青少年特发性脊柱侧凸(adolescent idiopathic scoliosis,AIS)是一种脊柱三维畸形[1]。Lenke 2A型AIS包括结构性的主胸弯和上胸弯[2-4],对于度数较大的Lenke 2A型侧弯,通常采用后路胸椎融合术进行矫治,其目的是在矫正畸形的同时尽可能保留腰椎活动节段[5-6]。然而,这种方法存在远端叠加现象(distal adding-on)等并发症风险。远端叠加的特征是远端固定椎(lowest instrumented vertebra,LIV)逐渐偏移中线或LIV下位椎间盘成角逐渐增大,包括远端融合椎下位椎间盘成角增加>5°、LIV下位椎体偏移骶骨中垂线(central sacral vertical line,CSVL)的距离增加>5 mm。远端叠加可能加速LIV下方椎间盘的退变,引起外观畸形加重、疼痛不适等,降低患者满意度[7-9]。因此,如何降低术后叠加发生率一直是学者研究的热点。
在以往的研究中,关于Lenke 2A型AIS中远端叠加危险因素的研究集中在LIV的选择上,LIV位置过高(LIV位于远端充分触及椎体近端)、LIV旋转或偏移中线过大等诸多因素都会增加术后远端叠加的风险[10-12]。上端固定椎(upper instrumented vertebra,UIV)的选择在Lenke 2A型AIS中一直是研究的热点,其选择存在一定的争议,一般认为对于右胸弯患者,如果术前左肩较高,则应融合上胸弯;而对于术前左肩低的患者,上胸弯是否融合存在不确定性[13-14]。既往关于UIV的选择主要集中在其与肩平衡的关系上[15-16],而Cao等[17]和Qin等[18]研究发现肩平衡与远端叠加存在一定的相互代偿关系。因此,本研究针对术前左肩低的Lenke 2A型患者,分析上胸弯的融合是否会增加远端叠加的发生风险。
1 资料和方法 1.1 病例资料回顾性选择2010年7月16日至2018年10月21日在我院行脊柱后路胸腰椎融合手术且仅使用椎弓根螺钉内固定的AIS患者为研究对象。纳入标准:Lenke 2A型右胸弯;年龄为11~18岁;术前左肩低于右肩;术后随访2年以上;有完整的临床和影像学资料。排除标准:神经性肌源性及先天性脊柱侧凸;神经系统查体异常;有其他脊柱手术史。LIV的选择由经验丰富的脊柱外科医师根据远端充分触及椎(last substantially touched vertebra,LSTV)原则[19-20]确定。UIV的选择同样由经验丰富的脊柱外科医师根据术前双肩平衡等的相关策略决定。根据UIV的选择,将患者分为≥T3组(UIV在T3及T3以上)和<T3组(UIV在T3以下)。记录患者年龄、性别及Risser分级等临床信息。
1.2 影像学数据测量收集术前、术后及末次随访时患者直立后前位和侧位X线片测量结果,并评估术前左右弯曲位(bending位)X线片数据。测量的影像学参数包括上胸弯、主胸弯和腰弯的Cobb角,主胸弯的顶椎偏移,LIV相对于CSVL的位置,融合节段下方第1个椎间盘的倾斜程度,冠状面和矢状面平衡,躯干移位,以及锁骨角、T1倾斜角和X线片肩部高度(radiographical shoulder height,RSH)。术后肩部不平衡(postoperative shoulder imbalance,PSI)定义为术后左肩抬高2 cm[21]。冠状面C7铅垂线与CSVL的偏差用于测量冠状面平衡,其值>20 mm表示冠状面失衡。C7铅垂线偏离骶骨后缘(也称为矢状面垂直轴,sagittal vertical axis,SVA)用于测量矢状面平衡,其值>50 mm表示矢状面失衡[22]。在躯干垂直参考线和CSVL之间测量躯干移位[21]。侧弯柔韧性(%)=(术前站立位Cobb角-术前弯曲位Cobb角)/术前站立位Cobb角×100%[21]。矫正率(%)=(术前Cobb角-术后Cobb角)/术前Cobb角×100%[22]。当融合节段下方第1个椎体与CSVL之间的距离增加>5 mm或融合节段下方第1个椎间盘的角度增加>5°时,被认为是发生了远端叠加[23]。
所有测量均由两人使用Surgimap 2.1.2软件共同完成。此外,随机选择20例患者用于评估测量值的观察者内和观察者间变异性。所有参数具有较强的观察者内和观察者间一致性,Kappa系数均在0.8以上。
1.3 生活质量评估在末次随访时,患者填写脊柱侧凸研究协会22项(scoliosis research society-22,SRS-22)问卷[24]。该问卷涵盖功能/活动、疼痛、自我感知形象、治疗满意度和心理健康5个维度。每个维度包含5个问题选项,分值为1~5,5分代表理想的回答。5个维度得分的平均值为问卷结果。
1.4 统计学处理采用SPSS 20.0软件对数据进行分析。计量资料以x ± s表示,采用方差分析、t检验进行比较。计数资料以例数和百分数表示,采用χ2检验进行比较。通过逐步logistic回归分析考察远端叠加的影响因素。检验水准(α)为0.05。
