2. 海军军医大学(第二军医大学)第二附属医院门诊部, 上海 200003
2. Outpatient Department, The Second Affiliated Hospital of Naval Medical University (Second Military Medical University), Shanghai 200003, China
青少年特发性脊柱侧凸(adolescent idiopathic scoliosis,AIS)是指10~18岁青少年不明原因发生的Cobb角≥10 °的脊柱畸形,患病率为0.5%~5.2%,女性多见,是最常见的脊柱侧凸类型[1, 2]。脊柱畸形进行性加重可以导致外观畸形、腰背部疼痛甚至心肺功能障碍,对青少年的身体和心理健康造成严重危害。由于2/3的AIS患者在青春期会出现脊柱侧凸进展[3],因此,尽早发现并及时干预是治疗AIS的关键。对于Cobb角≥40°的脊柱侧凸患者,即使进入成年期并且骨骼发育成熟,脊柱畸形仍可能继续加重[4],此类患者通常需进行手术治疗。
手术治疗的主要目标是矫正脊柱畸形,防止侧弯继续进展,进而达到冠状面、矢状面平衡及固定节段稳定融合的效果。AIS的手术方式包括前路、后路及前后联合入路,其中后路脊柱融合术(posterior spinal fusion,PSF)是目前治疗AIS应用最广泛的手术方式[5]。虽然手术治疗使大多数AIS患者取得良好预后,但仍存在并发症风险。研究表明,AIS患者接受PSF后总体并发症发生率为1%~22%[6]。Bartley等[7]研究表明,AIS患者接受PSF的围手术期并发症发生率为2.4%,死亡率为0.03%,晚期并发症发生率为4.1%。术后并发症包括感染、内固定失败、畸形进展、神经功能损伤、脑脊液漏等。其中,畸形进展相关并发症是最常见、脊柱外科医师最关注的并发症类型,主要包括叠加(adding-on)现象、近端交界性后凸(proximal junctional kyphosis,PJK)、远端交界性后凸(distal junctional kyphosis,DJK)、冠状面失衡和术后双肩不平衡(postoperative shoulder imbalance,PSI)。这些并发症常常导致矫形手术失败,部分患者需进行翻修手术,给患者和其家庭造成沉重负担。本文对AIS患者PSF治疗后畸形相关并发症的最新进展进行总结,为今后AIS术后畸形相关并发症的研究和临床诊疗工作提供参考。
1 叠加现象 1.1 定义、诊断标准及发生率叠加现象又称为远端叠加现象,是指脊柱侧凸矫形术后内固定远端畸形进行性加重的现象,同时伴有远端椎体偏移、旋转或远端椎间盘角度增大[8]。其特征包括:(1)远端固定椎(lowest instrumented vertebra,LIV)下位椎间盘成角增加>5°;(2)LIV下位椎体偏离骶骨中垂线(central sacral vertical line,CSVL)的距离增加>5 mm。叠加现象是AIS后路矫形术后的常见并发症,这一现象最早由Suk等[9]报道。据文献报道,AIS患者接受PSF治疗后出现叠加现象的发生率差异较大,为2%~51%[10]。Yang等[11]研究发现,AIS患者叠加现象的总体发病率为14%,其中,Lenke 1A型、Lenke 2型和Lenke 5型AIS患者的发生率分别为15%、12%、9%。
1.2 危险因素分析及预防措施Fujii等[12]对69例接受后路选择性胸椎融合术(selective thoracic fusion,STF)的Lenke 1B、1C型AIS患者进行了研究,2年的随访中有13例患者发生叠加现象,发生率为18.8%。当LIV位于最后触及椎(last touched vertebra,LTV)头端且距离LTV越远时,叠加的风险越高。另外,建议术中常规进行X线透视,如果发现选择的LIV下方椎间盘成角>3°,则LIV应继续向下选择。Banno等[13]回顾性分析了90例接受PSF的Lenke 1A、2A型AIS患者资料,发现当LIV满足以下条件时叠加现象发生率仅为3.3%:(1)牵引位下的稳定椎,(2)侧方弯曲位(bending位)LIV下方椎间盘平衡。Wang等[14]认为LIV下方椎体(LIV+1)偏离CSVL的距离是Lenke 1A型AIS患者术后发生叠加现象的危险因素,当术前LIV+1偏离CSVL>10 mm时,叠加现象的发生率明显增加,因此,建议LIV应选择从骶骨向头端开始第1个偏离CSVL>10 mm的椎体。Joo等[8]认为,对于Lenke 1A型AIS患者,腰弯越大、年龄越小、骶骨倾斜角越大及融合节段越短,发生叠加现象的可能性越大,因此术前应充分评估各项参数,避免危险因素聚集。Matsumoto等[10]发现,对于接受STF的Lenke 1A型患者,当术后残余的主胸弯顶椎偏距较大且LIV位于LTV头端时,更容易发生叠加现象。因此,为了防止术后叠加发生,Matsumoto等[10]建议术中矫形时应尽可能纠正主胸弯的顶椎偏距,并且LIV应至少延伸到LTV。Cho等[15]强调了Lenke 1A型AIS患者区分L4-L型(术前L4椎体向左侧倾斜)和L4-R型(术前L4椎体向右侧倾斜)的重要性,他们研究发现L4-R型患者发生叠加现象的风险更高,而发生叠加现象的L4-L型患者往往年龄更小、骨骼发育不成熟。
Yang等[11]对AIS患者术后发生叠加现象的影响因素进行了文献总结,既往研究中叠加现象的危险因素包括低龄、骨骼发育不成熟、术前上胸弯较小、术前主胸弯较小、术前腰弯较小、术前冠状面与矢状面失衡、LIV选择不当及冠状面和矢状面序列过度矫正。同时,为了防止术后出现叠加现象,Yang等[11]建议:(1)LIV应至少选择下端椎下方1个椎体(EV+1);(2)LIV选择不应超过稳定椎上下2个椎体(SV±2);(3)LIV应选择从骶骨向头端开始第1个偏离CSVL>10 mm的椎体。
2 PJK 2.1 定义、诊断标准及发生率PJK是AIS患者进行后路矫形术后常见的并发症之一,是指脊柱内固定近端交界区后凸畸形逐渐加重的现象,这一概念最早由Lowe等[16]在进行舒尔曼病(Scheuermann disease)后凸畸形研究时提出。随着对脊柱畸形和PJK认识的逐渐深入,PJK的诊断标准在不断改进,目前应用最广泛的诊断标准由Glattes等[17]提出,即术后近端交界区后凸角(proximal junctional angle,PJA)≥10 °,且较术前增加至少10°。PJA是指上端固定椎(upper instrumented vertebra,UIV)下终板与UIV上方第2个椎体上终板之间的夹角。文献报道,AIS患者接受PSF后PJK的发生率为7%~46%[18, 19]。在以胸弯为主的Lenke 1、2型AIS患者中,PSF术后PJK发生率为16%,但患者通常无明显症状,翻修率<3%[20]。对于以腰弯为主的Lenke 5型患者,文献报道术后PJK的发生率为23%[21]。
