梗阻性左半结肠癌的外科治疗策略目前仍存在争议,其焦点主要在于如何减少吻合口瘘的发生及提高患者的生活质量和远期生存率[1]。内镜技术的发展为梗阻性左半结肠癌的治疗带来了理念转变和技术革新,通过术前经肛放置肠梗阻导管或留置自膨式金属支架减压过渡可实现较为可靠的一期肿瘤切除和肠吻合,特别是在不完全性梗阻的情况下具有显著的优势[2]。然而,内镜治疗本身也存在一定的局限性,针对不具备内镜处置条件或内镜治疗失败的梗阻性左半结肠癌患者,本团队探索并实践了一种吻合口旁分流式造口手术方式,在实现急诊一期肿瘤切除和结肠吻合的同时,有效降低了吻合口瘘的发生风险,且二期造口关闭术简便易行,取得了较为理想的临床疗效,现报告如下。
1 资料和方法 1.1 病例来源纳入我院2019年7月至2022年1月不具备内镜处置条件或内镜治疗失败的梗阻性左半结肠癌患者共5例。5例患者均进行一期肿瘤切除肠吻合+吻合口旁分流式造口术及二期造口关闭术。
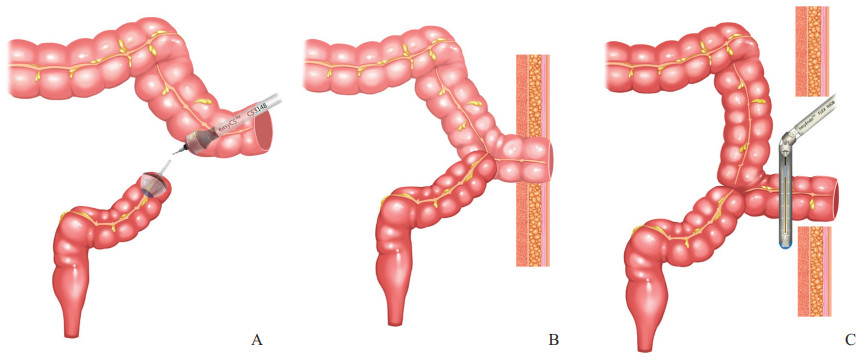
1.2 治疗方法(1)一期手术:首先行剖腹探查术,以确认肿瘤局部可切除。常规完成左半结肠切断后移除切除的肠段,于远端肠管开口置入适宜大小的管状吻合器钉座并荷包缝合固定;将近端结肠拖出腹腔外接减压盆,经端口向近端肠管插入胃肠减压器,通过手法挤压辅助,尽可能吸除肠腔内积蓄的粪水和气体,并用温热生理盐水反复灌洗肠腔至灌洗液清亮;经近端结肠端口插入吻合器(深6~10 cm),经系膜缘侧肠壁穿出,与远端结肠开口行端侧吻合(图 1A)。最后,选择腹壁合适的位置,经原手术切口或另取切口将近端结肠开口引出腹腔,做经腹壁单腔肠造口(图 1B)。术中注意保持吻合口无成角、无扭曲、无张力。(2)二期造口关闭术:术后4~8周关闭造口。分离造口肠管与腹壁之间的粘连至腹壁腱膜层,采用直线切割闭合器切除造口段结肠,缝合关闭造口,然后逐层缝合腹壁腱膜和皮肤(图 1C)。
|
图 1 吻合口旁分流式造口术及二期造口关闭术示意图 A:采用管状吻合器完成远端结肠端口与近端结肠侧壁吻合;B:将近端结肠开口引出腹腔做经腹壁单腔肠造口;C:采用直线切割闭合器离断造口段结肠并完成造口关闭. |
2 结果
5例患者中男3例、女2例,年龄为37~71岁,平均年龄为56.4岁;肿瘤位于结肠脾曲3例、降结肠中段1例、乙状结肠1例;完全性肠梗阻2例、不完全性肠梗阻3例。5例患者均于我科成功施行急诊手术治疗,其中腹腔镜辅助手术4例、直接开放手术1例。出现肠梗阻症状至手术的时间为3~12 d。5例患者行一期肿瘤切除肠吻合+吻合口旁分流式造口术后均无吻合口瘘、腹腔感染及造口相关并发症,均顺利出院,平均住院时间为8.0(6~11)d。
二期造口关闭术与一期肿瘤切除肠吻合+吻合口旁分流式造口术间隔33~59 d,平均间隔时间为46.2 d。1例患者二期造口关闭术在静脉麻醉下实施,3例在硬膜外麻醉下实施,1例在局部麻醉下实施,5例二期手术均成功,平均手术时间为30.4(26.0~35.0)min。5例患者二期造口关闭术后均无肠瘘、切口感染等并发症。
3 讨论我国结肠癌的发病率和死亡率一直呈上升趋势,其中8%~29%的患者以急性肠梗阻为首发表现,且以左半结肠癌导致的闭襻性梗阻多见[3]。梗阻性左半结肠癌的处理一直是困扰外科医师的一大难题,也是该领域学术争议的焦点[4]。梗阻性左半结肠癌常见的手术方式包括:(1)一期单纯结肠造口术,二期肿瘤切除肠吻合术,三期造口关闭术[5];(2)一期肿瘤切除+近端结肠造口术,二期消化道重建术,即Hartmann术式[6];(3)一期结肠次全切除+肠吻合术[7];(4)一期肿瘤切除+结肠吻合+吻合口近端结肠或末端回肠保护性造口术,二期造口关闭术[8];(5)术前内镜下解除梗阻后限期一期肿瘤切除+结肠吻合术[9]。上述术式各有优缺点,具体方案的选择除受患者病情影响外,更受手术医师技术操作、经验、习惯及担当意识的影响[10]。
随着外科理念的发展和技术的进步,梗阻性左半结肠癌一期完成肿瘤切除+结肠吻合不再是外科禁忌[11]。一期急诊肿瘤切除+肠吻合术为一期肿瘤切除+结肠吻合术后加行近端结肠或末段回肠保护性造口术[8],其缺点主要在于这2种传统保护性造口的还纳手术相对繁杂,并发症发生率高,且受腹腔粘连的制约明显[12]。同时,末端回肠造口由于不在肿瘤切除手术的操作区域,需另取腹壁切口,进一步增加了手术创伤和腹腔感染的风险。