2 结果 2.1 患者手术前后影像学资料共104例术前左肩低的Lenke 2A型AIS患者纳入研究,其中女73例、男31例,手术时年龄为(14.8±3.2)岁,随访时间为24~74(33.0±9.6)个月,Risser分级为3.3±1.5。患者影像学资料见表 1。术前上胸弯、主胸弯和腰弯的平均Cobb角分别为(41.0±9.0)°、(55.6±11.8)°和(25.7±7.6)°,侧弯柔韧性分别为(22.9±14.0)%、(42.9±17.3)%和(71.3±36.2)%。末次随访时,上胸弯、主胸弯和腰弯的平均Cobb角分别为(22.5±7.5)°、(20.4±7.7)°、(9.2±5.1)°,矫正率分别为(42.5±20.6)%、(62.8±13.4)%和(62.1±21.5)%。冠状面失衡5例,矢状面失衡6例。末次随访时,27例(26.0%)患者出现远端叠加,无患者因叠加现象进行翻修手术。
|
|
表 1 伴左肩低Lenke 2A型AIS患者手术前后的影像学资料 Tab 1 Preoperative and postoperative radiographical data of Lenke type 2A AIS patients with low left shoulder |
2.2 UIV选择≥T3组与<T3组患者临床及影像学参数比较
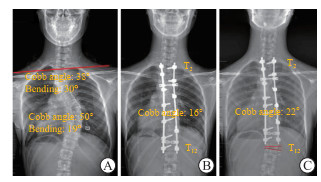
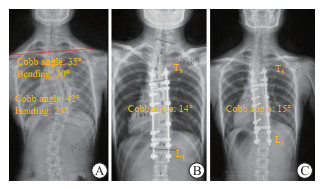
根据UIV的选择,≥T3组患者71例(图 1,表 2),<T3组患者33例(图 2,表 2)。两组患者术前临床及影像学参数匹配(均P>0.05)。LIV的选择采用LSTV原则,且在两组间差异无统计学意义(P>0.05)。两组患者术后即刻的RSH、躯干平衡及上胸弯、主胸弯残留角度差异均无统计学意义(均P>0.05)。末次随访时,≥T3组的远端叠加发生率高于<T3组(P<0.001);两组在锁骨角、RSH和躯干移位等方面差异均无统计学意义(均P>0.05);15例(14.4%)患者发生PSI,其中<T3组4例(12.1%),≥T3组11例(15.5%),差异无统计学意义(P>0.05)。
|
图 1 UIV高于T3患者的影像学资料 Fig 1 Radiographical data of patients with UIV above T3 A 16-year-old girl with Lenke type 2A AIS. A: Preoperative X-ray showed low left shoulder (RSH was 11.7 mm, red line); B: Immediately postoperative, UIV was T2; C: After 2 years of follow-up, the shoulder balance was improved, and X-ray showed adding-on (red lines). UIV: Upper instrumented vertebra; AIS: Adolescent idiopathic scoliosis; RSH: Radiographical shoulder height. |
|
|
表 2 UIV选择≥T3组和<T3组伴左肩低Lenke 2A型AIS患者的临床和影像学资料 Tab 2 Clinical and radiographical data of Lenke type 2A AIS patients with low left shoulder in UIV≥T3 and < T3 groups |
|
图 2 UIV低于T3患者的影像学资料 Fig 2 Radiographical data of patients with UIV below T3 A 17-year-old girl with Lenke type 2A AIS. A: Preoperative X-ray showed low left shoulder (RSH was 12.3 mm, red line); B: Immediately postoperative, UIV was T5; C: After 2 years of follow-up, X-ray showed no adding-on. UIV: Upper instrumented vertebra; AIS: Adolescent idiopathic scoliosis; RSH: Radiographical shoulder height. |
2.3 UIV选择≥T3组与<T3组患者生活质量比较
末次随访时,两组患者SRS-22问卷各维度评分差异均无统计学意义(均P>0.05)。见表 3。
|
|
表 3 UIV选择≥T3组和<T3组伴左肩低Lenke 2A型AIS患者的SRS-22问卷评分比较 Tab 3 Comparison of SRS-22 questionnaire scores between UIV≥T3 group and < T3 group of patients with Lenke type 2A AIS and low left shoulder |
