2. 海军军医大学(第二军医大学)基础医学院学员四大队, 上海 200433
2. The Fourth Student Team, College of Basic Medical Sciences, Naval Medical University (Second Military Medical University), Shanghai 200433, China
QT间期是指从心室除极开始到心室复极结束的总时间,即QRS波群起始到T波结束的时间[1]。QT间期的正常值随心率而变化。随着心率的增加QT间期缩短,而心动过缓时则延长。因此,QT间期需要校正,校正后的QT间期称为QTc。QT间期延长的诊断标准为女性QTc>480 ms,男性QTc>470 ms[1]。QTc延长与尖端扭转型室性心动过速(torsade de pointes,TDP)相关[2],TDP是一种多形性室性心动过速,可进展为心室颤动导致患者死亡。QT间期延长的病因很多,基因异常[3]、心肌缺血[4]、严重颅内损伤[5]、电解质紊乱[6]和某些药物(如Ⅰa类与Ⅲ类抗心律失常药、大环内酯类药物、三环类抗抑郁药、喹诺酮类药物、抗精神病药和止吐药等)[7-11]均可导致QT间期延长。500 ms以上的长QT间期患者出现心律失常的风险明显增加[12-13]。本研究拟分析住院期间心电图检查发现QTc≥500 ms患者的科室分布及引起QT间期延长的病因,为预防QT间期延长和可能发生的TDP提供依据。
1 资料和方法 1.1 临床资料回顾性分析2019年1月30日至2022年7月27日在海军军医大学(第二军医大学)第一附属医院接受心电图检查且诊断为长QT间期(QTc≥500 ms)的住院患者的临床资料。
1.2 心电图分析住院患者的心电图从海军军医大学(第二军医大学)第一附属医院电子病历系统获取,所有心电图均采用标准测量[14]方法获得,并由2名高年资主治医师分别进行诊断。重点关注住院患者心电图的QT间期。
1.3 统计学处理应用SPSS 23.0软件进行统计学分析。呈正态分布的计量资料以x±s表示,两组间比较采用独立样本t检验;计数资料以例数和百分数表示。检验水准(α)为0.05。
2 结果 2.1 患者的基线资料共有61例住院患者入选,平均年龄为(64.2±15.3)岁,男34例(55.7%)、女27例(44.3%),患者既往病史和心电图改变见表 1。患者的平均QT间期为(494.1±59.0)ms,平均QTc为(551.8±64.2)ms。男性和女性患者QTc的差异无统计学意义[(552.3±69.9)ms vs(551.2±57.5)ms,t=0.066,P=0.947]。61例QT间期延长的患者中有6例于住院期间死亡。16例病因为冠心病的QT间期延长患者的心电图以非ST段抬高(9例)为主,其中Wellen综合征8例,非Wellen综合征1例;ST段抬高患者有7例,其中前间壁2例,广泛前壁2例,下壁3例。
|
|
表 1 QT间期延长住院患者的基线资料和心电图特征 |
2.2 QT间期延长患者的住院科室分布
61例QT间期延长患者的住院科室主要集中于急诊科(28例,45.9%)和心血管内科(19例,31.1%),其余散在分布于其他科室,心血管外科3例(4.9%),烧伤科2例(3.3%),血液科、肿瘤科、呼吸内科、消化内科、肾内科、神经内科、神经外科、普外科、介入科各1例(1.6%)。
2.3 QT间期延长的病因61例住院患者出现QT间期延长的病因主要为药物(27例,44.3%)、冠心病(16例,26.2%)及电解质紊乱(15例,24.6%),其余9.8%(6例)为急性颅内病变,1.6%(1例)为先天性长QT间期综合征及8.2%(5例)未知原因。引起延长QT间期的药物中,常见的为Ⅲ类抗心律失常药(胺碘酮9例)、抗生素(喹诺酮类4例,大环内酯类3例)、5-羟色胺受体拮抗剂(雷莫司琼3例,托烷司琼1例,帕洛诺司琼1例)、抗真菌药(伏立康唑1例,卡泊芬净3例,均为静脉用药)、抗惊厥药(4例)、三环类抗抑郁药(1例)及抗精神病药(1例)。
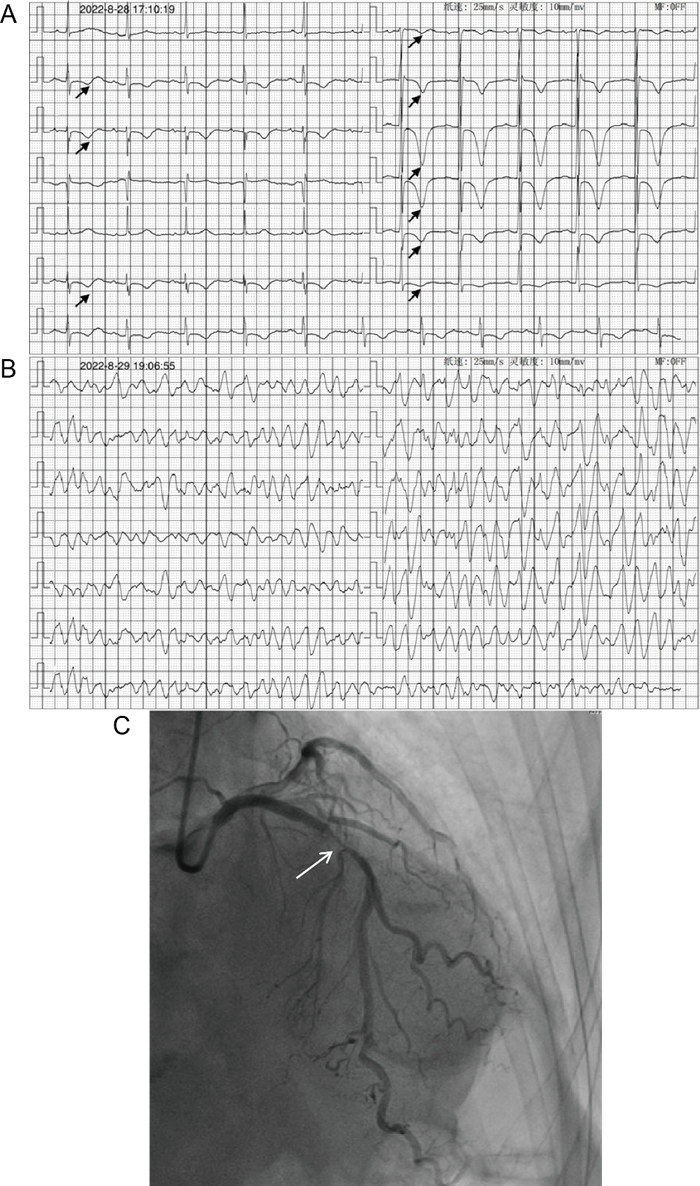
2.4 住院期间QT间期延长患者心律失常的发生情况住院期间3例(4.9%,3/61)QT间期延长患者发生了TDP,其中2例经及时治疗及去除病因后治愈出院(图 1),1例抢救无效死亡。
|
图 1 QT间期延长引发TDP 患者女,78岁.A:心电图(2022-08-28 17:10)示窦性心律(64 min-1),PR间期230 ms,QRS波时限90 ms,巨大T波深倒置(Ⅱ、Ⅲ、aVF、V1~V6导联,箭头所示)伴QT间期延长(QT间期500 ms,QTc 520 ms);B:心电图(2022-08-29 19:06)示RS波提前发生,宽大畸形形态多变,频率约300 min-1,节律不规则,QRS主波围绕基线上下扭转,QRS波群前无P波,为TDP;C:冠状动脉造影(2022-08-29 18:10)(体位:右前斜位30°+头位29°)示左主干未见明显狭窄,前降支近中段发出第二对角支处次全闭塞(箭头所示),回旋支中段狭窄约30%,右冠状动脉近中段斑块浸润,狭窄10%~30%.TDP:尖端扭转型室性心动过速;QTc:校正后的QT间期. |
