2. 解放军陆军第八十三集团军医院骨科, 新乡 453004
2. Department of Orthopaedics, No. 83 Army Group Hospital, Xinxiang 453004, Henan, China
慢性腰痛是现代社会最常见的肌肉骨骼问题,是患者生活质量低、经济负担重的原因之一[1]。通常认为慢性腰痛的病因是生物、心理和社会因素等相互作用的结果[2]。虽然生物、心理和社会因素在预测腰痛复发和慢性发作方面有重要作用,但脊柱形态和姿势因素也可能影响腰痛的发生。多项研究表明,正常的脊柱-骨盆矢状面参数对正常人群保持平衡姿势至关重要[3-5]。然而,关于脊柱-骨盆矢状面参数对慢性腰痛的影响仍不明确。既往研究多集中在椎间盘退变性腰痛患者的矢状面参数特征分析,且样本量偏小[6-7]。为了更好地了解慢性腰痛患者脊柱-骨盆矢状面参数的特征,本研究对比分析一组慢性腰痛患者与无症状成人脊柱-骨盆矢状面参数的差异,现将有关情况报告如下。
1 资料和方法 1.1 研究对象回顾性分析2019年7月至2021年6月在海军军医大学(第二军医大学)第一附属医院门诊就诊的435例慢性腰痛患者(腰痛组)资料。纳入标准:(1)年龄>18岁;(2)至少连续3个月症状以腰痛为主;(3)有完整站立位全脊柱正侧位X线片资料。排除标准:(1)脊柱畸形如脊柱侧凸或滑脱;(2)脊柱骨折;(3)脊柱肿瘤;(4)既往脊柱融合手术;(5)既往椎间盘切除术累及1个及以上节段;(6)髋关节或骨盆疾病史;(7)X线摄片禁忌证(如妊娠、肿瘤);(8)明显的腿痛;(9)存在运动系统缺陷。
选取同时间段内在海军军医大学(第二军医大学)第一附属医院体检的146名无腰痛症状成人作为对照组。纳入标准:(1)年龄>18岁;(2)经骨科医师评估确认无脊柱疾病;(3)无脊柱、髋关节、盆腔疾病史;(4)无X线摄片禁忌证(如妊娠、肿瘤);(5)有完整站立位全脊柱正侧位X线片资料。本研究经海军军医大学(第二军医大学)第一附属医院伦理委员会审批。
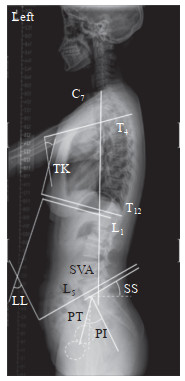
1.2 数据采集收集两组人群的年龄、性别、BMI等一般资料。用Surgmap软件在全脊柱正侧位X线片上测量脊柱-骨盆矢状面参数(图 1),包括胸椎后凸角(thoracic kyphosis,TK;T4椎体上终板延长线与T12椎体下终板延长线之间的夹角)[8]、腰椎前凸角(lumbar lordosis,LL;L1椎体上终板延长线与L5椎体下终板延长线之间的夹角)、骶骨倾斜角(sacral slope,SS;水平线与骶骨终板切线之间的夹角)、骨盆倾斜角(pelvic tilt,PT;股骨头中心连线中点和骶骨终板中点的连线与铅垂线之间的夹角)、骨盆入射角(pelvic incidence,PI;股骨头中心连线中点和骶骨终板中点的连线与骶骨终板垂线之间的夹角)、矢状面躯干偏移(sagittal vertical axis,SVA;C7椎体中点铅垂线与S1椎体后上角的水平距离)[9]。根据Roussouly等[5]的分类方法将腰椎前凸分为4型。1型:SS<35°,LL较腰椎前凸顶点位于L5中点,下腰弯角度很小,趋于水平;2型:SS<35°,LL较小,腰椎前凸顶点位于L4,下腰弯趋于水平,胸弯及腰弯均偏小;3型:SS为35°~45°,PI相对较大,腰椎前凸顶点在L4,平均有4个椎体构成腰椎前凸;4型:SS>45°,腰椎前凸顶点在L3或更高位椎体,胸弯偏大。
|
图 1 脊柱-骨盆矢状面参数测量方法示意图 Fig 1 Schematic diagram of measurement methods of sagittal spino-pelvic parameters |
1.3 统计学处理
采用SPSS 22.0软件进行数据分析。服从正态分布的计量资料采用x±s表示,组间比较采用独立样本t检验。计数资料以例数(百分数)表示,组间比较采用χ2检验。检验水准(α)为0.05。
2 结果 2.1 一般资料腰痛组患者249例,男97例、女152例,平均年龄(40.66±11.40)岁,BMI(23.59±1.54)kg/m2。对照组86例,男40例、女46例,平均年龄(41.78±12.81)岁,BMI(23.72±1.23)kg/m2。两组研究对象的年龄、性别、BMI差异均无统计学意义(P均>0.05)。
2.2 两组脊柱-骨盆矢状面参数的比较腰痛组TK大于对照组,而LL-TK、SS、PI和SS-PT均小于对照组,差异均有统计学意义(P均<0.05)。两组间LL、PT、LL-PI和SVA差异均无统计学意义(P均>0.05)。见表 1。
|
|
