented. Further-more, their team comprehensively compared the in vitro and in vivo behaviors of the balloon-shape RPENS for the treatment of vertebral compression fractures [164]. The balloon-shape RPENS could satisfy the clinical needs and had good biodegradability and bioavailability. These researches showed the RPENS had a promising potential for the clinical application for the treatment of vertebral compression fractures.

|
Download:
|
| Fig. 2. Balloon-shape P(DLLA-CL) RPENS for the treatment of vertebral compression fractures. The left images showed the moulds and the RPENSs. The middle image showed the mechanical properties of naural bones, natural bones with CPC injection, natural bones with PMMA injection, and natural bones with balloon insertion and CPC injection. The right image showed the burst pressure measurements of RPENS. Reprinted with permission [68]. Copyright 2013, Elsevier Publisher. | |
3.2. Cartilage tissue engineering
Cartilage is a resilient and smooth elastic tissue. It includes a rubber-like padding that covers and protects the ends of long bones at the joints, a structural component of the nose, the bronchial tubes, the rib cage, the ear, the intervertebral discs and etc. Cartilage tissue has a limited capacity for spontaneous repair potential because of its avascular nature, insufficient number of chondrocytes and low mitotic activity [165]. Therefore, tissue engineering offers a promising alternative material for the treatment of the injured cartilage. The treatment also required a high standard to the applied biomaterials.
Until now, some research works have focused on the develop-ment of 2D RPENSs for the restoration of injured cartilages. Shafiee et al. [166] developed poly(vinyl alcohol)/polycaprolactone (PVA/PCL) nanofibrous scaffolds seeded with rabbit bone marrow-mesenchymal stem cell (BM-MSC) for cartilage tissue engineering. The in vitro and in vivo behaviors were comprehensively assessed. The animal studies showed the RPENS had improved healing ability compared with untreated control. It suggested the RPENS could serve as a suitable scaffold for cartilage regeneration. Articular cartilage has a complex structure, which increases the difficulty of cartilage repair. McCullen et al. [167] fabricated trilaminar composite electrospun scaffolds to mimic the structural organization and mechanical properties of cartilage's collagen fibrillar network. The results demonstrated that the scaffolds had in vitro cartilage formation ability and superior mechanical properties to homogenous scaffolds. Nanofibrous membranes generally exhibit a relatively small pore size and require techniques such as multilayering or the inclusion of sacrificial fibers to enhance cellular infiltration. Garrigues et al. [168] compared multilayer to single-layer electrospun poly(ε-caprolac-tone) (PCL) scaffolds for cartilage tissue engineering and studied the effect of the incorporation of cartilage-derived matrix into the PCL fibers on chondrogenesis by human adipose-derived stem cells (hASCs). The results demonstrated that multilayer electrospun scaffolds could enhance homogeneous cell seeding and the inclusion of cartilage-derived matrix could stimulate chondro-genesis-related bioactivity. To study the effect of combining collagen and electrospun nanofibers on osteochondral regenera-tion, Zhang et al. [169] studied the combination of collagen and electrospun poly-L-lactic acid nanofibers synergistically promotes osteochondral regeneration. Compared with collagen scaffold, the collagen-nanofiber scaffold showed fast subchondral bone emer-gence and better cartilage formation. The immobilization of bioactive substances onto nanofiber surface is a promising method to increase the ability of cartilage formation. Piai et al. [170] developed a chemical immobilization method of chondroitin sulfate at the surface of nanofiber. The immobilized scaffolds showed lower roughness, higher hydrophilicity, and a highly effective ability for human articular chondrocytes phenotypic stability.
3.3. Neural tissue engineeringCommon 2D electrospun nanofibrous membrane is not enough to mimic the 3D structure of cartilage. Several works have explored the possibility of 3D complex scaffolds for cartilage repair. Zheng et al. [171] fabricated different 3D shapes of electrospun gelatin/polycaprolactone scaffolds and studied the in vivo behaviors for cartilage formation. Different 3D shaped scaffolds showed differ-ent in vivo behaviors. Moreover, the results demonstrated high PCL content was unfavourable for 3D cartilage regeneration. Chen et al. [172] developed a 3D porous scaffolds with or without cross-linking by hyaluronic acid based on electrospun gelatin/PLA nanofibers (Fig. 3). The 3D scaffold with cross-linking could enhance cartilage repair and might be a promising scaffold for cartilage tissue regeneration.

|
Download:
|
| Fig. 3. Schematic of 3D scaffolds preparation based on electrospun nanofibrous scaffolds for cartilage tissue engineering. Reprinted with permission [172]. Copyright 2014, American Chemical Society. | |
Neural degeneration is a prevalent burden on the healthcare system in the world. Although various cell therapies and implants have been explored, nerve damage repair is still a challenging problem in this field [173]. Autograft implantation, as a gold standard, is limited by insufficient donor nerves from patients, surgery of the donor site, and possible functional impairment of the donor site. Neuroprosthetic devices implantation is limited by the presence of increased scarring and fibrosis, and insufficient nerve growth ability. Therefore, neural tissue engineering such as the application of RPENSs provides a promising way to improve nerve regeneration for nerve damage repair.
Both chemical and topographical factors of tissue engineering scaffolds are pivotal for nerve growth and regeneration. Some works focused on the loading of bioactive substances into electrospun nanofibrous scaffolds [174, 175] or on the application of aligned nanofibrous scaffolds [145, 176]. Recently, many works have started to focus on the development of scaffolds with both topographical effect and chemical factor (bioactive substances). Prabhakaran et al. [177] prepared aligned nanofibers of poly(3-hydroxybutyrate-co-3-hydroxyvalerate) (PHBV) and composite PHBV/collagen nanofibers. The aligned scaffold had higher nerve cell proliferation ability than random scaffold. Moreover, it elongated cell morphology with bi-polar neurite extensions, which are required for nerve regeneration. This work proved the aligned PHBV/collagen nanofibers are promising substrates for nerve repair. Hu et al. [178] prepared nerve growth factor/bovine serum albumin encapsulated aligned PCL nanofiber and studied its potential for nerve tissue engineering. The results showed the scaffold increased the length of neurites and directed neurites extension along the nanofiber axis. The results proved the aligned composite scaffold had a potential for nerve growth and regeneration. Zhu et al. [179] used electrospinning and electro-spraying technqiues to fabricate a novel nerve tissue engineered scaffold, which consisted of highly aligned PCL microfibrous framework and bioactive substance-embedded PLGA core-shell nanospheres (Fig. 4). The scaffold could increase the length of neurites and direct neurites growth along the fiber axis in the cell culture experiments of PC-12 and astrocyte cell lines. It suggested that the composite scaffold is an attractive way for guiding neural tissue growth and regeneration.

|
Download:
|
| Fig. 4. (A) Schematic of the key components of an ideal neural scaffold. (B) Schematic of electrospinning setup for aligned microfiberous membrane prepara-tion. (C) Schematic of electrospinning setup for random microfiberous membrane preparation. (D) Schematic of coaxial electrospaying setup for PLGA microsphers into PCL electrospun scaffolds. Reprinted with permission [179]. Copyright 2013, Elsevier Publisher. | |
Sometimes, resorbable polymers are difficult to be electrospun into nanofibers. In these types of cases, researchers can modify these polymers with an electrospinning agent. Poly(glycerol sebacate) (PGS) is a resorbable polymer and is difficult to be electrospun into nanofiber. Hu et al. [180] synthesized PGS-based copolymers with methyl methacrylate (MMA, an electrospinning agent) and then prepared PGS-PMMA RPENS. Blending gelatin into the PGS-PMMA RPENS showed good nerve regeneration potential. It provided a promising way to prepare electrospun scaffolds based on some special resorbable polymers that are difficult to be electrospun into nanofibers.