2.5 QT间期延长住院患者的死亡原因
QT间期延长的住院患者中有6例(9.8%)死亡,其中3例死于心脏疾病,1例死于重症肺炎,1例死于脑出血,1例死于晚期结肠癌。死于重症肺炎的1例患者在住院期间长时间使用了阿奇霉素,后发生TDP,最终抢救无效死亡。
3 讨论QT间期延长分为先天性和获得性两大类[15]。临床上获得性QT间期延长较先天性更常见,本研究QT间期延长的61例住院患者中,仅1例(1.6%)为先天性长QT间期综合征,其余患者均考虑获得性QT间期延长,大多存在可以纠正的原因。无论是先天性还是获得性QT间期延长,均可能出现TDP而导致患者晕厥或猝死。在临床诊疗过程中关注QT间期,及时发现并纠正引起QT间期延长的病因,可以避免长QT间期导致的恶性心律失常发生。
药物是获得性QT间期延长最常见的原因,多数患者暴露于单一药物,也有部分患者暴露于多种药物[15-17]。有研究估计,5%~7%的室性心动过速、心室颤动或心源性猝死是由药物引起的长QT间期和TDP所致[18]。抑制延迟整流钾通道的快速激活部分,延长心肌动作电位时程和有效不应期是临床上药物导致QT间期延长的主要药效机制[19]。离子通道表达模式的变化导致早期后除极,早期后除极优先出现在心肌M细胞和浦肯野细胞中,如果同时合并复极离散度显著增加,早期后除极诱发的早搏会触发TDP[20]。潜在遗传背景也可能发挥一定作用,钾电压门控通道亚家族E调节亚基(potassium voltage-gated channel subfamily E regulatory subunit,KCNE)2(T8A)基因多态性[21]和钠电压门控通道α亚基5(sodium voltage-gated channel α subunit 5,SCN5A)钠离子通道突变(L1825P)[22]可能与药物诱导的长QT间期综合征有关。
在药物诱导的长QT间期综合征的情况下,药代动力学药物效应可单独或联合作用而进一步延长QT间期[23]。胺碘酮是本研究中最常见的延长QT间期的药物,尽管QT间期延长30~60 ms,但研究表明,胺碘酮能抑制INa、ICaL、INa-CaR、IKr和IKs等离子通道,虽然心室复极时间延长,导致QT间期显著延长30~60 ms,但由于逆转跨壁复极离散度,心电相对稳定,很少引起TDP,发生率<1%[24]。其他常见的药物包括抗生素及抗精神病药等[25]。临床上使用可能引起QT间期延长的药物时,建议监测心电图QT间期[26],一旦发现QT间期延长,应及时停药以避免TDP。引起QT间期延长是药物退出市场最常见的原因之一[27]。20世纪90年代开始,美国FDA和欧洲药品管理局开始要求临床前和临床药物试验时常规监测药物是否会引起QT间期延长[28]。
本研究发现住院患者中引起QT间期延长的第二大原因为冠心病。Jiménez-Candil等[29]报道非ST段抬高急性冠状动脉综合征患者的QTc延长提示预后不佳。QT间期延长主要发生在急性冠状动脉综合征后的第2天至第11天,发生率为19%~60%[4]。发生心肌缺血时,交感神经过度活跃,通过增加复极离散度,产生后除极,继而增加心室复极化持续时间,从而表现为长QT间期[30]。低血钾等电解质紊乱也是临床常见的引起获得性QT间期延长的原因。住院患者发生的QT间期延长多数是可逆的,因此,管理QT间期延长的基础是识别和及时停用任何延长QT间期的药物,并积极纠正电解质紊乱,如低钾血症和低镁血症等[7-11]。
本研究的61例QT间期延长患者中有6例住院期间死亡。这些患者多有心脏疾病、肿瘤及急性脑血管事件等,全身总体状况差,难以确认死亡原因是否和QT间期延长直接相关。多项研究发现QT间期延长与严重疾病和高死亡率有关,在患有基础心脏疾病的患者中风险最高[31-34]。
由于存在较多的危险因素,住院患者发生TDP的风险显著高于门诊患者[35]。而心血管内科住院患者的风险尤其高,Tisdale等[36]报道入住冠心病ICU的900例患者中,18.2%的患者最初的心电图QTc>500 ms,危险因素包括低钾血症、低镁血症、急性心肌梗死和心力衰竭。Mahmud等[37]报道的712例急诊患者中,50例(7%)患者存在QTc延长,而这些病例中,12%的患者在随后的治疗中使用了引起QT间期延长的药物。本研究中,住院患者QT间期延长主要见于急诊科留观病房及ICU和心血管内科。但其他科室也有发现,几乎涵盖全院各个科室。散在分布于各科室的肿瘤患者,因为使用雷莫司琼等止吐药,也可能发生QT间期延长的情况。各科室均可能会使用红霉素[7-11]、阿奇霉素[9-10]等大环内酯类抗生素及抗真菌药物[38]来抗感染治疗。有些科室及医师可能对QT间期延长的危害认识不足,因此除了心电图室发现QT间期≥550 ms需报危急值外[39],医院的临床药学部门应建立使用可引起QT间期延长药物的预警机制,加强跟踪、监督及技术指导,在医师电子处方系统中设置弹窗提醒,要求用药全程监测心电图QT间期变化,并避免相关药物的联合使用。同时借鉴国外的半定量评分系统[40],如评估KCNE1 D85N和KCNE2 T8A突变基因座水平,进一步研究风险预测模型,并应用于可能延长QT间期药物的处方中来评估风险,避免药物的不良反应。