随着内镜技术和器械的不断进步,通过内镜下置放自膨式金属支架缓解梗阻症状再限期完成肿瘤切除的治疗策略取得了良好的近期和远期疗效[13],成为胃肠肿瘤外科临床研究的前沿热点,但该方法存在诸多局限性。(1)内镜操作本身存在一定的外科风险,支架对肿瘤的机械性挤压可能导致局部出血及肠穿孔,且存在促进肿瘤播散转移的可能[14]。研究报道,梗阻性左半结肠癌患者内镜下置放自膨式金属支架治疗后,其远期生存率显著低于急诊手术患者[15]。(2)支架存在滑脱、移位的可能,减压效果不确切。(3)结肠支架置放成功与否受患者病情和内镜操作者经验的影响,在梗阻肠腔闭塞严重的情况下存在支架置放失败的可能,不仅延误了治疗,还会进一步增加肠梗阻的严重程度。研究表明,支架置放失败的梗阻性结直肠癌患者总体预后劣于直接行急诊手术的患者[16]。
本团队急诊处置梗阻性左半结肠癌时,探索并实践了一种吻合口旁分流式造口的手术方式。本术式的主要优点如下:(1)梗阻远、近端肠管无论口径相差多少都可以吻合。(2)从源头上能有效预防吻合口瘘的发生。肠管水肿严重者,使用可吸收缝线加固缝合更加可靠。(3)术后短期内即可以关闭造口,且操作简单、方便,不存在二期不能回纳的问题。(4)选择经腹腔镜辅助小切口造口可以简化手术操作、减轻手术创伤,对病情危重、全身状况差的患者更具优势。本术式的临床适应证为梗阻性左半结肠癌,肿瘤位置包括但不限于结肠脾曲、降结肠及乙状结肠上段,特别是为不具备内镜处置条件、内镜治疗失败或不愿意接受内镜治疗的梗阻性左半结肠癌患者提供了一种一期术后保护性造口方式。对于肿瘤位于乙状结肠以下者,由于吻合口位置低,难以在腹壁完成近端造口,故不推荐这一术式。
本团队采用的这种吻合口旁分流式造口手术方式是对Santulli肠吻合造瘘术适应证的拓展。Santulli肠吻合造瘘术最早于1961年由Santulli和Blanc[17]提出并用于小儿先天性小肠闭锁的外科治疗,随后许多外科医师尝试将其应用于早期高位小肠瘘[18]、新生儿肠梗阻[19]及全结肠神经发育异常[20]患儿的治疗,并取得较为理想的临床效果。本组5例梗阻性左半结肠癌在急诊一期完成肿瘤切除肠吻合恢复肠道连续性的同时,通过吻合口旁分流式造口有效降低了吻合口处的肠腔内压力,取得了与传统末端回肠或近端结肠造口相近的保护性效果。此外,本术式可以较传统的保护性造瘘术更早进行回纳,减少了长时间造口给患者带来的不便。更为重要的,在造口关闭时无须进行广泛的肠管游离,且可在神经阻滞麻醉或局部麻醉下进行,操作简单、创伤小,无二期手术吻合口瘘的发生风险,值得在临床上推广应用。
| [1] |
VELD J V, AMELUNG F J, BORSTLAP W A A, VAN HALSEMA E E, CONSTEN E C J, SIERSEMA P D, et al. Changes in management of left-sided obstructive colon cancer: national practice and guideline implementation[J]. J Natl Compr Cancer Netw, 2019, 17: 1512-1520. DOI:10.6004/jnccn.2019.7326 |
| [2] |
VELD J V, AMELUNG F J, BORSTLAP W A A, VAN HALSEMA E E, CONSTEN E C J, SIERSEMA P D, et al. Comparison of decompressing stoma vs stent as a bridge to surgery for left-sided obstructive colon cancer[J]. JAMA Surg, 2020, 155: 206-215. DOI:10.1001/jamasurg.2019.5466 |
| [3] |
BRAY F, FERLAY J, SOERJOMATARAM I, SIEGEL R L, TORRE L A, JEMAL A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA a Cancer J Clin, 2018, 68: 394-424. DOI:10.3322/caac.21492 |
| [4] |