Electroactive biomaterials are an attractive substrate to provide electrical stimulation for nerve growth and regeneration. Zhang et al. [146] developed aligned core-sheath nanofibers with electrical conductivity and studied the synergistic effect of electrical stimulation and nerve growth factor on neuron growth.
The release of nerve growth factor could be increased by electrical stimulation. Moreover, the composite scaffolds under electrical stimulation could support PC12 neurite outgrowth and increase the percentage of neurite-bearing cells and the median neurite length. This suggested a promising way for nerve growth. and regeneration.
3.4. Vascular tissue engineeringCardiovascular diseases (atherosclerosis, coronary arterial restenosis and etc.) are major cause of morbidity and mortality in the world. Currently, autologous vascular grafts are mainly used in clinics, which are limited by possible thrombosis, limited sources, and the need for a second surgical procedure [181]. Artificial grafts such as polytetrafluoroethylene and Dacron Ⓡ have also been applied in the clinical treatment of vascular disease. However, they are not ideal for the treatment of small-diameter blood vessel disease (< 5 mm) [182]. Small-diameter blood vessel substitutes are a requisite for the replacement of coronary blood vessel. Electrospun scaffold-based vascular grafts have showed a promising possibility to meet the replacement requirements of small-diameter blood vessel [183].
The loading of bioactive substances in electrospun scaffolds is an attractive way for vascular tissue engineering. The loading ways can be classified into three types of methods: physical blending, chemical modification, core-shell fabrication and etc. Jia et al. [184] developed four different kinds of native proteins (collagen, gelatin, fibrinogen, and bovine serum albumin)-loaded polyurethane RPENSs and studied cell proliferation of smooth muscle cells on the scaffolds. The results suggested collagen and gelatin were promising proteins to fabricate electrospun nanofiber-based scaffolds for vascular tissue regeneration. Zhu et al. [185] prepared poly(ester-urethane) urea electrospun scaffolds and then the nanofiber surface was modified a arginine-glycine-aspartic (RGD) peptide. The prepared composite scaffold had a good potential application for vascular tissue engineering. Merkle et al. [147] used coaxial electrospinning technique to fabricate core-shell polyvinyl alcohol (PVA)/gelatin electrospun nanofibrous scaffolds. These scaffolds provided mechanical strength and biological properties facilitating the cell proliferation experiments of human umbilical vein endothelial cells and rat smooth muscle cells. Endothelial cells favored core-shell scaffolds, whereas smooth muscle cells favored pure gelatin scaffolds. These works could provide useful informa-tion for the development of electrospun scaffolds for vascular tissue engineering applications.
Topographical factor of tissue engineering scaffolds has also been considered for vascular tissue engineering. Zhong et al. [82] developed aligned PLGA/PCL scaffolds and studied cell prolifera-tion of smooth muscle cells on the scaffolds (Fig. S2 in Supporting information). Compared with random scaffolds, aligned scaffolds could maintain cell shapes of the cells. This work suggested the aligned scaffolds could be a promising candidate for vascular tissue regeneration. Similar works have also published and proved aligned scaffolds showed obvious advantages for vascular tissue regeneration [186, 187].
Cell incorporation into the electrospun scaffold has been explored for vascular tissue regeneration. Rayatpisheh et al. [188] combined cell sheet technology and electrospinning technology to fabricate circumferentially aligned tubular constructs of human aortic smooth muscle cells for vascular tissue engineering. This method improved cell sheet handling, results in rapid circumferential alignment of cells and introduction of an analogue to small-diameter blood vessel's internal elastic lamina. The engineered blood vessel media were structurally more close to the native vessel than previous work due to perthe presence of internal elastic lamina and showed a promising way for vascular tissue engineering.
3.5. Skin tissue engineeringSkin is the largest organ of vertebrates and is the first defense organ against insult from the environment. It protects vertebrates from mechanical injury, chemical hazards, and bacterial invasion. When an injury damages the skin's protective barriers, the body triggers a response called wound healing. Skin defects and necrosis can result from burns, tissue trauma, ultraviolet radiation, and chemical damage. Over 6 million patients suffer from severe burns and 3 hundred of thousand patients die every year in the world. Therefore, skin defect repair is an important clinical problem. The conventional treatments for skin defect repair include autografts, allografts, and xenografts [189, 190]. Autografts have a higher success rate but are limited by the autograft supply and possible donor site morbidity. Allografts and xenografts can be abundantly obtained, but are limited by high risk of immune rejection and disease transmis-sion. To resolve these problems, artificial tissue engineering skin substitutes have been developed such as Integra, alloderm, apligraf, and epicel and have been applied in clinics. Their major limitations include high cost and low mechanical strength [191, 192].
Ideal treatment biomaterials for skin regeneration should protect wounds from infections and fluid loss, should be stable until the natural extracellular matrix and the new skin are re-established, should have enough cellular and acellular components for vascularization and re-epitheliazation. Electrospun scaffolds can easily load angiogenic and/or vasculogenic factors, epidermal factors and molecules with anti-inflammatory and antimicrobial properties [148, 193-195]. Moreover, they can support the adhe-sion and spread of fibroblasts and keratinocytes [196]. They also can support growth and differentiation of mesenchymal stem cell into epidermal lineage [197]. Therefore, electrospun scaffolds have been widely studied for the treatment of skin defect repair.
Many natural and synthetic polymers have been developed as the matrix biomaterials for wound healing [198]. Typical applica-tion polymers include zein [199], hydroxyl derivatives of carboxylic acids [200], poly(lactic acid-co-glycolic acid) [189] and etc. Furthermore, their mixtures such as poly(caprolactone)/cellulose acetate [201], polyurethane/cellulose acetate/zein [202], poly (lactic acid)/polycaprolactone/cellulose acetate [203].
Some works focused on the development of RPENSs to increase cell growth and proliferation for wound healing. These types of works generally added some substances that can increase cell growth and proliferation into the RPENSs. Typical substances include plant extracts [204], dextran [201], gelatin [205], chitosan [206], gum tragacanth [207] and etc.
Many works focused on the loading of antibacterial substances into the RPENSs. The loading can be classified into two kinds of methods: surface immobilization onto the nanofibers and blending into the nanofibers. GhavamiNejad et al. [208] developed mussel-inspired electrospun scaffolds functionalized with size-controlled silver nanoparticles for wound dressing application. The size and amount of silver nanoparticles on the surface of nanofibers could be controlled with the minimum degree of aggregation. The electrospun scaffolds have controlled silver release and antibacterial activity. Furthermore, the rat skin repair experiments (Fig. S3 in Supporting information) showed Ag nanoparticles-immobilized RPENS had the best treatment effi-ciency compared with controls. Therefore, they showed great potential for skin wound healing. A majority of works mixed antibacterial drug with polymers and then prepared antibacterial drug-loaded RPENSs for wound healing application. The anti-bacterials drugs are distributed into the nanofibers and onto the nanofibers. Typical examples include silver nanoparticles [199], tetracycline hydrochloride drug [201], These scaffolds showed good cell cytocompatibility and good antibacterial performance. Therefore, they have good potential for biomaterial development of wound healing.