本研究存在一定的局限性:(1)为回顾性研究,研究结果受到样本选择的影响;(2)研究只纳入了住院患者,没有纳入门急诊患者。
综上所述,本研究结果显示住院患者中QT间期延长多见于急诊科和心血管内科,但几乎所有其他临床科室均可出现。住院患者QT间期延长的病因绝大多数为获得性,主要包括药物、冠心病及电解质紊乱等,是否存在其他潜在影响因素有待后续进一步研究。
| [1] |
TAGGART N W, HAGLUND C M, TESTER D J, et al. Diagnostic miscues in congenital long-QT syndrome[J]. Circulation, 2007, 115(20): 2613-2620. DOI:10.1161/CIRCULATIONAHA.106.661082 |
| [2] |
WARING W S, GRAHAM A, GRAY J, et al. Evaluation of a QT nomogram for risk assessment after antidepressant overdose[J]. Br J Clin Pharmacol, 2010, 70(6): 881-885. DOI:10.1111/j.1365-2125.2010.03728.x |
| [3] |
WALLACE E, HOWARD L, LIU M, et al. Long QT syndrome: genetics and future perspective[J]. Pediatr Cardiol, 2019, 40(7): 1419-1430. DOI:10.1007/s00246-019-02151-x |
| [4] |
HASANIEN A A, DREW B J, HOWIE-ESQUIVEL J. Prevalence and prognostic significance of long QT interval in patients with acute coronary syndrome: review of the literature[J]. J Cardiovasc Nurs, 2014, 29(3): 271-279. DOI:10.1097/JCN.0b013e31829bcf1a |
| [5] |
VALLI G, ROSSI L, VARESI C, et al. Brain stem involvement and long QT interval in transmissible spongiform encephalopathy[J]. Ann N Y Acad Sci, 1994, 724: 363-366. DOI:10.1111/j.1749-6632.1994.tb38933.x |
| [6] |
TIVER K D, DHARMAPRANI D, QUAH J X, et al. Vomiting, electrolyte disturbance, and medications; the perfect storm for acquired long QT syndrome and cardiac arrest: a case report[J]. J Med Case Rep, 2022, 16(1): 9. DOI:10.1186/s13256-021-03204-7 |
| [7] |
FIETS R B, BOS J M, DONDERS A, et al. QTc prolongation during erythromycin used as prokinetic agent in ICU patients[J]. Eur J Hosp Pharm, 2018, 25(3): 118-122. DOI:10.1136/ejhpharm-2016-001077 |
| [8] |
GIUDICESSI J R, ACKERMAN M J, CAMILLERI M. Cardiovascular safety of prokinetic agents: a focus on drug-induced arrhythmias[J]. Neurogastroenterol Motil, 2018, 30(6): e13302. DOI:10.1111/nmo.13302 |
| [9] |
YANG Z, PRINSEN J K, BERSELL K R, et al. Azithromycin causes a novel proarrhythmic syndrome[J]. Circ Arrhythm Electrophysiol, 2017, 10(4): e003560. DOI:10.1161/CIRCEP.115.003560 |
| [10] |