不同研究中关于PJK自然史的报道较为一致,在一项随访至少5年的研究中,26% 的AIS患者在末次随访时(平均7.3年)发生PJK,其中大多数患者(82%)在术后第2年出现PJK[22]。另一项针对410例AIS患者的研究报道中,PSF术后2年有111例患者发生PJK,发生率为27%;有37例患者在术后8周随访时即表现出PJK,其中4例在术后2年随访时PJK得到缓解[23]。Wang等[24]回顾性分析了接受PSF治疗的123例AIS患者资料,28% 的患者术后发生PJK,术后6个月内发生PJK的患者占31%,6~18个月内发生PJK的患者占46%,18个月及以后发生PJK的患者占23%。
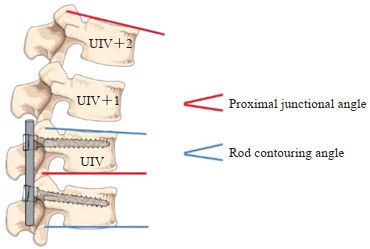
2.2 危险因素分析及预防措施李庆达等[25]针对Lenke 5型AIS患者PSF治疗后发生PJK的研究表明,UIV位于胸腰段、交界区后韧带复合体损伤及术后骨盆入射角与腰椎前凸角差值(pelvic incidence-lumbar lordosis,PI-LL)过高是术后发生PJK的危险因素。因此,建议避免UIV在胸腰段、术中避免损伤交界区后韧带复合体及建立良好的PI-LL值可能会减少PJK的发生。研究表明,术后骨盆入射角较大同时伴有继发性腰椎前凸增大和胸椎后凸增大的AIS患者更容易发生PJK,这可能与矫形术后恢复脊柱矢状面平衡的代偿机制有关;此外,不同材质内固定棒对PJK发生也有一定的影响,使用钴铬棒的患者发生PJK的风险较高,为28%[20]。Erkilinc等[26]研究发现,AIS患者PSF中在UIV水平放置横突钩能显著降低PJK发生的风险,横突钩组PJK发生率为3.2%,螺钉组为13.3%,差异有统计学意义。该研究同时指出,术前较大的后凸角度和较大的后凸矫正率与PJK的发生有关,因此,推荐术中使用横突钩来预防PJK发生。Boeckenfoerde等[27]纳入了192例接受PSF的AIS患者,研究发现,切除棘突不会对PJK的发生造成显著影响,术前胸椎后凸过大、弯棒角(rod contouring angle)较大及PJA- 弯棒角不匹配是PJK发生的危险因素(图 1[27]),因此,强调弯棒时既不能太直也不能角度过大,特别是在内固定近端,应选择合适的弯棒角度以匹配脊柱序列。Clément等[28]的研究也证实,PJK的发生与随访时胸椎后凸不足有关。通过适当增加胸椎后凸和选择性胸椎融合(保留近端腰椎活动度)可显著降低PJK的发生率。
|
图 1 近端交界区后凸角与弯棒角示意图[27] Fig 1 Schematic diagram of proximal junctional angle and rod contouring angle[27] Proximal junctional angle is the included angle between the lower endplate of the UIV and the upper endplate of the second vertebral body above the UIV, and rod contouring angle is the angle between the upper endplate of UIV and the lower endplate of the first vertebral body below UIV. UIV: Upper instrumented vertebra. |
3 DJK 3.1 定义及发生率
DJK是指脊柱内固定节段远端交界区后凸畸形逐渐增大的现象,由于脊柱机械应力增加,DJK可以导致邻近节段的疼痛、椎间盘退变、矢状面失衡及外观畸形,是AIS脊柱融合术的常见并发症之一。DJK这一概念首次由Lowe等[16]提出,目前常用的诊断标准为:LIV上终板与其下方第1个椎体(LIV+1)下终板之间的矢状面夹角≥10°,且与术前相比增大至少10°则诊断为DJK[29]。研究表明,DJK在舒尔曼病和成人脊柱侧凸患者中多见,AIS患者发生DJK的风险相对较低,为0.2%~15%[30, 31, 32, 33]。
3.2 危险因素分析及预防措施LIV是AIS患者术后是否发生DJK的重要影响因素。矢状面稳定椎(sagittal stable vertebra,SSV)是指矢状面被骶骨后上角垂线平分的主弯下方的第1个椎体,SSV这一概念的提出对于预防DJK具有重要的临床意义。Marciano等[34]研究发现,对于以胸弯为主(Lenke 1~3型)的B型和C型AIS患者,若融合节段未延伸至SSV,术后2年发生DJK的风险与SSV组相比明显升高(45.5% vs 7.7%),因此推荐胸弯AIS患者的融合节段应尽量融合至SSV或其以下节段。Segal等[35]的研究也证实了融合至SSV的重要性,该研究还发现术后远端交界角(distal junctional angle)≥5 °是DJK的另一危险因素,其可以使DJK发生率增加16倍。此外,该研究中发生DJK的患者LIV几乎全部位于胸腰段(T11~L1),因此,建议对于伴有DJK高危因素的AIS患者,LIV应慎重选择在胸腰段。另一项针对Lenke 1型或2型AIS患者的研究表明,当LIV位于L1或以上椎体时,PSF治疗后DJK的总体发生率为6.6%,若LIV未固定至SSV,术后胸椎后凸≥25°或术后胸腰段后凸≥10°也是DJK发生的高危因素[36],因此,建议此类患者LIV未固定至SSV时,术中矫形时应使胸椎后凸<25°且胸腰段后凸<10°。对于准备接受选择性胸椎融合的AIS患者,Yang等[37]认为LIV选择SSV或SSV下方椎体是手术的最佳策略。Banno等[13]发现Lenke 1A和2A型AIS患者选择LIV时,其下方椎间盘处于前凸状态能有效避免DJK的发生。
文献中关于DJK其他危险因素的报道较为少见。Lowe等[33]证明术后T10~L2过度后凸是发生DJK的危险因素;此外,与前路手术相比,后路手术DJK的发生率较高(14.6% vs 4.2%),这可能与后路手术破坏了脊柱后方韧带结构有关。
4 冠状面失衡 4.1 定义、发生率及自然史冠状面失衡(coronal imbalance)是指冠状面上C7铅垂线到骶骨中垂线的水平距离,即冠状面平衡距离(coronal balance distance,CBD)超过一定范围,导致躯干倾斜的现象。目前关于冠状面失衡的诊断标准存在一定争议。研究表明CBD≥2 cm时脊柱畸形更易进展,因此,Zhang等[38]在研究中将冠状面失衡定义为CBD≥2 cm;而Lowe等[39]在对成人脊柱侧凸进行分型研究时将CBD≥3 cm作为冠状面失衡的标准;另有学者认为,CBD≥4 cm时患者的疼痛和功能障碍评分变化显著,因此CBD≥4 cm可作为诊断冠状面失衡的标准[40]。