NEO V S Q, JAIN S R, YEO J W, NG C H, GAN T R X, TAN E, et al. Controversies of colonic stenting in obstructive left colorectal cancer: a critical analysis with meta-analysis and meta-regression[J]. Int J Colorectal Dis, 2021, 36: 689-700. DOI:10.1007/s00384-021-03834-9 |
| [5] |
ZHOU H Y, WANG A Q, BIAN C, ZHANG J. Stoma-resection-reversal strategy for left-sided obstructive colon cancer—a video vignette[J]. Colorectal Dis, 2021, 23: 3052-3053. DOI:10.1111/codi.15898 |
| [6] |
DURÁN GIMÉNEZ-RICO H, ABRIL VEGA C, HERREROS RODRÍGUEZ J, CONCEJO CÚTOLI P, PASEIRO CRESPO G, SABATER MAROTO C, et al. Hartmann's procedure for obstructive carcinoma of the left colon and rectum: a comparative study with one-stage surgery[J]. Clin Transl Oncol, 2005, 7: 306-313. DOI:10.1007/BF02710270 |
| [7] |
HUGHES E S R, CUTHBERTSON A M. Subtotal colectomy for obstructing carcinoma of the upper left colon[J]. Dis Colon Rectum, 1965, 8: 411-412. DOI:10.1007/BF02617478 |
| [8] |
肖博凯, 曾玉剑, 施承民, 孙亮, 舒若, 张同, 等. 预防性末端回肠造瘘在梗阻性左半结肠癌患者期吻合中的应用[J]. 中华胃肠外科杂志, 2017, 20: 335-337. |
| [9] |
AREZZO A, PASSERA R, LO SECCO G, VERRA M, BONINO M A, TARGARONA E, et al. Stent as bridge to surgery for left-sided malignant colonic obstruction reduces adverse events and stoma rate compared with emergency surgery: results of a systematic review and meta-analysis of randomized controlled trials[J]. Gastrointest Endosc, 2017, 86: 416-426. DOI:10.1016/j.gie.2017.03.1542 |
| [10] |
VELD J V, AMELUNG F J, BORSTLAP W A A, VAN HALSEMA E E, CONSTEN E C J, DEKKER J W T, et al. Decompressing stoma as bridge to elective surgery is an effective strategy for left-sided obstructive colon cancer: a national, propensity-score matched study[J]. Ann Surg, 2020, 272: 738-743. DOI:10.1097/SLA.0000000000004173 |
| [11] |
AWOTAR G K, GUAN G X, SUN W, YU H L, ZHU M, CUI X Y, et al. Reviewing the management of obstructive left colon cancer: assessing the feasibility of the one-stage resection and anastomosis after intraoperative colonic irrigation[J/OL]. Clin Colorectal Cancer, 2017, 16: e89-e103. DOI: 10.1016/j.clcc.2016.12.001.
