2. 南京医科大学附属苏州医院(苏州市立医院)心血管病中心, 苏州 215008;
3. 海军军医大学(第二军医大学)附属公利医院超声科, 上海 200135
2. Cardiovascular Disease Center, The Affiliated Suzhou Hospital of Nanjing Medical University (Suzhou Municipal Hospital), Suzhou 215008, Jiangsu, China;
3. Department of Ultrasound, Gongli Hospital, Naval Medical University (Second Military Medical University), Shanghai 200135, China
临床实践表明,三血管气管(three-vessel and trachea,3VT)切面是胎儿心脏超声检查不可或缺的重要切面。国际妇产超声学会(International Society of Ultrasound in Obstetrics and Gynaecology,ISUOG)推荐的胎儿心脏连续横向扫查技术,更是将3VT切面作为超声筛查圆锥动脉干畸形的主要切面[1]。在正常3VT切面上,动脉导管弓(ductus arteriosus arch,DAA)与主动脉弓呈“V”字征于气管左侧汇入降主动脉。3VT切面异常与胎儿心血管畸形密切相关,例如“U”字征提示可能存在右位主动脉弓和左位动脉导管[2-4];“V”字征位于气管右侧提示右位主动脉弓和右位动脉导管[2-4];“O”字征提示可能存在双主动脉弓等[5-6]。在临床实践中,某些心脏畸形在3VT切面上仅探及1条大动脉(弓部)和上腔静脉(短轴观),两者紧密排列呈特定征象,南京医科大学附属苏州医院超声中心邓学东教授将其命名为“卜”字征。查阅文献,国内外目前对3VT切面呈“卜”字征的疾病的鉴别诊断鲜有报道。笔者通过总结3VT切面上出现“卜”字征的心脏畸形类别,提出相关畸形的鉴别诊断流程图和鉴别要点,旨在提高超声医师在临床实践中对相关疾病的产前检出和诊断能力。
1 资料和方法 1.1 研究对象连续性入选2020年8月至2023年10月于南京医科大学附属苏州医院行心脏超声检查的胎儿。纳入标准:(1)孕龄为20~41周(孕龄根据母体末次月经日期计算;若末次月经不准确,根据超声测量的双顶径、头围、腹围及股骨长计算孕龄);(2)胎儿心脏超声各切面图像清晰可读。排除因母体腹壁较厚、胎动频繁等因素导致胎儿心脏超声图像模糊者。本研究通过南京医科大学附属苏州医院伦理委员会审批(IEC-C-008-A07-V1.0),检查前充分告知家属并签署知情同意书。
1.2 研究方法超声检查采用WS80A(韩国三星公司)和E10(美国GE公司)彩色超声诊断仪,配置探头分别为C1-5-D和CA1-7A。孕妇取仰卧位(检查过程中若有需要,孕妇可取侧卧位),于静息状态下进行检查。检查过程如下:(1)测量和记录胎儿双顶径、头围、腹围和股骨长(单位:mm);(2)按照ISUOG推荐的胎儿心脏连续横向扫查法[1]初步筛查胎儿心脏畸形;(3)选取3VT切面图像进行分析;(4)对3VT切面呈“卜”字征的胎儿详细检查心脏及大血管,并储存超声图像。
超声图像判读由2位具有至少20年胎儿心脏超声诊断经验的主任医师独立判读。若两者判读结果一致,该结果即为最终诊断;若两者判读结果不一致,由第3位同等资历医师核定。
1.3 统计学处理采用SPSS 25软件进行数据分析。计数资料以例数和百分数表示,计量资料以x±s表示。
2 结果 2.1 胎儿一般资料纳入胎儿共计27 019例,母体年龄为19.00~46.00(26.16±3.81)岁,胎儿周龄为20.14~40.42(24.11±2.97)周。3VT切面呈“卜”字征的胎儿有37例,发生率为0.14%;阳性病例的具体资料如表 1所示。37例3VT切面呈“卜”字征的胎儿中,13例(35.14%)为完全性大动脉转位(complete transposition of great arteries,TGA),11例(29.73%)为大动脉关系异常的右心室双出口(double outlet of right ventricle with abnormal relationship of great arteries,DORV/AA),7例(18.92%)为共同动脉干(truncus arteriosus,TA;van Praagh A1、A2和A3型),6例(16.22%)为室间隔缺损型肺动脉闭锁(pulmonary atresia with ventricular septal defect,PA/VSD)。
|
|
表 1 3VT切面呈“卜”字征胎儿的一般资料 |
2.2 鉴别诊断 2.2.1 鉴别诊断流程
