2. 海军军医大学(第二军医大学)第二附属医院脊柱外科, 上海 200003
2. Spine Center, Department of Orthopaedics, The Second Affiliated Hospital of Naval Medical University (Second Military Medical University), Shanghai 200003, China
随着我国人均寿命的延长和生活、工作方式的改变, 越来越多的人出现颈肩部酸痛、上肢麻木、无力、放射性疼痛等不适, 这些症状与椎间孔处神经根和神经节受压有很大关系, 目前以神经根型及其为主的混合型颈椎病在颈椎病中最多见(占60%~70%), 而神经根型颈椎病中以C5/C6节段最为多见[1-2]。目前对神经根型颈椎病的研究多集中于椎间盘、骨赘等外来致压物方面, 而对于颈椎间孔本身的研究则少见。
基于多层螺旋CT产生的数字骨科学对骨组织成像效果较好, 同时对软组织有一定的显像效果, 是目前研究颈椎间孔的重要影像学手段[2-3]。本课题组前期完成了华东地区健康成人颈椎间孔影像学参数的测量[4], 在此基础上制定了椎间孔各相关径值单侧正常参考值95%的区间范围。本研究通过测量伴C5/C6椎间孔狭窄神经根型颈椎病的影像学参数, 探讨颈椎间孔形态、狭窄程度的临床意义, 尝试提出颈椎间孔绝对、相对狭窄及颈椎间孔狭窄症的影像学诊断标准, 为神经根型颈椎病的手术减压范围和程度提供依据。
1 资料和方法 1.1 研究对象通过预试验结果确定样本量后, 以简单随机化方法选取2014年9月至2019年7月在海军军医大学(第二军医大学)第二附属医院因伴C5/C6椎间孔狭窄神经根型颈椎病住院手术治疗的患者492例作为病例组, 男246例、女246例。纳入标准: (1)有颈肩部酸胀、疼痛等不适感或上肢根性疼痛、上肢或手麻木等症状; (2)年龄为18~60岁, 体型发育正常; (3)颈肩部活动度受限, 可有压痛、叩击痛、压颈试验阳性, 臂丛牵拉试验阳性, 上肢酸胀、疼痛、麻木, 四肢肌力可减退、肌张力可增强, 四肢骨膜反射、腱反射正常或亢进, 四肢温触觉、痛觉等浅感觉可减退, 霍夫曼征、巴宾斯基征等病理征阴性; (4)颈椎MRI检查示C5/C6椎间孔、神经根管狭窄, 神经根受压; (5)将检查的辐射影响等告知患者, 其充分知晓并接受相关检查。病例组患者中, 将狭窄或严重狭窄一侧的C5/C6椎间孔确定为观察侧椎间孔, 另一侧则为对侧椎间孔。
正常成人组为前期研究[4]选择的191名来院体检的健康成年人(共382个C5/C6椎间孔)。
1.2 颈椎椎间孔形态及影像学参数测量 1.2.1 颈椎正侧位X线片采用荷兰飞利浦KB 500 mA X线机, 拍摄时以C4椎体为中心线, 拍正位片时使正中矢状面平行于台面, 拍侧位片时使同一椎体上下终板重叠。
1.2.2 MRI检查采用荷兰飞利浦1.5 T MRI扫描仪, 颈椎扫描采用颈椎线圈, 扫描序列有T1加权水平面序列、T1加权冠状面序列、T2加权冠状面序列、T2压脂相冠状面序列和T2压脂相水平面序列, 层距为4 mm, 层厚为4 mm。常规设置层距、矩阵及层厚等参数后, 全部给予次成像采集, 自旋回波序列T1加权成像参数: 重复时间为450 ms, 回波时间为10~20 ms; 快速自旋回波序列T1加权成像参数: 重复时间为3 000 ms, 回波时间为110 ms。
1.2.3 CT检查采用荷兰飞利浦64排双源CT机, 扫描范围为枕骨粗隆至T1椎体下缘。扫描参数: 电压为120 kV, 电流为500 mA; 扫描速度为0.42 s/圈, 螺距为0.9∶1.0, 层厚为3.0 mm, 采集方式为64层/圈, 重组间隔为1.0 mm, 以标准算法重组; 扫描时间为8~14 s, 重建层厚为1.0 mm。用SuperImageTM Orthopedics Edition数字骨科系统对CT图像进行重建, 包括冠状面、矢状面、水平面和任意角度斜位图像。
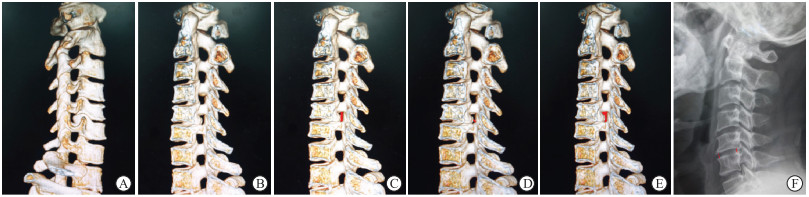