2.4 远端叠加的影响因素分析
多因素二项logistic回归分析显示,Risser分级和UIV选择是伴左肩低Lenke 2A型AIS患者术后发生远端叠加的独立影响因素。见表 4。
|
|
表 4 伴左肩低Lenke 2A型AIS患者术后远端叠加影响因素的logistic回归分析 Tab 4 Logistic regression analysis of influencing factors of distal adding-on in Lenke type 2A AIS patients with low left shoulder |
3 讨论
Lenke分型最早由Lenke等[4]于2001年提出,该分类考虑了脊柱侧凸的位置、柔韧性和弯曲严重程度,用于指导治疗和比较不同治疗方法的优劣[2]。经过多年的发展,Lenke分型已成为国际公认的指导手术方案和预后的重要标准。虽然它的分类系统有助于指导不同分型的手术方案,但它并没有明确定义融合的具体节段。减少融合节段可以降低手术成本、提高患者术后生活质量。
关于Lenke 2A型AIS患者远端叠加的研究倾向关注LIV的选择[8, 11-12]。而针对于UIV的选择研究较少。Suk等[6]认为当上胸弯Cobb角>25°、左肩高于右肩超过10 mm的患者上胸弯应该融合。而当上胸弯Cobb角为25°~40°时,若右肩高于左肩,特别是当双肩高度差>12 mm时上胸弯不需要融合[25]。Jiang等[13]认为,除了根据Lenke分型考虑术前双肩高度差外,在选择UIV时还应综合考虑上胸弯的柔韧性、主胸弯的大小等因素,对于术前上胸弯柔韧性好、右肩高的患者,UIV可选择T4或T5;对于上胸弯僵直且术前左肩高或肩平的患者,UIV应为T1或T2;对于上胸弯僵直且术前右肩较高的患者,上胸弯也可以部分融合或不融合,无需过度矫正。Kuklo等[15]也报道,如果患者术前肩部平衡,上胸弯是否融合对术后肩部平衡影响不大;如果术前右肩高,左肩可以自发抬起以补偿主胸弯的矫正,即使上胸弯的柔韧性较差也不需要完全融合;对于术前左肩高的患者,即使上胸弯柔韧性良好也需要进行上胸弯曲融合。Menon等[16]根据肩部平衡的决定性因素选择了UIV,如果肩部水平取决于上胸弯(双侧喙突线向上胸凹侧倾斜,相当于左肩抬高),无论上胸弯的大小和柔韧性如何,都建议选择T2为UIV;相反,如果肩关节水平取决于胸主弯(双侧喙突线向胸主弯侧倾斜,相当于右肩抬高),则建议选择T4为UIV,但应注意避免过度矫正主胸弯[26]。这些研究结果反映了目前UIV选择的基本状况。尽管在AIS患者的双肩平衡中高度重视UIV的选择,但目前尚缺乏对上胸弯UIV的选择和术后远端叠加风险的相关性研究。
在本研究中,26.0%(27/104)的患者在末次随访时观察到远端叠加现象。以往研究报道,叠加的发生率为12.9%~51.1%[4, 6, 12-13, 27-29]。本研究结果与以往报道一致。本研究将Lenke 2A型AIS患者根据不同的UIV选择分为≥T3和<T3两组,分析结果表明≥T3组的叠加风险增加。Cao等[17]在142例患者的研究中发现,在末次随访时发生远端叠加的患者较少能观察到肩部失平衡,术后远端叠加很可能与PSI之间存在相关性。Zhao等[29]在Lenke 1A/B型AIS患者中研究对称胸椎融合时发现,与对称融合组(在顶椎上下有相同数量的椎体融合)和下优势融合组(顶端以下融合的椎体比顶椎以上融合的椎体数多)相比,上优势融合组(顶端以上融合的椎体比顶椎以下融合的椎体数多)远端叠加的发生率显著增加,这很有可能是因为上胸弯的过度固定会降低通过双肩平衡进行代偿的能力。本研究通过对≥T3和<T3两组患者术后即刻的RSH及主胸弯残留角度进行对比,发现并无显著差异,说明本研究排除手术本身造成的远端叠加危险因素对结果的干扰。因而,我们认为对术前左肩低的Lenke 2A型AIS患者进行过度上胸弯固定可能会增加远端叠加的发生风险。
本研究存在以下局限性,首先,为回顾性研究设计及缺乏随机化分组;其次,结果可能会因相对较少的远端叠加患者而存在偏差。因此,需要开展更大样本量的研究以进一步得出更加可靠的结论。
综上所述,对于术前左肩低的Lenke 2A型AIS患者,UIV的选择是影响术后远端叠加的重要因素。对于此类患者,融合上胸弯将导致远端叠加的发生率增加。建议在伴左肩低的Lenke 2A型AIS患者中谨慎考虑将融合水平延长至T3及以上,以规避因失去肩部平衡的代偿能力而可能导致的远端叠加风险增加。
| [1] |
GARDNER-MORSE M, STOKES I A. Three-dimensional simulations of the scoliosis derotation maneuver with Cotrel-Dubousset instrumentation[J]. J Biomech, 1994, 27(2): 177-181. DOI:10.1016/0021-9290(94)90206-2 |
| [2] |