上述4种疾病的鉴别诊断可从是否存在主动脉和肺动脉、心室-大动脉连接关系及双肺的血供来源3个方面层层分析,从而逐步推导出诊断结果。具体如图 1所示。
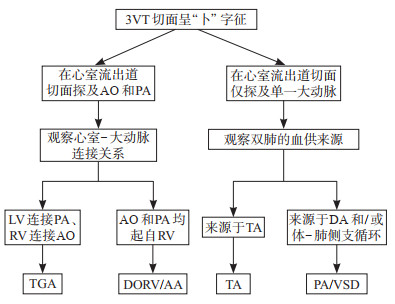
|
图 1 胎儿3VT切面呈“卜”字征病因的鉴别诊断流程图 3VT:三血管气管;TGA:完全性大动脉转位;DORV/AA:大动脉关系异常的右心室双出口;TA:共同动脉干;PA/VSD:室间隔缺损型肺动脉闭锁;AO:主动脉;PA:肺动脉;LV:左心室;RV:右心室;DA:动脉导管. |
2.2.2 鉴别诊断所需的主要超声切面
鉴别“卜”字征病因所需的超声切面主要包括左心室流出道切面和右心室流出道切面,另外探寻肺动脉起源所需的超声切面还有上纵隔横切面和主动脉弓长轴切面。见表 2。
|
|
表 2 胎儿3VT切面“卜”字征病因的超声鉴别诊断 |
2.2.3 鉴别诊断要点
如表 2所示,TGA的鉴别要点是心室-大动脉连接不一致即左心室连接肺动脉,右心室连接主动脉,两者平行走行,伴或不伴室间隔缺损(图 2A1~2A3)。DORV/AA的鉴别要点是主动脉和肺动脉全部或大部分起自右心室,两者平行走行,室间隔位于肺动脉瓣下或远离大动脉,伴或不伴肺动脉狭窄(图 2B1~2B3)。TA的鉴别要点是仅探及一组房室瓣和单一大动脉,单一大动脉骑跨于室间隔上,肺动脉主干或分支起自单一大动脉(图 2C1~2C3)。PA/VSD的鉴别要点是仅探及主动脉,主动脉骑跨于室间隔上,肺动脉闭锁(瓣膜、主干或分支闭锁),双侧肺组织的血供来源于动脉导管逆向灌注和/或体-肺侧支循环(图 2D1~2D3)。
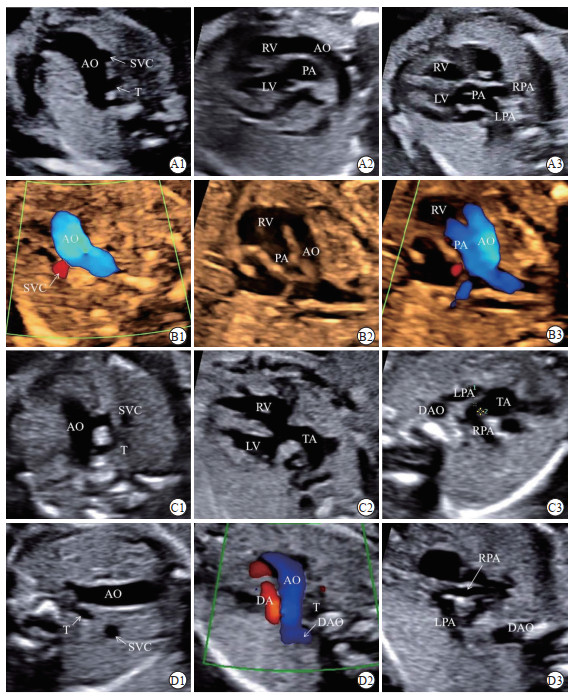
|
图 2 胎儿3VT切面呈“卜”字征的心脏疾病的超声图像 A1~A3:完全性大动脉转位的超声图像.A1:3VT切面呈“卜”字征;A2:右心室(RV)流出道切面显示主动脉(AO)起源于RV;A3:左心室(LV)流出道切面显示肺动脉(PA)起源于LV.B1~B3:大动脉关系异常的左心室双出口的超声图像.B1:3VT切面呈“卜”字征;B2:RV流出道切面显示AO和PA均起源于RV;B3:RV流出道切面彩色多普勒显像证实AO和PA均起源于RV.C1~C3:共同动脉干(TA)的超声图像.C1:3VT切面呈“卜”字征;C2:心室流出道切面显示单一大动脉骑跨于室间隔上;C3:上纵隔横切面显示左肺动脉(LPA)和右肺动脉(RPA)均起源于单一大动脉.D1~D3:室间隔缺损型肺动脉闭锁的超声图像.D1:3VT切面呈“卜”字征;D2:AO弓横切面显示DA的血流呈逆向灌注(红色);D3:上纵隔横切面显示依赖于DA逆向灌注的LPA和RPA.3VT:三血管气管;SVC:上腔静脉;T:气管;DAO:降主动脉;DA:动脉导管. |
3 讨论
超声3VT切面的可疑异常征象对产前超声筛查心脏畸形具有重要的警示作用。本研究以临床实践为导向,在既往研究基础之上,总结了超声3VT切面呈“卜”字征需要鉴别诊断的疾病,主要包括TGA、DORV/AA、TA(van Praagh A1、A2和A3型)和PA/VSD,并绘制了超声鉴别诊断流程图,剖析了“卜”字征病因鉴别诊断所需的主要超声切面和鉴别要点,对提高上述畸形的产前检出率、加深对相关畸形解剖关系的理解具有重要意义。
TGA病例中肺动脉起自左心室,主动脉起自右心室。一方面,肺动脉下方的动脉圆锥被吸收(肺动脉与二尖瓣之间呈纤维连接),肺动脉下方缺少动脉圆锥支撑,导致与肺动脉延续的DAA位置相对正常降低。另一方面,主动脉下方的动脉圆锥被保留下来(主动脉与三尖瓣之间呈肌性连接),主动脉下方存在动脉圆锥支撑,导致与升主动脉延续的主动脉弓位置相对正常升高[7-8]。上述2个解剖因素导致TGA胎儿无法像正常胎儿那样在3VT切面同时显示DAA和主动脉弓,而仅能显示位置更高的主动脉弓,后者与上腔静脉的短轴一起构成“卜”字征。
DORV/AA病例中,按照阜外医院逄坤静和李守军[9]提出的先天性右心室双出口新解剖分型超声心动图诊断规范专家共识,大动脉关系异常指大动脉转位,主动脉和肺动脉平行排列[10-11]。这种情况下,主动脉和肺动脉均起自右心室,且绝大多数情况下两者下方均存在动脉圆锥[12],主动脉被动脉圆锥推挤上移,从而使主动脉弓位置较正常更高。因此,3VT切面能探及主动脉弓和上腔静脉短轴形成的“卜”字征。
TA病例仅存在单一的动脉干,单一动脉干发出主动脉和肺动脉主干或分支。从van Praagh提出的TA分型方法中不难看出,绝大多数情况下van Praagh A1、A2和A3型DAA缺如[13],3VT切面上仅显示由单一的动脉干横弓和上腔静脉短轴形成“卜”字征。而A4型中虽然存在动脉导管,但合并了主动脉弓离断,3VT切面难以形成“V”字征或“卜”字征。