1.2.4 影像学参数测量利用CT三维重建图像和X线片, 由3位熟练的专业医师在相同窗宽、窗位、放大率及相同的最佳投射角度下, 分别观察双侧椎间孔形态并测量相关参数, 如果数据差异较大则采用格拉布斯准则判断, 将可疑值从此组测量数据中剔除, 不参与统计。(1)椎间孔形态: 分别从椎管外(图 1A)及椎管内(图 1B)观测最佳投射角度下各椎间孔的形态。(2)纵径: 椎间孔下位椎弓根上缘内侧中点至上位椎弓根下缘外侧中点的距离(图 1C)。(3)横径均值: 测量上前后径和下前后径并计算平均值, 其中上前后径为C6上关节突前上缘至C5椎体后下缘的间距(图 1D), 下前后径为C5下关节突前下缘至C6椎体后上缘的间距。(4)横截面积: 最佳投射角度下椎间孔横截面的面积(图 1E)。(5)椎间隙平均高度: 测量同一椎体上下终板重叠时椎间隙前后的高度并计算平均值(图 1F)。
|
图 1 C5/C6椎间孔的CT三维重建图像及参数测量 Fig 1 C5/C6 intervertebral foramen in CT 3-dimensional reconstruction images and measurement of related parameters A: Morphology of intervertebral foramen observed outside spinal canal; B: Morphology of intervertebral foramen observed in spinal canal; C: Longitudinal diameter of intervertebral foramen (red line); D: Upper anteroposterior diameter of intervertebral foramen (red line); E: Sagittal cross-sectional area of intervertebral foramen (red zone); F: Intervertebral disc height (red lines). CT: Computed tomography. |
1.3 统计学处理
应用SPSS 22.0软件对所测参数进行统计学分析。计量资料以x±s表示, 正常成人组和病例组之间C5/C6椎间孔各径值的比较采用单因素方差分析, 病例组双侧C5/C6椎间孔各径值的比较采用配对t检验, 不同性别之间各径值的比较采用独立样本t检验。计数资料以频数和百分数表示, 组间比较采用χ2检验或Fisher确切概率法。检验水准(α)为0.05。
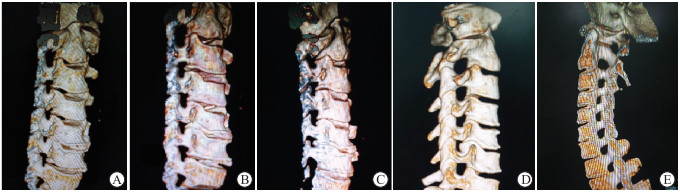
2 结果 2.1 观察侧C5/C6椎间孔形态变化情况综合颈椎MRI、数字骨科系统及术中探查结果, 病例组观察侧C5/C6椎间孔形态较正常成人组明显改变(图 2), 在492个观察侧C5/C6椎间孔中, 导致椎间孔狭窄的致压物以骨性致压物为主的椎间孔为422个(85.77%), 以非骨性致压物为主的椎间孔为70个(14.23%); 50.61%(249/492)的椎间孔呈纺锤形改变, 29.27%(144/492)的椎间孔呈不规则形改变, 呈类圆形、类椭圆形、类长方形、马蹄形的椎间孔分别占2.24%(11/492)、2.64%(13/492)、5.08%(25/492)、10.16%(50/492)。男女患者观察侧椎间孔形态分布差异无统计学意义(P>0.05, 表 1)。
|
图 2 C5/C6椎间孔形态 Fig 2 Morphology of C5/C6 intervertebral foramen A-D: Case group. A: Horseshoe-shaped; B: Spindle-shaped; C: Irregular; D: Rectangle-like. E: Normal adult group. |
|
|
表 1 伴C5/C6椎间孔狭窄神经根型颈椎病的男女患者的C5/C6椎间孔形态分布 Tab 1 Morphology distribution of C5/C6 intervertebral foramen in male and female patients with cervical spondylotic radiculopathy with C5/C6 intervertebral foramen stenosis |
2.2 C5/C6椎间孔各径值测量结果