LENKE L G. The Lenke classification system of operative adolescent idiopathic scoliosis[J]. Neurosurg Clin N Am, 2007, 18(2): 199-206. DOI:10.1016/j.nec.2007.02.006 |
| [3] |
LEHMAN R A Jr, LENKE L G, KEELER K A, et al. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases[J]. Spine (Phila Pa 1976), 2008, 33(14): 1598-1604. DOI:10.1097/BRS.0b013e318178872a |
| [4] |
LENKE L G, BETZ R R, HARMS J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis[J]. J Bone Joint Surg Am, 2001, 83(8): 1169-1181. |
| [5] |
DOBBS M B, LENKE L G, KIM Y J, et al. Selective posterior thoracic fusions for adolescent idiopathic scoliosis: comparison of hooks versus pedicle screws[J]. Spine (Phila Pa 1976), 2006, 31(20): 2400-2404. DOI:10.1097/01.brs.0000240212.31241.8e |
| [6] |
SUK S I, LEE S M, CHUNG E R, et al. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up[J]. Spine (Phila Pa 1976), 2005, 30(14): 1602-1609. DOI:10.1097/01.brs.0000169452.50705.61 |
| [7] |
WANG Y, HANSEN E S, HØY K, et al. Distal adding-on phenomenon in Lenke 1A scoliosis: risk factor identification and treatment strategy comparison[J]. Spine (Phila Pa 1976), 2011, 36(14): 1113-1122. DOI:10.1097/BRS.0b013e3181f51e95 |
| [8] |
YANG C, LI Y, YANG M, et al. Adding-on phenomenon after surgery in Lenke type 1, 2 adolescent idiopathic scoliosis: is it predictable?[J]. Spine (Phila Pa 1976), 2016, 41(8): 698-704. DOI:10.1097/BRS.0000000000001303 |
| [9] |
SPONSELLER P D, BETZ R, NEWTON P O, et al. Differences in curve behavior after fusion in adolescent idiopathic scoliosis patients with open triradiate cartilages[J]. Spine (Phila Pa 1976), 2009, 34(8): 827-831. DOI:10.1097/BRS.0b013e31819139ef |
| [10] |
QIN X, QIU Y, HE Z, et al. Can we stop distally at LSTV-1 for adolescent idiopathic scoliosis with Lenke 1A/2A curves?[J]. Spine (Phila Pa 1976), 2021, 47(8): 624-631. DOI:10.1097/brs.0000000000004206 |
| [11] |
HE Z, QIN X, YIN R, et al. The rotation of preoperative-presumed lowest instrumented vertebra: is it a risk factor for distal adding-on in Lenke 1A/2A curve treated with selective thoracic fusion?[J]. Eur Spine J, 2020, 29(8): 2054-2063. DOI:10.1007/s00586-020-06353-3 |
| [12] |