与TGA的单一动脉干相似,PA/VSD病例中仅存在主动脉,肺动脉在瓣膜、主干或分支水平发生闭锁,双侧肺组织的血供来源于动脉导管和/或体-肺侧支循环。从国际公认的Tchervenkov分型不难发现,与正常DAA相比,Tchervenkov A和B型中动脉导管常常走行迂曲,内径较细[14],难以与主动脉横弓构成正常的“V”字征。而Tchervenkov C型动脉导管完全缺如,肺组织血供完全依赖体-肺侧支循环[15]。因此,Tchervenkov A、B和C型PA/VSD在3VT切面上也显示为由主动脉横弓和上腔静脉短轴构成的“卜”字征。
本研究提出了3VT切面“卜”字征的产前超声鉴别诊断流程图,对后期的临床实践具有一定的指导意义。但是,本研究也存在不足之处,先天性心脏病纷繁复杂,本研究样本量较小,3VT切面呈“卜”字征的潜在疾病未被完全纳入,有待后续更大样本量的研究进一步探索。
综上所述,胎儿心脏超声3VT切面呈“卜”字征的鉴别诊断内容包括TGA、DORV/AA、TA(van Praagh A1、A2和A3型)和PA/VSD,超声医师掌握鉴别各疾病的超声诊断思路和方法有助于提高相关畸形的产前检出率和诊断能力。
| [1] |
International Society of Ultrasound in Obstetrics and Gynecology, CARVALHO J S, ALLAN L D, et al. ISUOG practice guidelines (updated): sonographic screening examination of the fetal heart[J]. Ultrasound Obstet Gynecol, 2013, 41(3): 348-359. DOI:10.1002/uog.12403 |
| [2] |
MORI M, ISHII Y, TAKAHASHI K, et al. Utility of the angle between the right aortic arch and first branch for detecting double aortic arch via fetal echocardiography[J]. Fetal Diagn Ther, 2024, 51(1): 16-22. DOI:10.1159/000534039 |
| [3] |
CAMPANALE C M, PASQUINI L, SANTANGELO T P, et al. Prenatal echocardiographic assessment of right aortic arch[J]. Ultrasound Obstet Gynecol, 2019, 54(1): 96-102. DOI:10.1002/uog.20098 |
| [4] |
YERLIKAYA G, EFETÜRK T, SPRINGER S, et al. Prenatal detection of right aortic arch[J]. Arch Gynecol Obstet, 2019, 299(4): 933-938. DOI:10.1007/s00404-019-05056-5 |
| [5] |
YAN Y, YANG Z, LI Y, et al. The prenatal diagnosis and prognosis of fetal right aortic arch and double aortic arch malformation: a single-center study[J]. J Obstet Gynaecol Res, 2023, 49(9): 2273-2282. DOI:10.1111/jog.15712 |
| [6] |
GUO Q, KONG Y, ZENG S, et al. Fetal double aortic arch: prenatal sonographic and postnatal computed tomography angiography features, associated abnormalities and clinical outcomes[J]. BMC Pregnancy Childbirth, 2020, 20(1): 614. DOI:10.1186/s12884-020-03300-4 |
| [7] |
GIREADǍ R, SOCOLOV D, MIHǍLCEANU E, et al. The additional role of the 3-vessels and trachea view in screening for congenital heart disease[J]. Medicina (Kaunas), 2022, 58(2): 262. DOI:10.3390/medicina58020262 |