病例组观察侧C5/C6椎间孔横径均值、纵径、横截面积、椎间隙平均高度分别为(5.81±1.40)mm、(10.45±1.70)mm、(50.02±15.46)mm2、(4.99±0.89)mm。191名健康成年人双侧C5/C6椎间孔(n=382)对应的各径值分别为(7.60±1.37)mm、(11.66±1.95)mm、(72.80±22.48)mm2、(5.78±0.95)mm。病例组观察侧椎间孔各径值均小于正常成人组, 差异均有统计学意义(P<0.05)。病例组观察侧椎间孔与对侧椎间孔之间及病例组男女患者之间各径值比较差异均无统计学意义(P>0.05)。见表 2。
|
|
表 2 病例组和正常成人组C5/C6椎间孔各径值测量结果 Tab 2 C5/C6 intervertebral foramen diameter in case group and normal adult group |
2.3 各径值对骨性颈椎间孔狭窄的诊断价值
以正常成人C5/C6椎间孔径值单侧95%下限为临界值, 纵径≤8.50 mm的C5/C6椎间孔中有33个致压物以骨性组织为主, 纵径>8.50 mm的椎间孔中有40个致压物以非骨性组织为主; 横径均值≤5.34 mm且致压物以骨性组织为主的椎间孔有363个, 横径均值>5.34 mm且致压物为非骨性组织的椎间孔有53个; 横截面积≤48.65 mm2且致压物以骨性组织为主的椎间孔有249个, 横截面积>48.65 mm2且致压物为非骨性组织的椎间孔有45个; 椎间隙平均高度≤4.20 mm且椎间孔中以骨性致压物为主的椎间孔有57个, 椎间隙平均高度>4.20 mm且致压物为非骨性致压物的椎间孔有29个; 横径均值≤5.34 mm且横截面积≤48.65 mm2的椎间孔有249个, 而纵径≤8.50 mm且横截面积≤48.65 mm2的椎间孔有31个, 椎间隙平均高度≤4.20 mm且横截面积≤48.65 mm2的椎间孔有55个。
C5/C6椎间孔横径均值诊断骨性颈椎间孔狭窄的灵敏度为86.02%, 特异度为70.71%;C5/C6椎间孔的纵径诊断骨性颈椎间孔狭窄的灵敏度为7.82%, 特异度为57.14%;C5/C6椎间孔横截面积诊断骨性颈椎间孔狭窄的灵敏度为59.00%, 特异度为64.29%;C5/C6椎间隙平均高度诊断骨性颈椎间孔狭窄的灵敏度为13.51%, 特异度为41.43%。综上可见, C5/C6椎间孔的横径均值在诊断骨性颈椎间孔狭窄导致的神经根型颈椎病灵敏度和特异度较高。
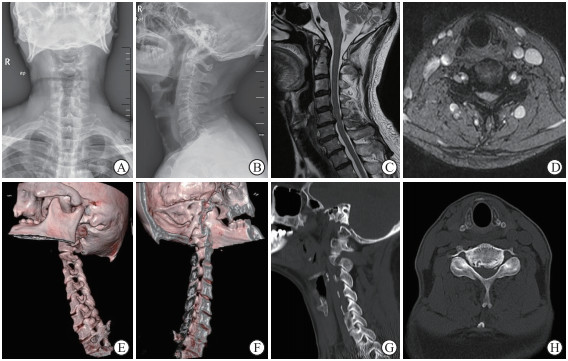
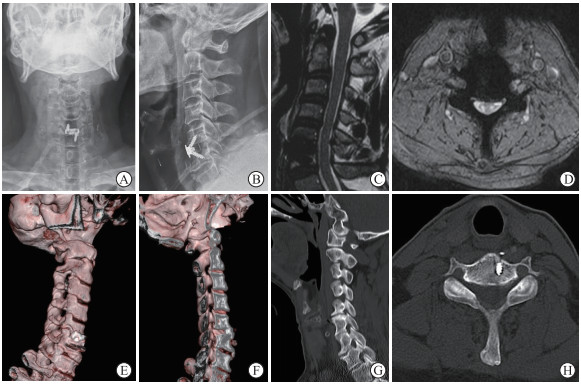
2.4 典型病例患者男, 69岁, 左侧肩部疼痛伴左上臂外侧疼痛、麻木2年, 加重2个月入院。术前检查提示C5/C6双侧椎间孔狭窄, 以左侧C5/C6椎间孔为甚, 左侧C5/C6椎间隙平均高度为5.8 mm, 左侧C5/C6椎间孔的纵径为8.03 mm, 左侧C5/C6椎间孔的横径均值为1.98 mm, 左侧C5/C6椎间孔横截面积为15.89 mm2(图 3)。结合X线片、CT、MRI检查结果, 判断致压物以骨性为主, 术中充分行C5/C6双侧椎间孔减压, 验证致压物为骨性, 行高度为8 mm的Zero-P VA撑开固定。术后复查X线片、CT、MRI见致压物明显切除, 左侧C5/C6椎间隙平均高度为7.94 mm, 左侧C5/C6椎间孔纵径为9.89 mm, 左侧C5/C6椎间孔横径均值为5.65 mm, 左侧C5/C6椎间孔横截面积为52.15 mm2(图 4), 患者症状明显缓解。
|
图 3 典型病例的术前影像学资料 Fig 3 Preoperative imaging data of a typical case Male, 69 years old, cervical spondylotic radiculopathy with C5/C6 intervertebral foramen stenosis. A: X-ray positive film; B: Lateral X-ray film showing narrowing of C5/C6 intervertebral space; C: Sagittal MRI showing