CHOI Y, LIM H S, CHUNG D, et al. Risk evaluation of azithromycin-induced QT prolongation in real-world practice[J]. Biomed Res Int, 2018, 2018: 1574806. DOI:10.1155/2018/1574806 |
| [11] |
RAO G A, MANN J R, SHOAIBI A, et al. Azithromycin and levofloxacin use and increased risk of cardiac arrhythmia and death[J]. Ann Fam Med, 2014, 12(2): 121-127. DOI:10.1370/afm.1601 |
| [12] |
PRIORI S G, SCHWARTZ P J, NAPOLITANO C, et al. Risk stratification in the long-QT syndrome[J]. N Engl J Med, 2003, 348(19): 1866-1874. DOI:10.1056/NEJMoa022147 |
| [13] |
TOMÁS M, NAPOLITANO C, DE GIULI L, et al. Polymorphisms in the NOS1AP gene modulate QT interval duration and risk of arrhythmias in the long QT syndrome[J]. J Am Coll Cardiol, 2010, 55(24): 2745-2752. DOI:10.1016/j.jacc.2009.12.065 |
| [14] |
RAUTAHARJU PM, SURAWICZ B, GETTES L S, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part Ⅳ: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society.Endorsed by the International Society for Computerized Electrocardiology[J]. J Am Coll Cardiol, 2009, 53(11): 982-991. DOI:10.1016/j.jacc.2008.12.014 |
| [15] |
WALKER B D, KRAHN A D, KLEIN G J, et al. Congenital and acquired long QT syndromes[J]. Can J Cardiol, 2003, 19(1): 76-87. |
| [16] |
CHEVALIER P, RODRIGUEZ C, BONTEMPS L, et al. Non-invasive testing of acquired long QT syndrome: evidence for multiple arrhythmogenic substrates[J]. Cardiovasc Res, 2001, 50(2): 386-398. DOI:10.1016/s0008-6363(01)00263-2 |
| [17] |
EL-SHERIF N, TURITTO G, BOUTJDIR M. Acquired long QT syndrome and torsade de pointes[J]. Pacing Clin Electrophysiol, 2018, 41(4): 414-421. DOI:10.1111/pace.13296 |
| [18] |
NIEMEIJER M N, VAN DEN BERG M E, EIJGELSHEIM M, et al. Pharmacogenetics of drug-induced QT interval prolongation: an update[J]. Drug Saf, 2015, 38(10): 855-867. DOI:10.1007/s40264-015-0316-6 |
| [19] |
LI E C, ESTERLY J S, POHL S, et al. Drug-induced QT-interval prolongation: considerations for clinicians[J]. Pharmacotherapy, 2010, 30(7): 684-701. DOI:10.1592/phco.30.7.684 |
| [20] |
HAVERKAMP W, BREITHARDT G, CAMM A J, et al. The potential for QT prolongation and proarrhythmia by non-antiarrhythmic drugs: clinical and regulatory implications.Report on a policy conference of the European Society of Cardiology[J]. Eur Heart J, 2000, 21(15): 1216-1231. DOI:10.1053/euhj.2000.2249 |