4. Summary and outlookElectrospinning technique is a simple and efficient technique for preparing nanometer polymer scaffolds. The application of electrospun nanofibrous scaffolds has attracted more and more attention in the field of tissue engineering. Besides the main application fields described in the above section 3, electrospun nanofibrous scaffolds have also been explored for skelet al muscle repair [149], corneal repair [209], hernia repair [210], intestinal repair [211] and etc.
RPENs have many advantages for their application in the field of tissue engineering. (i) high surface-to-volume ratios, (ii) easy fabrication and functionalization, (iii) low cost, (iv) controllability of nanofiber properties, (v) excellent biocompatibility and biodegradability. It should be noted there are still some short-comings of RPENs for the application in the field of tissue engineering. (i) The pore size of electrospun nanofibrous scaffolds is too small, which is not enough for cell infiltration growth. (ii) The mechanical properties of electrospun nanofibrous scaffolds are generally not ideal for hard tissue regeneration. Necessary consideration or treatments are needed for the application process.(iii) In vivo degradation performance of electrospun nanofibrous scaffolds is difficult to control. Further researches are needed to overcome these shortcomings. Shape and micro/nanomorpholo-gies of electrospun nanofibers might play important roles of the electrospun scaffolds in their application. Therefore, it is necessary to characterize the shapes and the surface morphologies of electrospun nanofibers using some important nanocharacteriza-tion technologies such as atomic force microscopy [212-214]. Furthermore, it will be beneficial for the development of RPENs in the field of tissue engineering to synthesize novel resorbable polymers [215, 216].
AcknowledgmentsThis work has been supported by research grants from the National Key R & D Program of China (No. 2016YFD0400202-8) and Scientific Instruments Development Project of the Science and Technology Commission of Shanghai Municipality (No. 17142202800).
Appendix A. Supplementary dataSupplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.cclet.2019.07.033.
| [1] |
N. Ashammakhi, A.M. Gonzalez, P. Törmälä, I.T. Jackson, Eur. J. Plastic Surg. 26 (2004) 383-390. DOI:10.1007/s00238-003-0568-8 |
| [2] |
B.L. Eppley, J. Craniofac. Surg. 8 (1997) 85-86. DOI:10.1097/00001665-199703000-00003 |
| [3] |
Q. Chen, Y. Yang, X. Lin, et al., Chem. Commun. (Camb.) 54 (2018) 5369-5372. DOI:10.1039/C8CC02791A |
| [4] |
Y. Yu, Q. Xu, S. He, et al., Coord. Chem. Rev. 387 (2019) 154-179. DOI:10.1016/j.ccr.2019.01.020 |
| [5] |
Y. Qiao, J. Wan, L. Zhou, et al., Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 11 (2019) e1527.
|
| [6] |
J. Zhang, Z. Xie, J. Yan, J. Zhong, Synthetic biodegradable polymers for bone tissue engineering, in: V.K. Thakur, M.K. Thakur, M.R. Kessler (Eds.), Handbook of Composites from Renewable Materials, Biodegradable Materials, vol 5, Wiley-Scrivener Publishing, Hoboken, 2010, pp. 355-375.
|
| [7] |
T. Kuang, F. Chen, L. Chang, et al., Chem. Eng. J. 307 (2017) 1017-1025. DOI:10.1016/j.cej.2016.09.023 |
| [8] |
X. Shi, P. Yang, X. Peng, et al., Polymer 170 (2019) 65-75. DOI:10.1016/j.polymer.2019.03.008 |
| [9] |
F. Chen, L. Wu, Z. Zhou, et al., Chin. Chem. Lett. 30 (2019) 197-202. DOI:10.1016/j.cclet.2018.10.007 |
| [10] |
G. Tang, R. Xiong, D. Lv, et al., Adv. Sci. 6 (2019) 1802342.
|
| [11] |
M. Ding, T. Zhang, H. Zhang, et al., Food Hydrocoll. 95 (2019) 326-335. DOI:10.1016/j.foodhyd.2019.04.052 |
| [12] |
M. Ma, J. Zhong, W. Li, et al., Soft Matter 9 (2013) 11325-11333. DOI:10.1039/c3sm51498f |
| [13] |
X. Liu, J. Aho, S. Baldursdottir, et al., Int. J. Pharm. 529 (2017) 371-380. DOI:10.1016/j.ijpharm.2017.06.086 |
| [14] |
E. Zdraveva, J. Fang, B. Mijovic, T. Lin, Electrospun nanofibers, in: G. Bhat (Ed.), Structure and Properties of High-Performance Fibers, Woodhead Publishing, Oxford, 2017, pp. 267-300.
|
| [15] |
D. Eaves, Handbook of Polymer Foams, Smithers Rapra Publishing, Shropshire, 2004, pp. 1-302.
|
| [16] |
C. Sun, D. Zhang, Y. Liu, R. Xiao, J. Appl. Polym. Sci. 93 (2004) 2090-2094. DOI:10.1002/app.20683 |
| [17] |
C.J. Ellison, A. Phatak, D.W. Giles, C.W. Macosko, F.S. Bates, Polymer 48 (2007) 3306-3316. DOI:10.1016/j.polymer.2007.04.005 |
| [18] |
P. Wang, Y. Wang, L. Tong, Light Sci. Appl. 2 (2013) e102.
|
| [19] |
L. Xia, P. Xi, B. Cheng, Mater. Lett. 147 (2015) 79-81. DOI:10.1016/j.matlet.2015.02.046 |
| [20] |
B. Ma, A. Qin, X. Li, C. He, Carbo. Polym. 97 (2013) 300-305. DOI:10.1016/j.carbpol.2013.04.080 |
| [21] |
A. Abdal-Hay, N.A.M. Barakat, J.K. Lim, Sci. Adv. Mater. 4 (2012) 1268-1275. DOI:10.1166/sam.2012.1382 |
| [22] |
G. Li, P. Li, C. Zhang, et al., Comp. Sci. Technol. 68 (2008) 987-994. DOI:10.1016/j.compscitech.2007.07.010 |
| [23] |
J.D. Hartgerink, E. Beniash, S.I. Stupp, Proc. Nat. Acad. Sci. U. S. A. 99 (2002) 5133-5138. DOI:10.1073/pnas.072699999 |
| [24] |
X. Li, G. Liu, Langmuir 25 (2009) 10811-10819. DOI:10.1021/la9013625 |
| [25] |
R.T. Weitz, L. Harnau, S. Rauschenbach, M. Burghard, K. Kern, Nano Lett. 8 (2008) 1187-1191. DOI:10.1021/nl080124q |
| [26] |
J. Yu, H. Yu, B. Cheng, X. Zhao, Q. Zhang, J. Photochem. Photobiol. A:Chem. 182 (2006) 121-127. DOI:10.1016/j.jphotochem.2006.01.022 |
| [27] |
N. Zhang, R. Qiao, J. Su, et al., Small 13 (2017)1604293. https://www.researchgate.net/publication/313320517_Recent_Advances_of_Electrospun_Nanofibrous_Membranes_in_the_Development_of_Chemosensors_for_Heavy_Metal_Detection
|
| [28] |
S. Gao, G. Tang, D. Hua, et al., J. Mater. Chem. B:Mater. Biol. Med. 7 (2019) 709-729. DOI:10.1039/C8TB02491J |
| [29] |
D.I. Braghirolli, D. Steffens, P. Pranke, Drug Discov. Today 19 (2014) 743-753. DOI:10.1016/j.drudis.2014.03.024 |
| [30] |
S. Sell, C. Barnes, M. Smith, et al., Polymer Int. 56 (2007) 1349-1360. DOI:10.1002/pi.2344 |
| [31] |
W. Gilbert, De Magnete Magnetcisque Corporibus, Et De Magno Magnete Tellure (on the Magnet, Magnetick Bodies Also, and on the Great Magnet the Earth; a New Physiology, Demonstrated by Many Arguments & Experiments), The Chiswick Press, Lodon, 1600.