表 1 两组脊柱-骨盆矢状面参数的比较 Tab 1 Comparison of spino-pelvic sagittal parameters between 2 groups |
2.3 两组腰椎前凸类型的比较
腰痛组与对照组的腰椎前凸类型均以2型为主[70.7%(176/249)vs 57.0%(49/86)],其次是3型[27.3%(68/249)vs 38.4%(33/86)],而1型、4型腰椎前凸占比均较低,分别为1.2%(3/249)和2.3%(2/86)、0.8%(2/249)和2.3%(2/86),两组的腰椎前凸类型构成比差异无统计学意义(χ2=6.161,P=0.104)。
3 讨论已有研究者对脊柱-骨盆矢状面参数在发育性脊柱滑脱[7, 10-11]、退变性脊柱滑脱[12]、青少年特发性脊柱侧凸[13-15]和成人脊柱畸形[16-17]等脊柱疾病中的作用进行了研究,还有研究评估了慢性腰痛与腰椎间盘疾病的脊柱-骨盆参数[6-7, 18-19]。During等[6]评估了20例L5~S1椎间盘退变患者和24例无影像学异常的腰痛患者的腰椎-骨盆矢状面参数,结果只在L5~S1椎间盘退变的患者中观察到异常的腰骶关节角。Rajnics等[7]也观察到50例慢性腰痛和椎间盘突出症患者与30名健康者在SS、PT、LL方面差异有统计学意义,但PI、TK差异没有统计学意义。然而矢状面参数与慢性腰痛之间的关系目前仍不清楚。
在慢性腰痛患者中,骨盆形态(PI)和骨盆方向(PT和SS)参数与LL之间存在很强的相关性,这些相关性也存在于正常个体中[20]。既往研究发现,慢性腰痛患者SS减小、PT增大、LL减小[18-19, 21]。Barrey等[19]认为,LL的丧失不仅是继发于椎间盘退变的结构性病变,也是体位性病变,以减少椎间盘负荷相关的疼痛。Rajnics等[18]认为,更小的SS、更大的PT和更小的LL导致更大的压应力,使椎间盘发生退变。本研究发现,腰痛组的SS小于对照组,但两组间PT、LL差异没有统计学意义。有趣的是,本研究中腰痛组与对照组之间所有参数的平均差异都很小,这可能是不同研究之间得出的结论存在差异甚至是冲突的原因,与选择的研究对象有关。即使在无腰痛症状的对照组中,脊柱-骨盆矢状面参数也是高度可变的。因此,虽然差异存在统计学意义,但仍认为慢性腰痛患者的脊柱-骨盆矢状面参数与正常人的差异很小,在临床上除了脊柱-骨盆序列外还有多种因素会导致腰椎退变。在骨盆形态方面,腰痛组的平均PI为(44.67±8.84)°,与其他研究报道[6, 18-19]相似。与之前的3项研究[6, 18-19]不同的是,腰痛组与对照组之间PI差异有统计学意义,尽管平均差异只有2.43°,可能与纳入研究的受试者人数较多有关。
有研究发现腰痛患者腰椎前凸的类型与正常人群不同。Jackson和McManus[21]观察到腰痛患者远端节段LL较小,近端节段LL较大。相反,Gautier等[22]报道腰椎前凸类型(通过近端LL与远端LL评估)与腰痛的发生没有相关性。事实上,仅通过区分近端和远端LL来描述腰椎前凸的类型可能过于简单,无法完全代表常见的腰椎前凸类型,尤其是在没有考虑骨盆几何形状影响的情况下。从这个意义上说,Roussouly等[5]提出的分类方法更有可能涵盖所有类型的腰椎前凸。Roussouly等[5]认为1型腰椎前凸是正常成年人中最不常见的腰椎前凸类型。本研究结果也佐证了该分类的可行性,腰痛组患者2型腰椎前凸的占比最高(70.7%),这一发现证实了更大比例的慢性腰痛患者倾向于表现出较小的SS(<35°)与长而小的LL(平背)。PI是一个形态参数(与体位无关),与腰椎前凸的类型有关,PI异常小的患者发生腰痛的风险可能增加,因为腰椎前凸导致的椎间盘压力增加和/或维持适当平衡所需的肌肉生物力学欠佳。正如Barrey等[19]报道结果,在腰痛患者中2型腰椎前凸患者的比例更大可能是继发于先前存在的椎间盘退变或体位适应,以减少椎间盘负荷带来的疼痛。这些假设尚需未来对腰椎前凸的类型作进一步研究证实。
腰痛患者的骨盆、腰椎和胸椎参数与对照组之间差异存在统计学意义,腰椎前凸的类型分布在两组间也有不同。与无腰痛症状成人相比,腰痛患者站立位SS异常小(<35°)伴随较长但较小LL所占比例较高。以上这些发现可能有助于根据脊柱-骨盆矢状面参数特征识别容易发生腰痛的受试者。未来应前瞻性评估年轻无症状受试者,以确定脊柱-骨盆矢状面特定参数是否可以预测慢性腰痛的发展。对于具有特定矢状面参数的受试者,是否可以制定特定的措施来预防腰痛的发生尚不清楚,旨在改变腰痛患者脊柱-骨盆矢状面参数的特定康复方案也需进一步研究。
| [1] |