冠状面失衡是AIS矫形手术的常见并发症,也是影响AIS患者术后外观和手术满意度的重要原因。文献中报道的AIS患者在后路矫形术后冠状面失衡发生率差异较大,与侧弯类型、融合节段、判断标准等因素有关。研究表明,术后即刻冠状面失衡的发生率可高达50%[41],但多数患者可在随访过程中自发纠正。若冠状面失衡持续存在,则称为持续性冠状面失衡,文献报道其发生率为2%~ 14%[42],此类患者往往需要进行翻修手术。术后冠状面失衡具有很强的自我纠正趋势,在一项纳入954例AIS患者的研究中,术后即刻冠状面失衡的发生率为31.1%,术后6个月降至17.5%,术后2年随访时为12%[43]。另一项研究表明,AIS患者冠状面失衡发生率从术后2年时的17% 降至术后5年随访时的6%,提示冠状面失衡在术后5年内能够逐渐纠正[44]。
4.2 危险因素分析及预防措施Hwang等[45]对50例接受选择性腰椎融合的Lenke 5C型AIS患者研究发现,28% 的患者在术后早期发生冠状面失衡,术前胸腰弯/ 腰弯的灵活性较低、胸腰段后凸较大及远端交界角较大是Lenke 5C型AIS患者术后发生冠状面失衡的预测因素。虽然此类患者术后早期可能发生冠状面失衡,但随着LIV倾斜度减小,大部分冠状面失衡能自发纠正。Banno等[42]对以腰弯为主的Lenke 5C或6C型AIS患者进行研究发现,术后发生持续性冠状面失衡的危险因素包括术前胸腰弯/ 腰弯的顶椎偏距(apical vertebra translation)较大(≥49.5 mm)、术后即刻冠状面失衡(即C7铅垂线与骶骨中垂线的距离<-27.5 mm)及年龄较大。Yang等[46]纳入80例Lenke 5、6型AIS患者的研究发现,术前弯曲位X线片检查中L5倾斜是术后发生冠状面失衡的重要危险因素。Bao等[47]研究发现,术前存在凸侧冠状面失衡的胸腰弯/ 腰弯脊柱侧凸患者术后更容易发生冠状面失衡。Shetty等[48]认为,术前LIV倾斜≥25°是Lenke 5C型AIS患者术后发生冠状面失衡的危险因素,而术后UIV倾斜可能是为了代偿冠状面失衡。
Jiang等[49]研究发现,Lenke 1、2型AIS患者STF治疗后冠状面失衡的发生率较高,腰弯修正C型患者冠状面失衡的发生率(42.5%)高于A型(34.8%)和B型(30.0%),A型患者能够通过远端叠加来代偿冠状面失衡,而B型或C型患者可以通过腰弯的自发矫正来代偿冠状面失衡。OhrtNissen等[50]对接受STF的Lenke 1型AIS患者进行研究发现,术后2年冠状面失衡发生率为13%,主胸弯的过度矫正可能是术后冠状面失衡的危险因素,因此建议术中应避免过度矫正。Gomez等[51]发现,PSF治疗后2年6.4% 的AIS患者出现冠状面失衡,该研究同时指出,骨骼发育不成熟、男性和主弯矫正率低可能与冠状面失衡有关。由于大部分AIS患者的冠状面失衡会自我纠正,因此文献主要集中于危险因素分析和机制探讨方面,而对于预防措施和治疗的报道较少。
5 PSI 5.1 定义及发生率PSI是AIS矫形术后的主要并发症之一,显著影响患者的外观和自我满意度。目前普遍将双肩高度差≥1 cm作为PSI的诊断标准。临床上用于评价双肩平衡的指标较多,主要分为影像学评价指标与临床外观评价指标。目前普遍采用Kuklo等[52]提出的分级标准,利用站立位X线片测量肩锁关节上方软组织影来评价双肩的高度差,<1 cm为双肩平衡,1~2 cm为轻度失衡,>2~3 cm为中度失衡,>3 cm为重度失衡。除此之外,影像学评价指标还包括锁骨角、T1倾斜角、喙突高度差、斜方肌长度、第一肋- 锁骨高度差、锁骨胸廓角度差等。临床外观评价指标包括斜方肌丰满度、左侧肋骨突出度、左肩抬高程度、内侧双肩高度差、外侧双肩高度差、肩部面积指数、肩角及腋窝角等。目前对于使用哪种指标来评估双肩平衡情况并无一致观点,但大部分学者认为在进行影像学测量的同时要注重大体测量,大体测量可作为手术决策时影像学评估的一种补充。文献报道,AIS矫形术后PSI的发生率为16%~38%[53, 54, 55]。
5.2 危险因素分析及预防措施研究表明,术前双肩平衡情况及上胸弯、主胸弯的矫形程度对于PSI起关键作用[53, 56]。Suk等[57]使用椎弓根螺钉系统对AIS患者进行矫形发现,仅融合主胸弯左肩平均抬高17 mm,术前双肩平衡情况及上胸弯矫形是保证术后双肩平衡的重要因素。Rose和Lenke[58]建议,对于非结构性上胸弯,若术前右肩高则不需融合上胸弯,UIV选择T4或T5;如术前双肩平衡,则需要选择至T3;若术前左肩高,则需固定至T1或T2。对于结构性上胸弯,如果术前左肩高,需要固定到T2;若术前双肩平衡,可部分融合上胸弯至T3;而如果术前右肩高,考虑到上胸弯的柔韧性较差,仍需部分融合上胸弯至T3。目前这一处理原则在临床中得到广泛应用,并取得良好效果。
Sato等[59]开展了一项纳入99例Lenke 1A型AIS患者的多中心回顾性研究,所有患者UIV选择T2,结果显示术后即刻PSI的发生率为27.3%,术后2年随访时为17.2%,LIV位于LTV下方、主胸弯矫正率过高是PSI的危险因素,因此,建议当UIV位于T2时,应注意避免同时有这2个危险因素。Yang等[60]认为,上胸弯术后顶椎偏距过大和叠加角度是AIS患者PSI的主要危险因素,使患者PSI的发生率明显增高,为了预防PSI,建议术中对上胸弯的顶椎偏距进行充分矫正,同时防止术后上胸弯叠加发生。Isogai等[61]对Lenke 2型AIS患者的研究发现,手术时UIV选择T1且患者Risser分级≥ 3级也是PSI的重要危险因素。Yagi等[55]对85例接受胸椎融合术的AIS患者资料进行回顾性分析,有25% 接受手术治疗的患者出现PSI,该研究发现,锁骨胸廓角度差和主胸弯顶椎偏距是PSI的独立危险因素。Sielatycki等[62]针对Lenke 1、2型AIS患者的研究表明,不管UIV如何选择,当主胸弯矫正良好(矫正率>54%)但上胸弯矫正欠佳(矫正率<52%)时,患者PSI的发生率高达59%,因此,建议当主胸弯矫正率过大时,应引起足够重视,术中需仔细矫正上胸弯以防止PSI的发生。
6 总结和展望AIS是最常见的脊柱侧凸类型,畸形进行性加重会对青少年的身体和心理健康造成严重危害。随着医疗技术和手术器械的发展,PSF治疗AIS已经是一种相对安全、有效的手术方式,但手术治疗仍无法避免并发症的出现。本文对术后畸形相关并发症进行总结,叠加现象、PJK、DJK、冠状面失衡和PSI是术后最常发生、研究最多的并发症,术后处理不当将会引起灾难性后果,因此,了解这些并发症的流行病学特点、诱发因素和发展规律对于手术决策至关重要。虽然越来越多的先进医疗设备和技术应用于脊柱侧凸矫形手术,但仍需要大量的高级别循证医学证据对AIS手术相关并发症的病因、发病机制和防治策略进行深入探讨,为今后更好地开展AIS诊疗工作提供依据。
| [1] |
KONIECZNY M R, SENYURT H, KRAUSPE R. Epidemiology of adolescent idiopathic scoliosis[J]. J Child Orthop, 2013, 7(1): 3-9. DOI:10.1007/s11832-012-0457-4 |
| [2] |