|
| [32] |
C.V. Boys, Proc. Phys. Soc. London 9 (1887) 8. https://www.researchgate.net/publication/232951068_On_the_Production_Properties_and_some_suggested_Uses_of_the_Finest_Threads
|
| [33] |
J.F. Cooley, Patent, GB 06385, 1900.
|
| [34] |
J.F. Cooley, Patent, US 692631, 1902.
|
| [35] |
W.J. Morton, Patent, US 705691, 1902.
|
| [36] |
A. Formhals, Patent, US 1975504, 1934.
|
| [37] |
A. Formhals, Patent, US 2349950, 1944.
|
| [38] |
N. Tucker, J.J. Stanger, M.P. Staiger, H. Razzaq, K. Hofman, J. Eng. Fibers Fabr. 7 (2012) 63-73. |
| [39] |
G. Taylor, P. Roy, Soc. A:Math. Phys. 280 (1964) 383-397. |
| [40] |
J.P. Berry, Patent, US 5024789, 1991.
|
| [41] |
R.F. Valentini, T.G. Vargo, J.A. Gardella, P. Aebischer, Biomaterials 13 (1992) 183-190. DOI:10.1016/0142-9612(92)90069-Z |
| [42] |
J. Doshi, D.H. Reneker, Electrospinning process and applications of electrospun fibers, Industry Applications Society Annual Meeting, 1993., Conference Record of the 1993 IEEE (1993) 1698-1703. https://www.researchgate.net/publication/224663896_Electrospinning_Process_and_Applications_of_Electrospun_Fibers
|
| [43] |
G. Srinivasan, D.H. Reneker, Polym. Int. 36 (1995) 195-201. DOI:10.1002/pi.1995.210360210 |
| [44] |
S. Rafiel, S. Maghsoodloo, B. Noroozi, V. Mottaghitalab, A.K. Haghi, Cellul. Chem. Technol. 47 (2013) 323-338. |
| [45] |
M.L.F. Nascimento, E.S. Araujo, E.R. Cordeiro, A. HP de Oliveira, H. P de Oliveira, Recent. Pat. Nanotech. 9 (2015) 76-85. DOI:10.2174/187221050902150819151532 |
| [46] |
A.L. Yarin, S. Koombhongse, D.H. Reneker, J. Appl. Phys. 90 (2001) 4836-4846. DOI:10.1063/1.1408260 |
| [47] |
C. Ding, H. Fang, G. Duan, et al., RSC Adv. 9 (2019) 13608-13613. DOI:10.1039/C9RA02024A |
| [48] |
H. Yang, S. Jiang, H. Fang, et al., Spectrochim. Acta A 200 (2018) 339-344. DOI:10.1016/j.saa.2018.04.045 |
| [49] |
S. Jiang, D. Han, C. Huang, G. Duan, H. Hou, Mater. Lett. 216 (2018) 81-83. DOI:10.1016/j.matlet.2017.12.146 |
| [50] |
H. Xu, S. Jiang, C. Ding, et al., Mater. Lett. 201 (2017) 82-84. DOI:10.1016/j.matlet.2017.05.019 |
| [51] |
G. Duan, S. Liu, S. Jiang, H. Hou, J. Mater. Sci. 54 (2019) 6719-6727. DOI:10.1007/s10853-019-03326-w |
| [52] |
G. Duan, S. Liu, H. Hou, e-Polymers 18 (2018) 569.
|
| [53] |
S.R. Merritt, A.A. Exner, Z. Lee, H.A. von Recum, Adv. Eng. Mater. 14 (2012) B266-B278. https://www.researchgate.net/publication/260743269_Electrospinning_and_Imaging
|
| [54] |
M. Zhu, D. Hua, M. Zhong, et al., Colloid Interf. Sci. Commun. 23 (2018) 52-58. DOI:10.1016/j.colcom.2018.01.002 |
| [55] |
A. Varesano, R.A. Carletto, G. Mazzuchetti, J. Mater. Process. Technol. 209 (2009) 5178-5185. DOI:10.1016/j.jmatprotec.2009.03.003 |
| [56] |
H. Niu, T. Lin, J. Nanomater. 2012 (2012) 12.
|
| [57] |
D. Kai, S.S. Liow, X.J. Loh, Mater. Sci. Eng. C 45 (2014) 659-670. DOI:10.1016/j.msec.2014.04.051 |
| [58] |
W. Ma, M. Zhang, Z. Liu, C. Huang, G. Fu, Environ. Sci. Nano 5 (2018) 2909-2920. DOI:10.1039/C8EN00895G |
| [59] |
X. Shi, Z. Xu, C. Huang, Y. Wang, Z. Cui, Macromolecules 51 (2018) 2283-2292. DOI:10.1021/acs.macromol.8b00220 |
| [60] |
P. Panda, S. Ramakrishna, J. Mater. Sci. 42 (2007) 2189-2193. DOI:10.1007/s10853-007-1581-2 |
| [61] |
W. Ouyang, S. Liu, L. Zhao, et al., Compos. Commun. 9 (2018) 76-80. DOI:10.1016/j.coco.2018.06.006 |
| [62] |
Y. Feng, T. Xiong, S. Jiang, S. Liu, H. Hou, RSC Adv. 6 (2016) 24250-24256. DOI:10.1039/C5RA27676D |
| [63] |
A. Huang, X. Peng, L. Geng, et al., Polym. Test. 71 (2018) 101-109. DOI:10.1016/j.polymertesting.2018.08.027 |
| [64] |
M. Zhu, D. Hua, H. Pan, et al., J. Colloid Interf. Sci. 511 (2018) 411-423. DOI:10.1016/j.jcis.2017.09.101 |
| [65] |
G. Duan, H. Fang, C. Huang, S. Jiang, H. Hou, J. Mater. Sci. 53 (2018) 15096-15106. DOI:10.1007/s10853-018-2700-y |
| [66] |
S. Zhou, G. Zhou, S. Jiang, P. Fan, H. Hou, Mater. Lett. 200 (2017) 97-100. DOI:10.1016/j.matlet.2017.04.115 |
| [67] |
P. Zhang, X. Zhao, X. Zhang, et al., ACS Appl. Mater. Interfaces 6 (2014) 7563-7571. DOI:10.1021/am500908v |
| [68] |
G. Sun, D. Wei, X. Liu, et al., Nanomed. Nanotechnol. Biol. Med. 9 (2013) 829-838. DOI:10.1016/j.nano.2012.12.003 |
| [69] |
Q. Lin, Y. Li, M. Yang, Sensor. Actuat. B -Chem. 161 (2012) 967-972. DOI:10.1016/j.snb.2011.11.074 |
| [70] |
Y. Li, C.T. Lim, M. Kotaki, Polymer 56 (2015) 572-580. DOI:10.1016/j.polymer.2014.10.073 |
| [71] |
X. Wang, T. Wu, W. Wang, C. Huang, X. Jin, Mater. Sci. Eng. C 58 (2016) 750-756. DOI:10.1016/j.msec.2015.09.038 |
| [72] |
A. Katoch, G.J. Sun, S.W. Choi, J.H. Byun, S.S. Kim, Sensor. Actuat. B -Chem. 185 (2013) 411-416. DOI:10.1016/j.snb.2013.05.030 |
| [73] |
H. Fan, T. Zhang, X. Xu, N. Lv, Sensor. Actuat. B -Chem. 153 (2011) 83-88. DOI:10.1016/j.snb.2010.10.014 |
| [74] |
T.H. Le, Y. Yang, L. Yu, et al., J. Appl. Polym. Sci. 133 (2016) 43397.