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of disease study 2016[J]. Lancet, 2017, 390: 1211-1259. DOI:10.1016/S0140-6736(17)32154-2 |
| [2] |
KNEZEVIC N N, CANDIDO K D, VLAEYEN J W S, VAN ZUNDERT J, COHEN S P. Low back pain[J]. Lancet, 2021, 398: 78-92. DOI:10.1016/S0140-6736(21)00733-9 |
| [3] |
JANSSEN M M, DREVELLE X, HUMBERT L, SKALLI W, CASTELEIN R M. Differences in male and female spino-pelvic alignment in asymptomatic young adults: a three-dimensional analysis using upright low-dose digital biplanar X-rays[J/OL]. Spine (Phila Pa 1976), 2009, 34: E826-E832. DOI: 10.1097/BRS.0b013e3181a9fd85.
|
| [4] |
MAC-THIONG J M, LABELLE H, BERTHONNAUD E, BETZ R R, ROUSSOULY P. Sagittal spinopelvic balance in normal children and adolescents[J]. Eur Spine J, 2007, 16: 227-234. DOI:10.1007/s00586-005-0013-8 |
| [5] |
ROUSSOULY P, GOLLOGLY S, BERTHONNAUD E, DIMNET J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position[J]. Spine (Phila Pa 1976), 2005, 30: 346-353. DOI:10.1097/01.brs.0000152379.54463.65 |
| [6] |
DURING J, GOUDFROOIJ H, KEESSEN W, BEEKER T W, CROWE A. Toward standards for posture. Postural characteristics of the lower back system in normal and pathologic conditions[J]. Spine (Phila Pa 1976), 1985, 10: 83-87. DOI:10.1097/00007632-198501000-00013 |
| [7] |
RAJNICS P, TEMPLIER A, SKALLI W, LAVASTE F, ILLÉS T. The association of sagittal spinal and pelvic parameters in asymptomatic persons and patients with isthmic spondylolisthesis[J]. J Spinal Disord Tech, 2002, 15: 24-30. DOI:10.1097/00024720-200202000-00004 |
| [8] |
ZHOU S, XU F, WANG W, ZOU D, SUN Z, LI W. Age-based normal sagittal alignment in Chinese asymptomatic adults: establishment of the relationships between pelvic incidence and other parameters[J]. Eur Spine J, 2020, 29: 396-404. DOI:10.1007/s00586-019-06178-9 |
| [9] |
CHA E, PARK J H. Spinopelvic alignment as a risk factor for poor balance function in low back pain patients[J/OL]. Global Spine J, 2022: 21925682221076417. DOI: 10.1177/21925682221076417.