DUNN J, HENRIKSON N B, MORRISON C C, et al. Screening for adolescent idiopathic scoliosis: evidence report and systematic review for the US preventive services task force[J]. JAMA, 2018, 319(2): 173-187. DOI:10.1001/jama.2017.11669 |
| [3] |
BUNNELL W P. The natural history of idiopathic scoliosis before skeletal maturity[J]. Spine (Phila Pa 1976), 1986, 11(8): 773-776. DOI:10.1097/00007632-198610000-00003 |
| [4] |
US PREVENTIVE SERVICES TASK FORCE, GROSSMAN D C, CURRY S J, et al. Screening for adolescent idiopathic scoliosis: us preventive services task force recommendation statement[J]. JAMA, 2018, 319(2): 165-172. DOI:10.1001/jama.2017.19342 |
| [5] |
HICKS J M, SINGLA A, SHEN F H, et al. Complications of pedicle screw fixation in scoliosis surgery: a systematic review[J]. Spine (Phila Pa 1976), 2010, 35(11): E465-E470. DOI:10.1097/BRS.0b013e3181d1021a |
| [6] |
KEIL L G, HIMMELBERG S M, GUISSÉ N F, et al. Complications following posterior spinal fusion for adolescent idiopathic scoliosis: a retrospective cohort study using the modified Clavien-Dindo-Sink system[J]. Spine Deform, 2022, 10(3): 607-614. DOI:10.1007/s43390-021-00468-3 |
| [7] |
BARTLEY C E, YASZAY B, BASTROM T P, et al. Perioperative and delayed major complications following surgical treatment of adolescent idiopathic scoliosis[J]. J Bone Joint Surg Am, 2017, 99(14): 1206-1212. DOI:10.2106/JBJS.16.01331 |
| [8] |
JOO Y S, HWANG C J, CHO J H, et al. Does sacral slanting affect distal adding-on in Lenke type 1A adolescent idiopathic scoliosis?[J]. Spine (Phila Pa 1976), 2018, 43(17): E990-E997. DOI:10.1097/BRS.0000000000002722 |
| [9] |
SUK S I, LEE S M, CHUNG E R, et al. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis[J]. Spine (Phila Pa 1976), 2003, 28(5): 484-491. DOI:10.1097/01.BRS.0000048653.75549.40 |
| [10] |
MATSUMOTO M, WATANABE K, HOSOGANE N, et al. Postoperative distal adding-on and related factors in Lenke type 1A curve[J]. Spine (Phila Pa 1976), 2013, 38(9): 737-744. DOI:10.1097/BRS.0b013e318279b666 |
| [11] |
YANG M, ZHAO Y, YIN X, et al. Prevalence, risk factors, and characteristics of the "adding-on" phenomenon in idiopathic scoliosis after correction surgery: a systematic review and meta-analysis[J]. Spine (Phila Pa 1976), 2018, 43(11): 780-790. DOI:10.1097/BRS.0000000000002423 |
| [12] |
FUJII T, KAWABATA S, SUZUKI S, et al. Can postoperative distal adding-on be predicted in Lenke type 1B and 1C curves with intraoperative radiographs?[J]. Spine (Phila Pa 1976), 2022, 47(6): E215-E221. DOI:10.1097/BRS.0000000000004174 |
| [13] |
BANNO T, YAMATO Y, HASEGAWA T, et al. Optimal lowest instrumented vertebra selection with consideration of coronal and sagittal planes to prevent distal junctional complications in patients with Lenke type 1A and 2A adolescent idiopathic scoliosis[J]. Spine Deform, 2023, 11(5): 1145-1156. DOI:10.1007/s43390-023-00692-z |
| [14] |
WANG Y, HANSEN E S, HØY K, et al. Distal adding-on phenomenon in Lenke 1A scoliosis: risk factor identification and treatment strategy comparison[J]. Spine (Phila Pa 1976), 2011, 36(14): 1113-1122. DOI:10.1097/BRS.0b013e3181f51e95 |