|
| [75] |
G. Duan, A. Greiner, Macromol. Mater. Eng. 304 (2019) 1800669.
|
| [76] |
J. Jun, J.S. Lee, D.H. Shin, S.G. Kim, J. Jang, Nanoscale 7 (2015) 16026-16033. DOI:10.1039/C5NR03616J |
| [77] |
W. Ma, Z. Guo, J. Zhao, et al., Sep. Purif. Technol. 177 (2017) 71-85. DOI:10.1016/j.seppur.2016.12.032 |
| [78] |
W. Ma, Q. Zhang, S.K. Samal, et al., RSC Adv. 6 (2016) 41861-41870. DOI:10.1039/C6RA06224E |
| [79] |
D.G. Yu, X.Y. Li, X. Wang, et al., ACS Appl. Mater. Interfaces 7 (2015) 18891-18897. DOI:10.1021/acsami.5b06007 |
| [80] |
S. Jiang, G. Duan, E. Zussman, A. Greiner, S. Agarwal, ACS Appl. Mater. Interfaces 6 (2014) 5918-5923. DOI:10.1021/am500837s |
| [81] |
T.T.T. Nguyen, C. Ghosh, S.G. Hwang, N. Chanunpanich, J.S. Park, Int. J. Pharm. 439 (2012) 296-306. DOI:10.1016/j.ijpharm.2012.09.019 |
| [82] |
J. Zhong, H. Zhang, J. Yan, X. Gong, Colloids Surf. B -Biointerfaces 136 (2015) 772-778. DOI:10.1016/j.colsurfb.2015.10.017 |
| [83] |
X. Xi, Q. Ma, M. Yang, et al., J. Mater. Sci. Mater. Electron. 25 (2014) 4024-4032. DOI:10.1007/s10854-014-2124-7 |
| [84] |
J.H. He, H.Y. Kong, R.R. Yang, et al., Thermal Sci. 16 (2012) 1263-1279. |
| [85] |
D. Li, Y. Wang, Y. Xia, Adv. Mater. 16 (2004) 361-366. DOI:10.1002/adma.200306226 |
| [86] |
L. Liu, H. Bakhshi, S. Jiang, H. Schmalz, S. Agarwal, Macromol. Rapid Commun. 39 (2018) 1800082. https://www.researchgate.net/publication/324652453_Composite_Polymeric_Membranes_with_Directionally_Embedded_Fibers_for_Controlled_Dual_Actuation
|
| [87] |
Y. Zuo, F. Yang, J.G.C. Wolke, Y. Li, J.A. Jansen, Acta Biomater. 6 (2010) 1238-1247. DOI:10.1016/j.actbio.2009.10.036 |
| [88] |
Y. Zhou, J. Fang, X. Wang, T. Lin, J. Mater. Res. 27 (2012) 537-544. DOI:10.1557/jmr.2011.295 |
| [89] |
E. Ercolani, C. Del Gaudio, A. Bianco, J. Tissue. Eng. Regen. M. 9 (2015) 861-888. DOI:10.1002/term.1697 |
| [90] |
M.L. Muerza-Cascante, D. Haylock, D.W. Hutmacher, P.D. Dalton, Tissue Eng. Part B-Rev. 21 (2015) 187-202. DOI:10.1089/ten.teb.2014.0347 |
| [91] |
W. Zhao, W. Liu, J. Li, X. Lin, Y. Wang, J. Biomed. Mater. Res. Part B:Appl. Biomater. 103 (2015) 807-818. |
| [92] |
J. Kucinska-Lipka, I. Gubanska, H. Janik, M. Sienkiewicz, Mater. Sci. Eng. C 46 (2015) 166-176. DOI:10.1016/j.msec.2014.10.027 |
| [93] |
G.C. Ingavle, J.K. Leach, Tissue. Eng. Part B-Rev. 20 (2014) 277-293. DOI:10.1089/ten.teb.2013.0276 |
| [94] |
I. Woods, T.C. Flanagan, Expet. Rev. Cardiovasc. Ther. 12 (2014) 815-832. |
| [95] |
P. Li, Z. Shang, K. Cui, et al., Chin. Chem. Lett. 30 (2019) 157-159. DOI:10.1016/j.cclet.2018.01.037 |
| [96] |
X. Hu, S. Liu, G. Zhou, et al., J. Control. Release 185 (2014) 12-21. DOI:10.1016/j.jconrel.2014.04.018 |
| [97] |
N. Ashammakhi, I. Wimpenny, L. Nikkola, Y. Yang, J. Biomed. Nanotechnol. 5 (2009) 1-19. DOI:10.1166/jbn.2009.1003 |
| [98] |
G. Duan, A.R.R. Bagheri, S. Jiang, et al., Biomacromolecules 18 (2017) 3215-3221. DOI:10.1021/acs.biomac.7b00852 |
| [99] |
D. Hua, Z. Liu, F. Wang, et al., Carbohyd. Polym. 151 (2016) 1240-1244. DOI:10.1016/j.carbpol.2016.06.066 |
| [100] |
Z. Guo, G. Tang, Y. Zhou, et al., Carbohyd. Polym. 169 (2017) 198-205. DOI:10.1016/j.carbpol.2017.04.020 |
| [101] |
X. Shi, W. Zhou, D. Ma, et al., J. Nanomater. 16 (2015) 122. https://www.researchgate.net/publication/277227948_Review_Article_Electrospinning_of_Nanofibers_and_Their_Applications_for_Energy_Devices
|
| [102] |
H. Yang, S. Liu, L. Cao, S. Jiang, H. Hou, J. Mater. Chem. A:Mater. Energy Sustain. 6 (2018) 21216-21224. DOI:10.1039/C8TA05109G |
| [103] |
Z. Dong, S.J. Kennedy, Y. Wu, J. Power Sources 196 (2011) 4886-4904. DOI:10.1016/j.jpowsour.2011.01.090 |
| [104] |
B. Huang, X. Wang, H. Fang, S. Jiang, H. Hou, Mater. Lett. 234 (2019) 354-356. DOI:10.1016/j.matlet.2018.09.131 |
| [105] |
X. Gong, J. Yang, Y. Jiang, S. Mu, Prog. Chem. 26 (2014) 41-47. |
| [106] |
F. Zhao, X. Zhao, B. Peng, et al., Chin. Chem. Lett. 29 (2018) 1692-1697. DOI:10.1016/j.cclet.2017.12.015 |
| [107] |
B. Ghorani, N. Tucker, Food Hydrocol. 51 (2015) 227-240. DOI:10.1016/j.foodhyd.2015.05.024 |
| [108] |
A. Rezaei, A. Nasirpour, M. Fathi, Compr. Rev. Food Sci. Food Saf. 14 (2015) 269-284. DOI:10.1111/1541-4337.12128 |
| [109] |
J.A. Bhushani, C. Anandharamakrishnan, Trends Food Sci. Technol. 38 (2014) 21-33. DOI:10.1016/j.tifs.2014.03.004 |