nerve compression; D: C5/C6 cross-sectional MRI showing bilateral nerve compression; E: CT 3-dimensional reconstruction showing severe intervertebral foramen stenosis outside the spinal canal; F: CT 3-dimensional reconstruction of severe intraspinal intervertebral foramen stenosis; G: CT 2-dimensional reconstruction showing bony stenosis of intervertebral foramen of C5/C6; H: Cross-sectional CT showing bony stenosis of bilateral intervertebral foramen in C5/C6. MRI: Magnetic resonance imaging; CT: Computed tomography. |
|
图 4 典型病例的术后影像学资料 Fig 4 Postoperative imaging data of a typical case Male, 69 years old, cervical spondylotic radiculopathy with C5/C6 intervertebral foramen stenosis. A: X-ray positive film; B: Lateral X-ray film showed that the height of C5/C6 intervertebral space was increased; C: No compression was found in the sagittal position of MRI; D: The cross-sectional MRI of C5/C6 showed that there was no compression of bilateral nerves; E: CT 3-dimensional reconstruction showed that the intervertebral foramen was enlarged outside the spinal canal; F: CT 3-dimensional reconstruction showed that the intervertebral foramen was enlarged; G: CT 2-dimensional reconstruction showed that the intervertebral foramen of C5/C6 was enlarged compared with that before operation; H: Cross-sectional CT showed that the bony compression of the bilateral intervertebral foramen of C5/C6 was decompressed completely. MRI: Magnetic resonance imaging; CT: Computed tomography. |
3 讨论
本研究对492例C5/C6椎间孔狭窄致神经根型颈椎病患者的影像学参数测量结果显示, 狭窄C5/C6椎间孔的形态以纺锤形为主, 共249个, 占50.61%;第二常见的椎间孔形态是不规则形, 共144个, 占29.27%。而正常成人组中C5/C6椎间孔的形态以类椭圆形为主, 占59.69%, 纺锤形占17.28%[4]。病例组狭窄椎间孔形态改变最主要的原因是椎间孔入口处骨赘增生, 且以下节段椎体后上缘骨赘增生为主, 骨赘的形态以单峰型、双峰型、鸟嘴样、平峰样为主。同时组成椎间孔后壁的关节突肥大、增生、不稳及黄韧带肥厚、增生等也是椎间孔形态改变的主要原因之一, 椎间孔前壁骨赘增生及后壁关节突肥大、增生等导致颈椎间孔形态呈中央狭窄的纺锤形改变[1, 3]。研究表明, 颈椎间盘突出、关节突关节失稳等因素是导致该节段骨赘增生较其他节段明显且为双侧椎间孔同时发生的主要原因[5]。部分X线片及CT检查未见椎间孔狭窄, 但术中探查见椎间孔存在狭窄, 这可能与X线片、CT无法对椎间孔周围的软组织有效显影有关, 所以临床需要采用能够清晰显示软组织的MRI来完善检查[6-7]。