QIN X, HE Z, YIN R, et al. Selecting the last substantially touching vertebra as lowest instrumented vertebra in Lenke type 2A-R and 2A-L curves[J]. Spine (Phila Pa 1976), 2020, 45(5): 309-318. DOI:10.1097/brs.0000000000003254 |
| [13] |
JIANG J, QIAN B P, QIU Y, et al. Full fusion of proximal thoracic curve helps to prevent postoperative cervical tilt in Lenke type 2 adolescent idiopathic scoliosis patients with right-elevated shoulder[J]. BMC Musculoskelet Disord, 2017, 18(1): 362. DOI:10.1186/s12891-017-1730-y |
| [14] |
CHANG D G, KIM J H, KIM S S, et al. How to improve shoulder balance in the surgical correction of double thoracic adolescent idiopathic scoliosis[J]. Spine (Phila Pa 1976), 2014, 39(23): E1359-E1367. DOI:10.1097/BRS.0000000000000578 |
| [15] |
KUKLO T R, LENKE L G, GRAHAM E J, et al. Correlation of radiographic, clinical, and patient assessment of shoulder balance following fusion versus nonfusion of the proximal thoracic curve in adolescent idiopathic scoliosis[J]. Spine (Phila Pa 1976), 2002, 27(18): 2013-2020. DOI:10.1097/00007632-200209150-00009 |
| [16] |
MENON K V, TAHASILDAR N S. What constitutes shoulder imbalance in adolescent idiopathic scoliosis?aesthetic threshold for surgical correction[J]. World Neurosurg, 2020, 138: e827-e838. DOI:10.1016/j.wneu.2020.03.106 |
| [17] |
CAO K, WATANABE K, HOSOGANE N, et al. Association of postoperative shoulder balance with adding-on in Lenke type Ⅱ adolescent idiopathic scoliosis[J]. Spine (Phila Pa 1976), 2014, 39(12): E705-E712. DOI:10.1097/BRS.0000000000000325 |
| [18] |
QIN X, XIA C, XU L, et al. Natural history of postoperative adding-on in adolescent idiopathic scoliosis: what are the risk factors for progressive adding-on?[J]. BioMed Res Int, 2018, 2018: 3247010. DOI:10.1155/2018/3247010 |
| [19] |
MURPHY J S, UPASANI V V, YASZAY B, et al. Predictors of distal adding-on in thoracic major curves with AR lumbar modifiers[J]. Spine (Phila Pa 1976), 2017, 42(4): E211-E218. DOI:10.1097/BRS.0000000000001761 |
| [20] |
QIN X, SUN W, XU L, et al. Selecting the last "substantially" touching vertebra as lowest instrumented vertebra in Lenke type 1A curve[J]. Spine (Phila Pa 1976), 2016, 41(12): E742-E750. DOI:10.1097/brs.0000000000001374 |