| [21] |
SESTI F, ABBOTT G W, WEI J, et al. A common polymorphism associated with antibiotic-induced cardiac arrhythmia[J]. Proc Natl Acad Sci USA, 2000, 97(19): 10613-10618. DOI:10.1073/pnas.180223197 |
| [22] |
MAKITA N, HORIE M, NAKAMURA T, et al. Drug-induced long-QT syndrome associated with a subclinical SCN5A mutation[J]. Circulation, 2002, 106(10): 1269-1274. DOI:10.1161/01.cir.0000027139.42087.b6 |
| [23] |
VAN NOORD C, EIJGELSHEIM M, STRICKER B H. Drug-and non-drug-associated QT interval prolongation[J]. Br J Clin Pharmacol, 2010, 70(1): 16-23. DOI:10.1111/j.1365-2125.2010.03660.x |
| [24] |
VORPERIAN V R, HAVIGHURST T C, MILLER S, et al. Adverse effects of low dose amiodarone: a meta-analysis[J]. J Am Coll Cardiol, 1997, 30(3): 791-798. DOI:10.1016/s0735-1097(97)00220-9 |
| [25] |
SCOTT R B, CHRISTOPHER M C, PETER A N, et al. QTc prolongation, torsades de pointes, and psychotropic medications[J]. Psychosomatics, 2013, 54(1): 1-13. DOI:10.1016/j.psym.2012.11.001 |
| [26] |
DREW B J, CALIFF R M, FUNK M, et al. Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses[J]. Circulation, 2004, 110(17): 2721-2746. DOI:10.1161/01.CIR.0000145144.56673.59 |
| [27] |
MOLOKHIA M, PATHAK A, LAPEYRE-MESTRE M, et al. Case ascertainment and estimated incidence of drug-induced long-QT syndrome: study in Southwest France[J]. Br J Clin Pharmacol, 2008, 66(3): 386-395. DOI:10.1111/j.1365-2125.2008.03229.x |
| [28] |
SHAH R R. Drugs, QTc interval prolongation and final ICH E14 guideline: an important milestone with challenges ahead[J]. Drug Saf, 2005, 28(11): 1009-1028. DOI:10.2165/00002018-200528110-00003 |
| [29] |
JIMÉNEZ-CANDIL J, GONZÁLEZ I C, GONZÁLEZ MATAS J M, et al. Short-and long-term prognostic value of the corrected QT interval in the non-ST-elevation acute coronary syndrome[J]. J Electrocardiol, 2007, 40(2): 180-187. DOI:10.1016/j.jelectrocard.2006.10.006 |
| [30] |
ZIPES D P, RUBART M. Neural modulation of cardiac arrhythmias and sudden cardiac death[J]. Heart Rhythm, 2006, 3(1): 108-113. DOI:10.1016/j.hrthm.2005.09.021 |