C5/C6椎间孔狭窄神经根型颈椎病患者的颈椎间孔纵径较正常成人减小(P<0.05), 且男女患者之间椎间孔纵径差异无统计学意义(P>0.05)。椎间孔纵径减小是随着椎间盘退变导致椎间隙高度减低而出现的; 同时颈椎退变导致椎间孔周围软组织及骨性结构改变, 继而导致椎间孔纵径和椎间孔横截面积变小。椎间孔纵径≤8.50 mm的C5/C6椎间孔中有33个致压物为骨性组织, 颈椎间孔纵径诊断骨性颈椎间孔狭窄的灵敏度为7.82%, 特异度为57.14%。Wu等[8]研究表明, 屈曲位同时上肢外展时神经根经过椎间孔处的张力明显减小, 这是因为在屈曲位时颈椎间孔的纵径较中立位明显增加, 使椎间孔横截面积增大, 减轻了神经根压力。Liu等[9]研究表明, 以5、10、15 kg牵引颈椎时, 颈椎间孔纵径分别增加了3.75%、8.67%和10.43%, 以5、10 kg牵引时纵径与中立位未牵引时的纵径相比差异有统计学意义, 而与10、15 kg牵引时纵径的变化差异无统计学意义。这为枕颌带牵引缓解神经根型颈椎病的症状提供了临床依据, 临床上多行屈曲位颈椎牵引, 屈曲位牵引可以扩大椎间孔纵径、增大椎间孔纵径及横截面积, 部分缓解了神经根受压导致的症状。但并非牵引重量越大椎间孔纵径变化越大, 牵引负荷过大可能导致前、后纵韧带与椎间盘及关节突关节等损伤, 引起颈椎不稳, 出现更加严重的症状[10-11]。
C5/C6椎间孔狭窄神经根型颈椎病患者的颈椎间孔横径均值较正常成人减小(P<0.05), 男女患者之间差异无统计学意义(P>0.05)。以正常成人单侧95%下限为临界值, 颈椎间孔中致压物为骨性组织且横径均值≤5.34 mm的椎间孔有363个, 横径均值诊断颈椎间孔狭窄的灵敏度和特异度分别为86.02%、70.71%。研究表明椎间孔横径的变化与颈椎间孔狭窄的相关性更强[2, 12], 这与临床表现一致, 临床上椎间孔前壁骨赘增生及椎体后壁关节突肥厚、增生、失稳等导致颈椎间孔横径均值减小, 或伸展、侧弯、旋转等情况下椎间孔横径均值明显减小导致神经根经过椎间孔处的张力明显增加, 均可诱发甚至使颈肩部酸胀、疼痛、麻木、活动受限等症状加重, 这也是Spurling试验的理论依据[13]。
C5/C6椎间孔狭窄神经根型颈椎病患者椎间孔横截面积较正常成人减小(P<0.05), 男女患者之间椎间孔横截面积差异无统计学意义(P>0.05)。以正常成人单侧95%下限为临界值, 横截面积诊断颈椎间孔狭窄的灵敏度和特异度分别为59.00%、64.29%。颈椎间孔的横截面积与椎间孔的形态、纵径、横径、椎间隙高度等多种因素相关, 同时运动状态下颈椎间孔相关径值的改变也会导致颈椎间孔横截面积发生改变[3, 11]。本研究结果显示横径均值≤5.34 mm且横截面积≤48.65 mm2的C5/C6椎间孔有249个, 而纵径≤8.50 mm且横截面积≤48.65 mm2的C5/C6椎间孔有31个, 椎间隙平均高度≤4.20 mm且横截面积≤48.65 mm2的C5/C6椎间孔有55个。因此, 颈椎间孔的横径均值与横截面积相关性更强, 同时椎间孔其他径值及椎间隙高度也是影响椎间孔横截面积的重要因素。余情和李泽兵[14]研究显示, 侧弯侧椎间孔横截面积随着侧弯角度增大而减小, 侧弯对侧椎间孔横截面积则随着侧弯角度增大而增大。研究表明, 在全屈曲位时C3/C4、C4/C5、C5/C6椎间孔横截面积分别增加了16%、22.6%、13.3%, 且屈曲位角度越大椎间孔横截面积变化越大; 而在全伸展位时, C3/C4、C4/C5、C5/C6椎间孔横截面积分别减小了21%、15%、10%, 同样椎间孔的横截面积随着伸展角度的增加而减小, 其值与全屈曲位相比差异有统计学意义[6, 15]。多项研究表明, 在旋转位时旋转侧椎间孔横截面积随旋转角度增加不断减小, 而旋转对侧椎间孔横截面积变化则相反[16-17]。研究表明, 以5、10、15 kg牵引颈椎时, 相应的颈椎间孔纵径分别增加了3.75%、8.67%和10.43%[9], 而椎间孔横截面积分别增加了5.81%、16.56%和18.9%[18]。