| [110] |
D. Lv, R. Wang, G. Tang, et al., ACS Appl. Mater. Interfaces 11 (2019) 12880-12889. DOI:10.1021/acsami.9b01508 |
| [111] |
D. Lv, M. Zhu, Z. Jiang, et al., Macromol. Mater. Engin. 303 (2018)1800336.
|
| [112] |
M. Zhu, J. Han, F. Wang, et al., Macromol. Mater. Eng. 302 (2017) 1600353.
|
| [113] |
M. Zhu, R. Xiong, C. Huang, Carbohyd. Polym 205 (2019) 55-62. DOI:10.1016/j.carbpol.2018.09.075 |
| [114] |
Q. Ding, X. Xu, Y. Yue, et al., ACS Appl. Mater. Interfaces 10 (2018) 27987-28002. DOI:10.1021/acsami.8b09656 |
| [115] |
J. Han, K. Lu, Y. Yue, et al., Ind. Crop. Prod. 128 (2019) 94-107. DOI:10.1016/j.indcrop.2018.11.004 |
| [116] |
J. Han, Y. Yue, Q. Wu, et al., Cellulose 24 (2017) 4433-4448. DOI:10.1007/s10570-017-1409-4 |
| [117] |
S. Jiang, B. Uch, S. Agarwal, A. Greiner, ACS Appl. Mater. Interfaces 9 (2017) 32308-32315. DOI:10.1021/acsami.7b11045 |
| [118] |
J. Zhu, S. Jiang, H. Hou, S. Agarwal, A. Greiner, Macromol. Mater. Engin. 303 (2018) 1700615.
|
| [119] |
S. Jiang, S. Agarwal, A. Greiner, Angew. Chem. Int. Ed. 56 (2017) 15520-15538. DOI:10.1002/anie.201700684 |
| [120] |
S. Jiang, G. Duan, U. Kuhn, et al., Angew. Chem. Int. Ed. 56 (2017) 3285-3288. DOI:10.1002/anie.201611787 |
| [121] |
I.-D. Kim, A. Rothschild, Polym. Advan. Technol. 22 (2011) 318-325. DOI:10.1002/pat.1797 |
| [122] |
Z. Su, J. Ding, G. Wei, RSC Adv. 4 (2014) 52598-52610. DOI:10.1039/C4RA07848A |
| [123] |
K.Y. Hua, C.M. Deng, C. He, et al., Chin. Chem. Lett. 24 (2013) 643-646. DOI:10.1016/j.cclet.2013.04.033 |
| [124] |
Y. Qiao, C. Shi, X. Wang, et al., ACS Appl. Mater. Interfaces 11 (2019) 5401-5413. DOI:10.1021/acsami.8b19839 |
| [125] |
S. Jiang, V. Gruen, S. Rosenfeldt, et al., Research (2019) 4152536.
|
| [126] |
C. Jiang, J. Nie, G. Ma, RSC Adv. 6 (2016) 22996-23007. DOI:10.1039/C5RA27687J |
| [127] |
D.C. Higgins, R. Wang, M.A. Hoque, et al., Nano Energy 10 (2014) 135-143. DOI:10.1016/j.nanoen.2014.09.013 |
| [128] |
S.J. Guo, J. Bai, H.O. Liang, C.P. Li, Chin. Chem. Lett. 27 (2016) 459-463. DOI:10.1016/j.cclet.2015.12.029 |
| [129] |
S. Agarwal, S. Jiang, Y. Chen, Macromol. Mater. Engin. 304 (2019) 1800548.
|
| [130] |
S. Jiang, N. Helfricht, G. Papastavrou, A. Greiner, S. Agarwal, Macromol. Rapid Commun. 39 (2018) 1700838. https://www.researchgate.net/publication/323152103_Low-Density_Self-Assembled_Poly_N_-Isopropyl_Acrylamide_Sponges_with_Ultrahigh_and_Extremely_Fast_Water_Uptake_and_Release