|
| [12] |
OURÔ S, FERREIRA M P, ALBERGARIA D, MAIO R. Loop ileostomy in rectal cancer surgery: factors predicting reversal and stoma related morbidity[J]. Langenbeck's Arch Surg, 2021, 406: 843-853. DOI:10.1007/s00423-021-02169-x |
| [13] |
MORA-LÓPEZ L, HIDALGO M, FALCÓ J, SERRA-PLA S, PALLISERA-LLOVERAS A, GARCIA-NALDA A, et al. Long-term outcomes of colonic stent as a "bridge to surgery" for left-sided malignant large-bowel obstruction[J]. Surg Oncol, 2020, 35: 399-405. DOI:10.1016/j.suronc.2020.09.025 |
| [14] |
AMELUNG F J, BURGHGRAEF T A, TANIS P J, VAN HOOFT J E, TER BORG F, SIERSEMA P D, et al. Critical appraisal of oncological safety of stent as bridge to surgery in left-sided obstructing colon cancer; a systematic review and meta-analysis[J]. Crit Rev Oncol, 2018, 131: 66-75. DOI:10.1016/j.critrevonc.2018.08.003 |
| [15] |
KATSUKI R, JO T, YASUNAGA H, ISHIMARU M, SAKAMOTO T. Outcomes of self-expandable metal stent as bridge to surgery versus emergency surgery for left-sided obstructing colon cancer: a retrospective cohort study[J]. Am J Surg, 2021, 221: 168-173. DOI:10.1016/j.amjsurg.2020.06.012 |
| [16] |
LIM T Z, CHAN D, TAN K K. Patients who failed endoscopic stenting for left-sided malignant colorectal obstruction suffered the worst outcomes[J]. Int J Colorectal Dis, 2014, 29: 1267-1273. DOI:10.1007/s00384-014-1948-1 |
| [17] |
SANTULLI T V, BLANC W A. Congenital atresia of the intestine: pathogenesis and treatment[J]. Ann Surg, 1961, 154: 939-948. |
| [18] |
郭斌. Santulli肠造瘘术用于早期高位小肠瘘患儿中的安全性及可行性[J]. 当代医学, 2015, 21: 54-55. |
| [19] |
岳铭, 翟子绮, 王冠涛, 张宁, 杨合英. Santulli肠吻合造瘘术在新生儿肠梗阻中的应用[J]. 郑州大学学报(医学版), 2020, 55: 572-576. |
| [20] |
李世宪, 张宏伟, 刘丰丽, 殷易钰, 马同胜, 张腾飞, 等. Santulli肠造瘘术治疗全结肠神经发育异常患儿的疗效[J]. 江苏医药, 2021, 47: 373-376. |
 2022, Vol. 43
2022, Vol. 43