| [15] |
CHO R H, YASZAY B, BARTLEY C E, et al. Which Lenke 1A curves are at the greatest risk for adding-on... and why?[J]. Spine (Phila Pa 1976), 2021, 37(16): 1384-1390. DOI:10.1097/BRS.0b013e31824bac7a |
| [16] |
LOWE T G, KASTEN M D. An analysis of sagittal curves and balance after Cotrel-Dubousset instrumentation for kyphosis secondary to Scheuermann's disease. A review of 32 patients[J]. Spine (Phila Pa 1976), 1984, 19(15): 1680-1685. DOI:10.1097/00007632-199408000-00005 |
| [17] |
GLATTES R C, BRIDWELL K H, LENKE L G, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis[J]. Spine (Phila Pa 1976), 2005, 30(14): 1643-1649. DOI:10.1097/01.brs.0000169451.76359.49 |
| [18] |
LEE G A, BETZ R R, CLEMENTS D H 3rd, et al. Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis[J]. Spine (Phila Pa 1976), 1999, 24(8): 795-799. DOI:10.1097/00007632-199904150-00011 |
| [19] |
LONNER B S, REN Y, NEWTON P O, et al. Risk factors of proximal junctional kyphosis in adolescent idiopathic scoliosis-the pelvis and other considerations[J]. Spine Deform, 2017, 5(3): 181-188. DOI:10.1016/j.jspd.2016.10.003 |
| [20] |
FERRERO E, BOCAHUT N, LEFEVRE Y, et al. Proximal junctional kyphosis in thoracic adolescent idiopathic scoliosis: risk factors and compensatory mechanisms in a multicenter national cohort[J]. Eur Spine J, 2018, 27(9): 2241-2250. DOI:10.1007/s00586-018-5640-y |
| [21] |
WANG G, LI Y, LIU P, et al. Pelvic incidence correlates to sagittal spinal morphology in Lenke 5 adolescent idiopathic scoliosis and influences the proximal junctional kyphosis rate after correction surgery[J]. Eur Spine J, 2021, 30(9): 2457-2466. DOI:10.1007/s00586-021-06749-9 |
| [22] |
KIM Y J, BRIDWELL K H, LENKE L G, et al. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up[J]. Spine (Phila Pa 1976), 2005, 30(18): 2045-2050. DOI:10.1097/01.brs.0000179084.45839.ad |
| [23] |
KIM Y J, LENKE L G, BRIDWELL K H, et al. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases[J]. Spine (Phila Pa 1976), 2007, 32(24): 2731-2738. DOI:10.1097/BRS.0b013e31815a7ead |
| [24] |
WANG J, ZHAO Y, SHEN B, et al. Risk factor analysis of proximal junctional kyphosis after posterior fusion in patients with idiopathic scoliosis[J]. Injury, 2010, 41(4): 415-420. DOI:10.1016/j.injury.2010.01.001 |
| [25] |
李庆达, 贺宝荣, 惠华, 等. Lenke 5型青少年特发性脊柱侧凸术后近端交界性后凸发生的相关因素分析[J]. 中华医学杂志, 2023, 103(29): 2239-2245. DOI:10.3760/cma.j.cn112137-20221209-02607 |
| [26] |
ERKILINC M, COATHUP M, LISKA M G, et al. Can placement of hook at the upper instrumented level decrease the proximal junctional kyphosis risk in adolescent idiopathic scoliosis?[J]. Eur Spine J, 2023, 32(9): 3113-3117. DOI:10.1007/s00586-023-07803-4 |
| [27] |
BOECKENFOERDE K, SCHULZE BOEVINGLOH A, GOSHEGER G, et al. Risk factors of proximal junctional kyphosis in adolescent idiopathic scoliosis-the spinous processes and proximal rod contouring[J]. J Clin Med, 2022, 11(20): 6098. DOI:10.3390/jcm11206098 |