|
| [131] |
K. Molnar, A. Jedlovszky-Hajdu, M. Zrinyi, S. Jiang, S. Agarwal, Macromol. Rapid Commun. 38 (2017) 1700147.
|
| [132] |
S. Jiang, F. Liu, A. Lerch, L. Ionov, S. Agarwal, Adv. Mater. 27 (2015) 4865-4870. DOI:10.1002/adma.201502133 |
| [133] |
W. Fu, Y. Dai, J. Tian, et al., Nanotechnology 29 (2018) 345607.
|
| [134] |
W. Ma, S.K. Samal, Z. Liu, et al., J. Membrane Sci. 537 (2017) 128-139. DOI:10.1016/j.memsci.2017.04.063 |
| [135] |
W. Ma, Q. Zhang, D. Hua, et al., RSC Adv. 6 (2016) 12868-12884. DOI:10.1039/C5RA27309A |
| [136] |
M. Zhang, W. Ma, S. Wu, et al., J. Colloid Interf. Sci. 547 (2019) 136-144. DOI:10.1016/j.jcis.2019.03.099 |
| [137] |
Z. Jiang, H. Zhang, M. Zhu, et al., J. Appl. Polym. Sci. 135 (2018) 45766.
|
| [138] |
W. Ma, M. Zhang, Z. Liu, et al., J. Membrane Sci. 570 (2019) 303-313. |
| [139] |
W. Ma, J. Zhao, O. Oderinde, et al., J. Colloid Interf. Sci. 532 (2018) 12-23. DOI:10.1016/j.jcis.2018.06.067 |
| [140] |
Z. Liu, W. Ma, M. Zhang, et al., J. Appl. Polym. Sci. 136 (2019) 47638.
|
| [141] |
Y. Chen, L. Sui, H. Fang, et al., Compos. Sci. Technol. 174 (2019) 20-26. DOI:10.1016/j.compscitech.2019.02.012 |
| [142] |
S. Jiang, Y. Chen, G. Duan, et al., Polym. Chem. 9 (2018) 2685-2720. DOI:10.1039/C8PY00378E |
| [143] |
J. Zhou, B. Zhang, X. Liu, et al., Carbohyd. Polym. 143 (2016) 301-309. DOI:10.1016/j.carbpol.2016.01.023 |
| [144] |
J. Zhong, G. Sun, D. He, Nanoscale 6 (2014) 12217-12228. DOI:10.1039/C4NR04296D |
| [145] |
W. Fu, Y. Dai, X. Meng, et al., Nanotechnology 30 (2019) 045602.
|
| [146] |
J. Zhang, K. Qiu, B. Sun, et al., J. Mater. Chem. B:Mater. Biol. Med. 2 (2014) 7945-7954. DOI:10.1039/C4TB01185F |
| [147] |
V.M. Merkle, P.L. Tran, M. Hutchinson, et al., Acta Biomater. 27 (2015) 77-87. DOI:10.1016/j.actbio.2015.08.044 |
| [148] |
G. Jin, M.P. Prabhakaran, D. Kai, S. Ramakrishna, Eur. J. Pharm. Biopharm. 85 (2013) 689-698. DOI:10.1016/j.ejpb.2013.06.002 |
| [149] |
L. Wang, Y. Wu, B. Guo, P.X. Ma, ACS Nano 9 (2015) 9167-9179. DOI:10.1021/acsnano.5b03644 |
| [150] |
T. Liu, K. Huang, L. Li, et al., Comp. Sci. Technol. 175 (2019) 100-110. DOI:10.1016/j.compscitech.2019.03.012 |
| [151] |
Y. Zhu, Y. Chen, G. Xu, et al., Mater. Sci. Eng. C 32 (2012) 390-394. DOI:10.1016/j.msec.2011.11.002 |
| [152] |
D. Wei, R. Qiao, J. Dao, et al., Small 14 (2018) 1800063.
|
| [153] |
N. Xu, X. Ye, D. Wei, et al., ACS Appl. Mater. Interfaces 6 (2014) 14952-14963. DOI:10.1021/am502716t |
| [154] |
J.H. Jang, O. Castano, H.W. Kim, Adv. Drug Deliv. Rev. 61 (2009) 1065-1083. DOI:10.1016/j.addr.2009.07.008 |
| [155] |
J.M. Holzwarth, P.X. Ma, Biomaterials 32 (2011) 9622-9629. DOI:10.1016/j.biomaterials.2011.09.009 |
| [156] |
M.E. Frohbergh, A. Katsman, G.P. Botta, et al., Biomaterials 33 (2012) 9167-9178. DOI:10.1016/j.biomaterials.2012.09.009 |
| [157] |
J. Venugopal, S. Low, A.T. Choon, T.S. Sampath Kumar, S. Ramakrishna, J. Mater. Sci. Mater. Med. 19 (2008) 2039-2046. DOI:10.1007/s10856-007-3289-x |
| [158] |
H.W. Kim, J.H. Song, H.E. Kim, Adv. Funct. Mater. 15 (2005) 1988-1994. DOI:10.1002/adfm.200500116 |
| [159] |
H.W. Kim, H.H. Lee, J.C. Knowles, J. Biomed. Mater. Res. A 79A (2006) 643-649. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_JJ029265946
|
| [160] |
G. Chen, Y. Lv, Curr. Pharm. Des. 21 (2015) 1967-1978. DOI:10.2174/1381612821666150302152704 |
| [161] |
M. Ngiam, S. Liao, A.J. Patil, et al., Bone 45 (2009) 4-16. DOI:10.1016/j.bone.2009.03.674 |
| [162] |
H.J. Cho, S.K. Madhurakkat Perikamana, J.H. Lee, et al., ACS Appl. Mater. Interfaces 6 (2014) 11225-11235. DOI:10.1021/am501391z |
| [163] |
S. Ding, L. Li, X. Liu, et al., Colloids Surf. B -Biointerfaces 133 (2015) 286-295. DOI:10.1016/j.colsurfb.2015.06.015 |
| [164] |
X. Liu, D. Wei, J. Zhong, et al., ACS Appl. Mater. Interfaces 7 (2015) 18540-18552. DOI:10.1021/acsami.5b04868 |
| [165] |
M. Kim, B. Hong, J. Lee, et al., Biomacromolecules 13 (2012) 2287-2298. DOI:10.1021/bm3005353 |
| [166] |
A. Shafiee, M. Soleimani, G.A. Chamheidari, et al., J. Biomed. Mater. Res. A 99A (2011) 467-478. https://www.researchgate.net/publication/51615287_Electrospun_nanofiber-based_regeneration_of_cartilage_enhanced_by_mesenchymal_stem_cells
|
| [167] |
S.D. McCullen, H. Autefage, A. Callanan, E. Gentleman, M.M. Stevens, Tissue Eng. Part A 18 (2012) 2073-2083. DOI:10.1089/ten.tea.2011.0606 |
| [168] |
N.W. Garrigues, D. Little, J. Sanchez-Adams, D.S. Ruch, F. Guilak, J. Biomed. Mater. Res. A. 102 (2014) 3998-4008. DOI:10.1002/jbm.a.35068 |
| [169] |
S. Zhang, L. Chen, Y. Jiang, et al., Acta Biomater. 9 (2013) 7236-7247. DOI:10.1016/j.actbio.2013.04.003 |
| [170] |
J.F. Piai, M.A. da Silva, A. Martins, et al., Appl. Surf. Sci. 403 (2017) 112-125. DOI:10.1016/j.apsusc.2016.12.135 |
| [171] |
R. Zheng, H. Duan, J. Xue, et al., Biomaterials 35 (2014) 152-164. DOI:10.1016/j.biomaterials.2013.09.082 |
| [172] |
W. Chen, S. Chen, Y. Morsi, et al., ACS Appl. Mater. Interfaces 8 (2016) 24415-24425. DOI:10.1021/acsami.6b06825 |
| [173] |
V. Chiono, C. Tonda-Turo, Prog. Neurobiol. 131 (2015) 87-104. DOI:10.1016/j.pneurobio.2015.06.001 |
| [174] |
E. Kijenska, M.P. Prabhakaran, W. Swieszkowski, K.J. Kurzydlowski, S. Ramakrishna, Eur. Polym. J. 50 (2014) 30-38. DOI:10.1016/j.eurpolymj.2013.10.021 |
| [175] |
K. Suzuki, H. Tanaka, M. Ebara, et al., Acta Biomater. 53 (2017) 250-259. DOI:10.1016/j.actbio.2017.02.004 |
| [176] |
J. Xie, W. Liu, M.R. MacEwan, P.C. Bridgman, Y. Xia, ACS Nano 8 (2014) 1878-1885. DOI:10.1021/nn406363j |
| [177] |
M.P. Prabhakaran, E. Vatankhah, S. Ramakrishna, Biotechnol. Bioeng. 110 (2013) 2775-2784. DOI:10.1002/bit.24937 |
| [178] |
J. Hu, L. Tian, M. Prabhakaran, X. Ding, S. Ramakrishna, Polymers 8 (2016) 54. https://www.researchgate.net/publication/295244750_Fabrication_of_Nerve_Growth_Factor_Encapsulated_Aligned_Polye-Caprolactone_Nanofibers_and_Their_Assessment_as_a_Potential_Neural_Tissue_Engineering_Scaffold
|
| [179] |
W. Zhu, F. Masood, J. O'Brien, L.G. Zhang, Nanomed. Nanotechnol. Biol. Med. 11 (2015) 693-704. DOI:10.1016/j.nano.2014.12.001 |
| [180] |
J. Hu, D. Kai, H. Ye, et al., Mater. Sci. Eng. C 70 (2017) 1089-1094. DOI:10.1016/j.msec.2016.03.035 |
| [181] |
F. Du, H. Wang, W. Zhao, et al., Biomaterials 33 (2012) 762-770. DOI:10.1016/j.biomaterials.2011.10.037 |
| [182] |
R.Y. Kannan, H.J. Salacinski, P.E. Butler, G. Hamilton, A.M. Seifalian, J. Biomed. Mater. Res. Part B: Appl. Biomater. 74B (2005) 570-581.