| [8] |
LACHAUD M, DIONNE A, BRASSARD M, et al. Cardiac hemodynamics in fetuses with transposition of the great arteries and intact ventricular septum from diagnosis to end of pregnancy: longitudinal follow-up[J]. Ultrasound Obstet Gynecol, 2021, 57(2): 273-281. DOI:10.1002/uog.21920 |
| [9] |
逄坤静, 李守军. 先天性右室双出口新解剖分型超声心动图诊断规范专家共识[J]. 中国超声医学杂志, 2022, 38(7): 721-729. DOI:10.3969/j.issn.1002-0101.2022.07.001 |
| [10] |
GOTTSCHALK I, ABEL J S, MENZEL T, et al. Prenatal diagnosis, associated findings and postnatal outcome of fetuses with double outlet right ventricle (DORV) in a single center[J]. J Perinat Med, 2019, 47(3): 354-364. DOI:10.1515/jpm-2018-0316 |
| [11] |
KARMEGARAJ B, KUMAR S, SRIMURUGAN B, et al. 3D/4D spatiotemporal image correlation (STIC) fetal echocardiography provides incremental benefit over 2D fetal echocardiography in predicting postnatal surgical approach in double-outlet right ventricle[J]. Ultrasound Obstet Gynecol, 2021, 57(3): 423-430. DOI:10.1002/uog.21988 |
| [12] |
MA M, LI Y, CHEN R, et al. Diagnostic performance of fetal intelligent navigation echocardiography (FINE) in fetuses with double-outlet right ventricle (DORV)[J]. Int J Cardiovasc Imag, 2020, 36(11): 2165-2172. DOI:10.1007/s10554-020-01932-3 |
| [13] |
ABEL J S, BERG C, GEIPEL A, et al. Prenatal diagnosis, associated findings and postnatal outcome of fetuses with truncus arteriosus communis (TAC)[J]. Arch Gynecol Obstet, 2021, 304(6): 1455-1466. DOI:10.1007/s00404-021-06067-x |
| [14] |
GOTTSCHALK I, STRIZEK B, JEHLE C, et al. Prenatal diagnosis and postnatal outcome of fetuses with pulmonary atresia and ventricular septal defect[J]. Ultraschall Med, 2020, 41(5): 514-525. DOI:10.1055/a-0770-2832 |
| [15] |
GINDES L, SALEM Y, GASNIER R, et al. Prenatal diagnosis of major aortopulmonary collateral arteries (MAPCA) in fetuses with pulmonary atresia with ventricular septal defect and agenesis of ductus arteriosus[J]. J Matern Fetal Neonatal Med, 2022, 35(25): 5400-5408. DOI:10.1080/14767058.2021.1881475 |
 2024, Vol. 45
2024, Vol. 45