|
| [10] |
MAC-THIONG J M, WANG Z, DE GUISE J A, LABELLE H. Postural model of sagittal spino-pelvic alignment and its relevance for lumbosacral developmental spondylolisthesis[J]. Spine (Phila Pa 1976), 2008, 33: 2316-2325. DOI:10.1097/BRS.0b013e318186b236 |
| [11] |
MACIEJCZAK A, JABŁOŃSKA-SUDOŁ K. Correlation between correction of pelvic balance and clinical outcomes in mid- and low-grade adult isthmic spondylolisthesis[J]. Eur Spine J, 2017, 26: 3112-3121. DOI:10.1007/s00586-016-4808-6 |
| [12] |
KARIM S M, FISHER C, GLENNIE A, RAMPERSAUD R, STREET J, DVORAK M, et al. Preoperative patient-reported outcomes are not associated with sagittal and spinopelvic alignment in degenerative lumbar spondylolisthesis[J]. Spine (Phila Pa 1976), 2022, 47: 1128-1136. DOI:10.1097/BRS.0000000000004374 |
| [13] |
SCHLÖSSER T P C, CASTELEIN R M, GROBOST P, SHAH S A, ABELIN-GENEVOIS K. Specific sagittal alignment patterns are already present in mild adolescent idiopathic scoliosis[J]. Eur Spine J, 2021, 30: 1881-1887. DOI:10.1007/s00586-021-06772-w |
| [14] |
BURTON D A, KARKENNY A J, SCHULZ J F, HANSTEIN R, GOMEZ J A. Sagittal spinopelvic changes after posterior spinal fusion in adolescent idiopathic scoliosis[J]. J Child Orthop, 2020, 14: 544-553. DOI:10.1302/1863-2548.14.200155 |
| [15] |
张毅, 邵杰, 李唯, 李雄飞, 白玉树. 青少年特发性脊柱侧凸患者术后脊柱骨盆矢状面参数的变化[J]. 海军军医大学学报, 2022, 43: 533-539. ZHANG Y, SHAO J, LI W, LI X F, BAI Y S. Changes of sagittal spino-pelvic parameters after surgery in adolescent idiopathic scoliosis patients[J]. Acad J Naval Med Univ, 2022, 43: 533-539. |
| [16] |
ROSE P S, BRIDWELL K H, LENKE L G, CRONEN G A, MULCONREY D S, BUCHOWSKI J M, et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy[J]. Spine (Phila Pa 1976), 2009, 34: 785-791. DOI:10.1097/BRS.0b013e31819d0c86 |
| [17] |
NOLTE M T, LOUIE P K, HARADA G K, KHAN J M, FERGUSON J, DEWALD C J, et al. Sagittal balance in adult idiopathic scoliosis[J]. Clin Spine Surg, 2020, 33: 53-61. DOI:10.1097/BSD.0000000000000940 |
| [18] |
RAJNICS P, TEMPLIER A, SKALLI W, LAVASTE F, ILLES T. The importance of spinopelvic parameters in patients with lumbar disc lesions[J]. Int Orthop, 2002, 26: 104-108. DOI:10.1007/s00264-001-0317-1 |
| [19] |
BARREY C, JUND J, NOSEDA O, ROUSSOULY P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases[J]. Eur Spine J, 2007, 16: 1459-1467. DOI:10.1007/s00586-006-0294-6 |
| [20] |
WANG Q, SUN C T. Characteristics and correlation analysis of spino-pelvic sagittal parameters in elderly patients with lumbar degenerative disease[J/OL]. J Orthop Surg Res, 2019, 14: 127. DOI: 10.1186/s13018-019-1156-3.
|
| [21] |
JACKSON R P, MCMANUS A C. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study[J]. Spine (Phila Pa 1976), 1994, 19: 1611-1618. DOI:10.1097/00007632-199407001-00010 |
| [22] |
GAUTIER J, MORILLON P, MARCELLI C. Does spinal morphology influence the occurrence of low back pain? A retrospective clinical, anthropometric, and radiological study[J]. Rev Rhum Engl Ed, 1999, 66: 29-34. |
 2023, Vol. 44
2023, Vol. 44