| [21] |
OHRT-NISSEN S, KAMATH V H D, SAMARTZIS D, et al. Fulcrum flexibility of the main curve predicts postoperative shoulder imbalance in selective thoracic fusion of adolescent idiopathic scoliosis[J]. Eur Spine J, 2018, 27(9): 2251-2261. DOI:10.1007/s00586-018-5669-y |
| [22] |
SMITH M W, ANNIS P, LAWRENCE B D, et al. Acute proximal junctional failure in patients with preoperative sagittal imbalance[J]. Spine J, 2015, 15(10): 2142-2148. DOI:10.1016/j.spinee.2015.05.028 |
| [23] |
WANG Y, BÜNGER C E, WU C, et al. Postoperative trunk shift in Lenke 1C scoliosis: what causes it?How can it be prevented?[J]. Spine (Phila Pa 1976), 2012, 37(19): 1676-1682. DOI:10.1097/BRS.0b013e318255a053 |
| [24] |
MONTICONE M, NAVA C, LEGGERO V, et al. Measurement properties of translated versions of the Scoliosis Research Society-22 Patient Questionnaire, SRS-22:a systematic review[J]. Qual Life Res, 2015, 24(8): 1981-1998. DOI:10.1007/s11136-015-0935-5 |
| [25] |
SUN X, LIU W J, XU L L, et al. Does brace treatment impact upon the flexibility and the correctability of idiopathic scoliosis in adolescents?[J]. Eur Spine J, 2013, 22(2): 268-273. DOI:10.1007/s00586-012-2477-7 |
| [26] |
MITCHELL B C, SKAGGS D L, LENKE L G, et al. Defining risk factors for adding-on in Lenke 1 and 2 AR curves[J]. Spine Deform, 2021, 9(6): 1569-1579. DOI:10.1007/s43390-021-00382-8 |
| [27] |
MUNAKATA R, KOSEKI M, OBA H, et al. Selecting the C7-LIV line vertebra as the upper instrumented vertebra for adolescent idiopathic scoliosis Lenke type 1A curves: multicenter and a minimum 2-year follow-up study[J]. Spine (Phila Pa 1976), 2020, 45(17): 1239-1245. DOI:10.1097/BRS.0000000000003509 |
| [28] |
EL RACHKIDI R, SILVESTRE C, ROUSSOULY P. Early revision surgery for distal adding-on correction in Lenke 1 and 2 adolescent idiopathic scoliosis[J]. Cureus, 2022, 14(11): e30960. DOI:10.7759/cureus.30960 |
| [29] |
ZHAO Z, LIU Z, HU Z, et al. Does symmetric thoracic fusion make a difference in Lenke 1 A/B AIS patients?[J]. Spine (Phila Pa 1976), 2019, 44(3): E168-E174. DOI:10.1097/BRS.0000000000002940 |
 2024, Vol. 45
2024, Vol. 45