C5/C6椎间孔狭窄神经根型颈椎病患者的椎间隙平均高度较正常成人减小; 以正常成人单侧95%下限为临界值, 椎间隙平均高度≤4.20 mm且致压物为骨化物的颈椎间孔有57个, 椎间隙平均高度诊断骨性颈椎间孔狭窄的灵敏度和特异度分别为13.51%、41.43%。随着颈椎退变及颈部韧带松弛, 椎间盘髓核逐渐脱水、颈椎间盘体积变小, 同时关节突关节韧带退变导致椎间盘前后高度丢失, 使颈椎间孔纵径、横径、横截面积减小, 引起神经根受压逐渐加重而出现更加严重的颈肩部酸痛、上肢麻木、无力、放射性疼痛等不适等[12, 19-20]。研究表明, 椎间隙高度丢失1 mm时椎间孔横截面积减小20%~30%, 当椎间隙高度丢失2 mm时椎间盘横截面积丢失达到30%~40%, 而当椎间隙高度丢失3 mm时椎间孔横截面积只有原来的55%~65%[21], 因此术中不仅要注意椎间孔横径的充分、有效扩大, 同时也应适当地撑高椎间隙, 扩大椎间孔面积, 为神经根提供更加宽阔的骨性通道, 减少术后神经根再受压的可能。
椎间孔横径均值诊断神经根型颈椎病的灵敏度和特异度较高, 我们提出C5/C6椎间孔横径均值≤5.34 mm应考虑骨性C5/C6椎间孔狭窄。颈椎间孔横径减小主要由钩椎关节增生和后纵韧带肥厚、增生、骨化等导致, 术中减压时应更注意颈椎间孔入口处的处理和椎间孔横径的有效扩大, 同时不能忽略椎间孔前后壁及内外侧软组织的处理, 且术中应适当撑高椎间隙及增加椎间孔横截面积等, 以提高手术效果, 更好地改善患者预后。本研究仅选取单中心行颈前路手术的492例伴C5/C6椎间孔狭窄神经根型颈椎病患者, 样本量较小, 尚需多中心、大样本的研究进一步证实结果。
| [1] |
OSHINA M, TANI S, YAMADA T, et al. Limitations of minimally invasive posterior cervical foraminotomy—a decompression method of posteriorly shifting the nerve root—in cases of large anterior osteophytes in cervical radiculopathy: a retrospective multicenter cohort study[J]. J Orthop Sci, 2023, 28(4): 758-764. DOI:10.1016/j.jos.2022.06.011 |
| [2] |
HIRAI S, KATO S, NAKAJIMA K, et al. Anatomical study of cervical intervertebral foramen in patients with cervical spondylotic radiculopathy[J]. J Orthop Sci, 2021, 26(1): 86-91. DOI:10.1016/j.jos.2020.01.017 |
| [3] |
PARK M S, MOON S H, KIM T H, et al. Surgical anatomy of the uncinate process and transverse foramen determined by computed tomography[J]. Global Spine J, 2015, 5(5): 383-390. DOI:10.1055/s-0035-1550091 |
| [4] |
谢栋, 许晨辉, 叶程, 等. 华东地区健康成人颈椎椎间孔影像学参数测量[J]. 脊柱外科杂志, 2021, 19(3): 177-181. DOI:10.3969/j.issn.1672-2957.2021.03.007 |
| [5] |
CLIFTON W, VALERO-MORENO F, VLASAK A, et al. Microanatomical considerations for safe uncinate removal during anterior cervical discectomy and fusion: 10-year experience[J]. Clin Anat, 2020, 33(6): 920-926. DOI:10.1002/ca.23596 |