| [28] |
CLÉMENT J L, PESENTI S, ILHARREBORDE B, et al. Proximal junctional kyphosis is a rebalancing spinal phenomenon due to insufficient postoperative thoracic kyphosis after adolescent idiopathic scoliosis surgery[J]. Eur Spine J, 2021, 30(7): 1988-1997. DOI:10.1007/s00586-021-06875-4 |
| [29] |
GHASEMI A, STUBIG T, NASTO L A, et al. Distal junctional kyphosis in patients with Scheuermann's disease: a retrospective radiographic analysis[J]. Eur Spine J, 2017, 26(3): 913-920. DOI:10.1007/s00586-016-4924-3 |
| [30] |
AMERI E, BEHTASH H, MOBINI B, et al. The prevalence of distal junctional kyphosis following posterior instrumentation and arthrodesis for adolescent idiopathic scoliosis[J]. Acta Med Iran, 2011, 49(6): 357-363. |
| [31] |
LUHMANN S J, LENKE L G, BRIDWELL K H, et al. Revision surgery after primary spine fusion for idiopathic scoliosis[J]. Spine (Phila Pa 1976), 2009, 34(20): 2191-2197. DOI:10.1097/BRS.0b013e3181b3515a |
| [32] |
CAMPOS M, DOLAN L, WEINSTEIN S. Unanticipated revision surgery in adolescent idiopathic scoliosis[J]. Spine (Phila Pa 1976), 2012, 37(12): 1048-1053. DOI:10.1097/BRS.0b013e31823ced6f |
| [33] |
LOWE T G, LENKE L, BETZ R, et al. Distal junctional kyphosis of adolescent idiopathic thoracic curves following anterior or posterior instrumented fusion: incidence, risk factors, and prevention[J]. Spine (Phila Pa 1976), 2006, 31(3): 299-302. DOI:10.1097/01.brs.0000197221.23109.fc |
| [34] |
MARCIANO G, BALL J, MATSUMOTO H, et al. Including the stable sagittal vertebra in the fusion for adolescent idiopathic scoliosis reduces the risk of distal junctional kyphosis in Lenke 1-3 B and C curves[J]. Spine Deform, 2021, 9(3): 733-741. DOI:10.1007/s43390-020-00259-2 |
| [35] |
SEGAL D N, BALL J, FLETCHER N D, et al. Risk factors for the development of DJK in AIS patients undergoing posterior spinal instrumentation and fusion[J]. Spine Deform, 2022, 10(2): 377-385. DOI:10.1007/s43390-021-00413-4 |
| [36] |
WANG P Y, CHEN C W, LEE Y F, et al. Distal junctional kyphosis after posterior spinal fusion in Lenke 1 and 2 adolescent idiopathic scoliosis-exploring detailed features of the sagittal stable vertebra concept[J]. Global Spine J, 2023, 13(4): 1112-1119. DOI:10.1177/21925682211019692 |
| [37] |
YANG J, ANDRAS L M, BROOM A M, et al. Preventing distal junctional kyphosis by applying the stable sagittal vertebra concept to selective thoracic fusion in adolescent idiopathic scoliosis[J]. Spine Deform, 2018, 6(1): 38-42. DOI:10.1016/j.jspd.2017.06.007 |
| [38] |
ZHANG Z, SONG K, WU B, et al. Coronal imbalance in adult spinal deformity following posterior spinal fusion with instrument: a related parameters analysis[J]. Spine (Phila Pa 1976), 2019, 44(8): 550-557. DOI:10.1097/BRS.0000000000002897 |
| [39] |
LOWE T, BERVEN S H, SCHWAB F J, et al. The SRS classification for adult spinal deformity: building on the King/Moe and Lenke classification systems[J]. Spine (Phila Pa 1976), 2006, 31(19 Suppl): S119-S125. DOI:10.1097/01.brs.0000232709.48446.be |