|
| [183] |
A. Hasan, A. Memic, N. Annabi, et al., Acta Biomater. 10 (2014) 11-25. DOI:10.1016/j.actbio.2013.08.022 |
| [184] |
L. Jia, M.P. Prabhakaran, X. Qin, D. Kai, S. Ramakrishna, J. Mater. Sci. 48 (2013) 5113-5124. DOI:10.1007/s10853-013-7359-9 |
| [185] |
T. Zhu, K. Yu, M.A. Bhutto, et al., Chem. Eng. J. 315 (2017) 177-190. DOI:10.1016/j.cej.2016.12.134 |
| [186] |
K.K. Sankaran, K.S. Vasanthan, U.M. Krishnan, S. Sethuraman, J. Tissue Eng. Regen. Med. 8 (2014) 640-651. DOI:10.1002/term.1566 |
| [187] |
L. Jia, M.P. Prabhakaran, X. Qin, S. Ramakrishna, J. Biomater. Appl. 29 (2014) 364-377. DOI:10.1177/0885328214529002 |
| [188] |
S. Rayatpisheh, D.E. Heath, A. Shakouri, et al., Biomaterials 35 (2014) 2713-2719. DOI:10.1016/j.biomaterials.2013.12.035 |
| [189] |
S.G. Kumbar, S.P. Nukavarapu, R. James, L.S. Nair, C.T. Laurencin, Biomaterials 29 (2008) 4100-4107. DOI:10.1016/j.biomaterials.2008.06.028 |
| [190] |
P.P. Bonvallet, B.K. Culpepper, J.L. Bain, et al., Tissue Eng. Part A 20 (2014) 2434-2445. DOI:10.1089/ten.tea.2013.0645 |
| [191] |
R.F. Pereira, C.C. Barrias, P.L. Granja, P.J. Bartolo, Nanomedicine 8 (2013) 603-621. DOI:10.2217/nnm.13.50 |
| [192] |
D.M. Supp, S.T. Boyce, Clin. Dermatol. 23 (2005) 403-412. DOI:10.1016/j.clindermatol.2004.07.023 |
| [193] |
A. Yari, H. Yeganeh, H. Bakhshi, J. Mater. Sci. Mater. Med. 23 (2012) 2187-2202. DOI:10.1007/s10856-012-4683-6 |
| [194] |
P. Losi, E. Briganti, C. Errico, et al., Acta Biomater. 9 (2013) 7814-7821. DOI:10.1016/j.actbio.2013.04.019 |
| [195] |
K.M. Guthrie, A. Agarwal, D.S. Tackes, et al., Ann. Surg. 256 (2012) 371-377. DOI:10.1097/SLA.0b013e318256ff99 |
| [196] |
M. B.-Min, G. Lee, S.H. Kim, et al., Biomaterials 25 (2004) 1289-1297. DOI:10.1016/j.biomaterials.2003.08.045 |
| [197] |
G. Jin, M.P. Prabhakaran, S. Ramakrishna, Acta Biomater. 7 (2011) 3113-3122. DOI:10.1016/j.actbio.2011.04.017 |
| [198] |
G.D. Mogoşanu, A.M. Grumezescu, Int. J. Pharm. 463 (2014) 127-136. DOI:10.1016/j.ijpharm.2013.12.015 |
| [199] |
U. Dashdorj, M.K. Reyes, A.R. Unnithan, et al., Int. J. Biol. Macromol. 80 (2015) 1-7. DOI:10.1016/j.ijbiomac.2015.06.026 |
| [200] |
E.I. Shishatskaya, E.D. Nikolaeva, O.N. Vinogradova, T.G. Volova, J. Mater. Sci. Mater. Med. 27 (2016) 165. https://www.researchgate.net/publication/308480851_Experimental_wound_dressings_of_degradable_PHA_for_skin_defect_repair
|
| [201] |
N. Liao, A.R. Unnithan, M.K. Joshi, et al., Colloids Surf. A:Physicochem. Eng. Asp. 469 (2015) 194-201. DOI:10.1016/j.colsurfa.2015.01.022 |
| [202] |
A.R. Unnithan, G. Gnanasekaran, Y. Sathishkumar, Y.S. Lee, C.S. Kim, Carbo. Polym. 102 (2014) 884-892. DOI:10.1016/j.carbpol.2013.10.070 |
| [203] |
N. Tuancharoensri, G.M. Ross, S. Mahasaranon, P.D. Topham, S. Ross, Polymer Int. 66 (2017) 1463-1472. DOI:10.1002/pi.5393 |
| [204] |
G. Jin, M.P. Prabhakaran, D. Kai, et al., Biomaterials 34 (2013) 724-734. DOI:10.1016/j.biomaterials.2012.10.026 |
| [205] |
E.J. Chong, T.T. Phan, I.J. Lim, et al., Acta Biomater. 3 (2007) 321-330. DOI:10.1016/j.actbio.2007.01.002 |
| [206] |
A.C. Alavarse, F.W. de Oliveira Silva, J.T. Colque, et al., Mater. Sci. Eng. C 77 (2017) 271-281. DOI:10.1016/j.msec.2017.03.199 |
| [207] |
M. Ranjbar-Mohammadi, S. Rabbani, S.H. Bahrami, M.T. Joghataei, F. Moayer, Mater. Sci. Eng. C 69 (2016) 1183-1191. DOI:10.1016/j.msec.2016.08.032 |
| [208] |
A. GhavamiNejad, A. Rajan Unnithan, A. Ramachandra Kurup Sasikala, et al., ACS Appl. Mater. Interfaces 7 (2015) 12176-12183. DOI:10.1021/acsami.5b02542 |
| [209] |
Í. Ortega, A.J. Ryan, P. Deshpande, S. MacNeil, F. Claeyssens, Acta Biomater. 9 (2013) 5511-5520. DOI:10.1016/j.actbio.2012.10.039 |
| [210] |
G.C. Ebersole, E.G. Buettmann, M.R. MacEwan, et al., Surg. Endosc. 26 (2012) 2717-2728. DOI:10.1007/s00464-012-2258-8 |
| [211] |
S.R. Son, R.A. Franco, S.H. Bae, Y.K. Min, B.T. Lee, J. Biomed. Mater. Res. Part B: Appl. Biomater. 101B (2013) 1095-1105.
|
| [212] |
C. Shi, Y. He, M. Ding, Y. Wang, J. Zhong, Trend. Food Sci. Technol. 87 (2019) 3-13. DOI:10.1016/j.tifs.2018.11.028 |
| [213] |
C. Shi, Y. He, M. Ding, Y. Wang, J. Zhong, Trend. Food Sci. Technol. 87 (2019) 14-25. DOI:10.1016/j.tifs.2018.11.027 |
| [214] |
C. Shi, C. Bi, M. Ding, et al., Food Hydrocoll. 93 (2019) 253-260. DOI:10.1016/j.foodhyd.2019.02.035 |
| [215] |
W. Zhang, M. Huang, H. Su, et al., ACS Central Sci. 2 (2016) 48-54. DOI:10.1021/acscentsci.5b00385 |
| [216] |
W. Zhang, X. Lu, J. Mao, et al., Angew. Chem. Int. Ed. 56 (2017) 15014-15019. DOI:10.1002/anie.201709354 |
 2020, Vol. 31
2020, Vol. 31 