| [6] |
KAYA O, SARIYILMAZ K, TUTPINAR Y, et al. Evaluation of dynamic foraminal stenosis with positional MRI in patients with C6 radiculopathy-mimicking pain: a prospective radiologic cohort study[J]. Biomed Res Int, 2022, 2022: 1385387. DOI:10.1155/2022/1385387 |
| [7] |
陈标, 周永, 狄星伯. C5/C6颈椎间盘突出症患者颈髓受压程度与颈椎MRI测量值相关性分析[J]. 中国CT和MRI杂志, 2021, 19(4): 147-149. DOI:10.3969/j.issn.1672-5131.2021.04.045 |
| [8] |
WU S K, CHEN H Y, YOU J Y, et al. Outcomes of active cervical therapeutic exercise on dynamic intervertebral foramen changes in neck pain patients with disc herniation[J]. BMC Musculoskelet Disord, 2022, 23(1): 728. DOI:10.1186/s12891-022-05670-6 |
| [9] |
LIU J, EBRAHEIM N A, SANFORD C G Jr, et al. Quantitative changes in the cervical neural foramen resulting from axial traction: in vivo imaging study[J]. Spine J, 2008, 8(4): 619-623. DOI:10.1016/j.spinee.2007.04.016 |
| [10] |
YE L Q, CHEN C, LIU Y H, et al. Effect of cervical spine motion on displacement of posterolateral annulus fibrosus in cervical spondylotic radiculopathy with contained posterolateral disc herniation: a three-dimensional finite element analysis[J]. J Orthop Surg Res, 2022, 17(1): 548. DOI:10.1186/s13018-022-03450-5 |
| [11] |
CHANG V, BASHEER A, BAUMER T, et al. Dynamic measurements of cervical neural foramina during neck movements in asymptomatic young volunteers[J]. Surg Radiol Anat, 2017, 39(10): 1069-1078. DOI:10.1007/s00276-017-1847-6 |
| [12] |
SUN B, XU C, QI M, et al. Predictive effect of intervertebral foramen width on pain relief after ACDF for the treatment of cervical radiculopathy[J]. Global Spine J, 2023, 13(1): 133-139. DOI:10.1177/2192568221993444 |
| [13] |