| [40] |
PLOUMIS A, LIU H, MEHBOD A A, et al. A correlation of radiographic and functional measurements in adult degenerative scoliosis[J]. Spine (Phila Pa 1976), 2009, 34(15): 1581-1584. DOI:10.1097/BRS.0b013e31819c94cc |
| [41] |
CHEN K, BAI J, YANG Y, et al. Immediate postoperative coronal imbalance in Lenke 5 and Lenke 6 adolescent idiopathic scoliosis: is it predictable?[J]. Eur Spine J, 2019, 28(9): 2042-2052. DOI:10.1007/s00586-019-06019-9 |
| [42] |
BANNO T, YAMATO Y, OBA H, et al. Risk factors and clinical impact of persistent coronal imbalance after posterior spinal fusion in thoracolumbar/lumbar idiopathic scoliosis[J]. J Neurosurg Spine, 2022, 37(6): 883-892. DOI:10.3171/2022.5.SPINE22385 |
| [43] |
ANARI J B, TATAD A, CAHILL P J, et al. The impact of posterior spinal fusion (PSF) on coronal balance in adolescent idiopathic scoliosis (AIS): a new classification and trends in the postoperative period[J]. J Pediatr Orthop, 2020, 40(9): e788-e793. DOI:10.1097/BPO.0000000000001622 |
| [44] |
HUGHES J, BASTROM T P, BARTLEY C E, et al. Radiographic coronal imbalance and shoulder asymmetry continue to improve between 2 and 5 years following surgery of adolescent idiopathic scoliosis[J]. J Pediatr Orthop, 2021, 41(7): e512-e516. DOI:10.1097/BPO.0000000000001856 |
| [45] |
HWANG C J, LEE C S, KIM H, et al. Spontaneous correction of coronal imbalance after selective thoracolumbar-lumbar fusion in patients with Lenke-5C adolescent idiopathic scoliosis[J]. Spine J, 2018, 18(10): 1822-1828. DOI:10.1016/j.spinee.2018.03.013 |
| [46] |
YANG C, ZHAO Y, ZHAI X, et al. Coronal balance in idiopathic scoliosis: a radiological study after posterior fusion of thoracolumbar/lumbar curves (Lenke 5 or 6)[J]. Eur Spine J, 2017, 26(6): 1775-1781. DOI:10.1007/s00586-016-4844-2 |
| [47] |
BAO H, YAN P, QIU Y, et al. Coronal imbalance in degenerative lumbar scoliosis: prevalence and influence on surgical decision-making for spinal osteotomy[J]. Bone Joint J, 2016, 98-B(9): 1227-1233. DOI:10.1302/0301-620X.98B9.37273 |
| [48] |
SHETTY A P, SURESH S, AIYER S N, et al. Radiological factors affecting post-operative global coronal balance in Lenke 5 C scoliosis[J]. J Spine Surg, 2017, 3(4): 541-547. DOI:10.21037/jss.2017.09.04 |
| [49] |
JIANG H, SHAO W, XU E, et al. Coronal imbalance after selective posterior thoracic fusion in patients with Lenke 1 and 2 adolescent idiopathic scoliosis[J]. Biomed Res Int, 2018, 2018: 3476425. DOI:10.1155/2018/3476425 |
| [50] |
OHRT-NISSEN S, CHEUNG P W H, KAWASAKI S, et al. Curve overcorrection predicts coronal imbalance in selective thoracic fusion in adolescent idiopathic scoliosis[J]. Global Spine J, 2024, 14(3): 856-861. DOI:10.1177/21925682221124526 |
| [51] |
GOMEZ J A, MATSUMOTO H, COLACCHIO N D, et al. Risk factors for coronal decompensation after posterior spinal instrumentation and fusion in adolescent idiopathic scoliosis[J]. Spine Deform, 2014, 2(5): 380-385. DOI:10.1016/j.jspd.2014.05.001 |
| [52] |