| [31] |
LEHMANN M H, MORADY F. QT interval: metric for cardiac prognosis?[J]. Am J Med, 2003, 115(9): 732-734. DOI:10.1016/j.amjmed.2003.10.008 |
| [32] |
PANOULAS V F, TOMS T E, DOUGLAS K M, et al. Prolonged QTc interval predicts all-cause mortality in patients with rheumatoid arthritis: an association driven by high inflammatory burden[J]. Rheumatology, 2014, 53(1): 131-137. DOI:10.1093/rheumatology/ket338 |
| [33] |
STÖLLBERGER C, GERGER D, WEGNER C, et al. Quantitative electrocardiographic measures, neuromuscular disorders, and survival in left ventricular hypertrabeculation/noncompaction[J]. Ann Noninvasive Electrocardiol, 2013, 18(3): 251-255. DOI:10.1111/anec.12053 |
| [34] |
VEGLIO M, CHINAGLIA A, CAVALLO-PERIN P. QT interval, cardiovascular risk factors and risk of death in diabetes[J]. J Endocrinol Invest, 2004, 27(2): 175-181. DOI:10.1007/BF03346265 |
| [35] |
DREW B J, ACKERMAN M J, FUNK M, et al. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation[J]. Circulation, 2010, 121(8): 1047-1060. DOI:10.1161/CIRCULATIONAHA.109.192704 |
| [36] |
TISDALE J E, WROBLEWSKI H A, OVERHOLSER B R, et al. Prevalence of QT interval prolongation in patients admitted to cardiac care units and frequency of subsequent administration of QT interval-prolonging drugs: a prospective, observational study in a large urban academic medical center in the US[J]. Drug Saf, 2012, 35(6): 459-470. DOI:10.2165/11598160-000000000-00000 |
| [37] |
MAHMUD R, GRAY A, NABEEBACCUS A, et al. Incidence and outcomes of long QTc in acute medical admissions[J]. Int J Clin Pract, 2018, 72(11): e13250. DOI:10.1111/ijcp.13250 |
| [38] |
SALEM M, REICHLIN T, FASEL D, et al. Torsade de pointes and systemic azole antifungal agents: analysis of global spontaneous safety reports[J]. Glob Cardiol Sci Pract, 2017, 2017(2): 11. DOI:10.21542/gcsp.2017.11 |
| [39] |
心电图危急值2017中国专家共识——中国心电学会危急值专家工作组[J]. 临床心电学杂志, 2017, 26(6): 401-402.
|
| [40] |
LOPEZ-MEDINA A I, CHAHAL C A A, LUZUM J A. The genetics of drug-induced QT prolongation: evaluating the evidence for pharmacodynamic variants[J]. Pharmacogenomics, 2022, 23(9): 543-557. DOI:10.2217/pgs-2022-0027 |
 2024, Vol. 45
2024, Vol. 45