DERNEK B, AYDOǦMUŞ S, DUYMUŞ T M, et al. The incidence of impingement syndrome in cases of cervical radiculopathy: an analysis of 220 cases[J]. J BackMusculoskelet Rehabil, 2020, 33(3): 363-366. DOI:10.3233/BMR-181354 |
| [14] |
余情, 李泽兵. 颈椎旋转对颈椎间孔形态的影响[J]. 中华物理医学与康复杂志, 2003, 25(12): 719-722. DOI:10.3760/j:issn:0254-1424.2003.12.005 |
| [15] |
张正丰, 梅芳瑞, 周军海. 下颈椎屈伸运动对椎间孔面积影响的实验研究[J]. 中国脊柱脊髓杂志, 1998, 8(5): 259-262. DOI:10.3969/j.issn.1004-406X.1998.05.006 |
| [16] |
DUGAILLY P M, BEYER B, SALEM W, et al. Morphometric changes of the cervical intervertebral foramen: a comparative analysis of pre-manipulative positioning and physiological axial rotation[J]. Musculoskelet Sci Pract, 2018, 34: 97-102. DOI:10.1016/j.msksp.2018.01.007 |
| [17] |
YOSHIOKA N, TAKAYAMA M, KOBAYASHI T, et al. Neurological disturbance of the upper extremities after cervical laminoplasty: a morphological assessment focused on the intervertebral foramen[J]. Spine, 2020, 45(23): E1549-E1555. DOI:10.1097/BRS.0000000000003671 |
| [18] |
KNAPIK D M, ABOLA M V, GORDON Z L, et al. Differences in cross-sectional intervertebral foraminal area from C3 to C7[J]. Global Spine J, 2018, 8(6): 600-606. DOI:10.1177/2192568218758085 |
| [19] |
YANG R, MA M, HUANG L, et al. Influences of different lower cervical bone graft heights on the size of the intervertebral foramen: multiple planar dynamic measurements with laser scanning[J]. Lasers Med Sci, 2018, 33(3): 627-635. DOI:10.1007/s10103-018-2452-6 |
| [20] |
AHMED S H, EL-SHAARAWY E A A, ISHAQ M F, et al. Morphological and radiometrical study of the human intervertebral foramina of the cervical spine[J]. Folia Morphol, 2014, 73(1): 7-18. DOI:10.5603/FM.2014.0002 |
| [21] |
LU J, EBRAHEIM N A, HUNTOON M, et al. Cervical intervertebral disc space narrowing and size of intervertebral foramina[J]. Clin Orthop Relat Res, 2000(370): 259-264. DOI:10.1097/00003086-200001000-00026 |
 2023, Vol. 44
2023, Vol. 44