KUKLO T R, LENKE L G, GRAHAM E J, et al. Correlation of radiographic, clinical, and patient assessment of shoulder balance following fusion versus nonfusion of the proximal thoracic curve in adolescent idiopathic scoliosis[J]. Spine (Phila Pa 1976), 2002, 27(18): 2013-2020. DOI:10.1097/00007632-200209150-00009 |
| [53] |
LEE C K, DENIS F, WINTER R B, et al. Analysis of the upper thoracic curve in surgically treated idiopathic scoliosis. A new concept of the double thoracic curve pattern[J]. Spine (Phila Pa 1976), 1993, 18(12): 1599-1608. DOI:10.1097/00007632-199309000-00006 |
| [54] |
LI M, GU S, NI J, et al. Shoulder balance after surgery in patients with Lenke type 2 scoliosis corrected with the segmental pedicle screw technique[J]. J Neurosurg Spine, 2009, 10(3): 214-219. DOI:10.3171/2008.11.SPINE08524 |
| [55] |
YAGI M, TAKEMITSU M, MACHIDA M. Chest cage angle difference and rotation of main thoracic curve are independent risk factors of postoperative shoulder imbalance in surgically treated patients with adolescent idiopathic scoliosis[J]. Spine (Phila Pa 1976), 2013, 38(19): E1209-E1215. DOI:10.1097/BRS.0b013e31829e0309 |
| [56] |
WINTER R B. The idiopathic double thoracic curve pattern. Its recognition and surgical management[J]. Spine (Phila Pa 1976), 1989, 14(12): 1287-1292. DOI:10.1097/00007632-198912000-00003 |
| [57] |
SUK S I, KIM W J, LEE C S, et al. Indications of proximal thoracic curve fusion in thoracic adolescent idiopathic scoliosis: recognition and treatment of double thoracic curve pattern in adolescent idiopathic scoliosis treated with segmental instrumentation[J]. Spine (Phila Pa 1976), 2000, 25(18): 2342-2349. DOI:10.1097/00007632-200009150-00012 |
| [58] |
ROSE P S, LENKE L G. Classification of operative adolescent idiopathic scoliosis: treatment guidelines[J]. Orthop Clin North Am, 2007, 38(4): 521-529, vi. DOI:10.1016/j.ocl.2007.06.001 |
| [59] |
SATO T, YONEZAWA I, MATSUMOTO H, et al. Surgical predictors for prevention of postoperative shoulder imbalance in Lenke type 2A adolescent idiopathic scoliosis[J]. Spine (Phila Pa 1976), 2022, 47(4): E132-E141. DOI:10.1097/BRS.0000000000004135 |
| [60] |
YANG Y, YANG M, ZHAO J, et al. Postoperative shoulder imbalance in adolescent idiopathic scoliosis: risk factors and predictive index[J]. Eur Spine J, 2019, 28(6): 1331-1341. DOI:10.1007/s00586-019-05933-2 |
| [61] |
ISOGAI N, YAGI M, OTOMO N, et al. Upper end vertebra of proximal thoracic curve at T1 is a novel risk factor of postoperative shoulder imbalance in Lenke type 2 adolescent idiopathic scoliosis[J]. Global Spine J, 2023, 13(5): 1223-1229. DOI:10.1177/21925682211023049 |
| [62] |
SIELATYCKI J A, CERPA M, BEAUCHAMP E C, et al. The amount of relative curve correction is more important than upper instrumented vertebra selection for ensuring postoperative shoulder balance in Lenke type 1 and type 2 adolescent idiopathic scoliosis[J]. Spine (Phila Pa 1976), 2019, 44(17): E1031-E1037. DOI:10.1097/BRS.0000000000003088 |
 2024, Vol. 45
2024, Vol. 45


