2. 北京中医药大学东直门医院超声科,北京 100010
2. Department of Ultrasound, Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing 100010, China
流行病学调查发现,冠状动脉粥样硬化性心脏病(以下简称冠心病)的死亡率位列心脏病死亡率的首位,是心血管疾病导致死亡的最主要类型[1]。心绞痛是冠心病最常见的临床表现之一,分为稳定型、不稳定型和变异型3种类型。心绞痛多是由于冠状动脉斑块破裂、出血甚至脱落导致动脉管腔狭窄闭塞、心肌缺血缺氧引起的一种病症,若治疗不及时,易引发心肌梗死,甚至死亡。研究显示,冠心病患者颈动脉硬化可发生在疾病早期,对患者行颈动脉超声检查可以达到筛查冠状动脉硬化的目的[2]。动脉弹性是心脑血管疾病的重要标志物及独立危险因素[3]。动脉弹性主要反映动脉舒张功能,它取决于动脉腔径大小和管壁厚度或可扩张性。脉搏波传导速度(pulse wave velocity,PWV)可间接反映动脉血管弹性,其作为动脉管壁弹性检测的无创性新方法,与心血管疾病死亡密切相关[4]。既往研究发现,心绞痛可能与系统性动脉硬化呈正相关,臂踝PWV适用于筛查劳力性心绞痛[5]。目前针对稳定型及不稳定型冠心病心绞痛患者的颈动脉PWV研究鲜见报道。极速脉搏波传导速度(ultrafast pulse wave velocity,UFPWV)利用组织多普勒成像技术,以超过2 000帧/秒的速度采集图像,能够准确检测颈动脉PWV,并具有较好的可重复性[6]。本研究选取2020年6月至2021年6月黑龙江中医药大学附属第一医院收治的冠心病心绞痛患者64例为研究对象,探讨UFPWV技术在冠心病心绞痛患者颈动脉粥样硬化风险评估中的应用价值。
1 资料和方法 1.1 研究对象前瞻性选取2020年6月至2021年6月黑龙江中医药大学附属第一医院收治的冠心病心绞痛患者64例,按照心绞痛的类型分为稳定组(稳定型心绞痛,34例)和不稳定组(不稳定型心绞痛,30例)。因未检索到相关研究数据,故按照一般经验,n≥30才能满足模型估计的基本要求,因此本研究选取的最小样本量为30例。纳入标准:(1)经临床诊断符合冠心病稳定型心绞痛和不稳定型心绞痛诊断标准[7-10];(2)无急性心肌梗死病史;(3)年龄<80岁;(4)沟通能力正常,自愿参与并配合本研究。排除标准:(1)肝肾功能明显异常(如存在肝硬化、肝性脑病、腹水、肾功能衰竭等);(2)近半年内发生过脑梗死;(3)合并心肌炎、扩张型心肌病等;(4)机体凝血功能明显异常(凝血酶原时间>12 s);(5)合并感染性疾病;(6)超声图像不清晰;(7)临床资料不完整。选取同期健康志愿者30名作为健康对照组。本研究经黑龙江中医药大学附属第一医院伦理委员会审批,所有研究对象均签署了知情同意书。
1.2 常规二维颈动脉超声检查和PWV检测应用具有PWV模式的法国声科SuperSonic Airplorer超声诊断仪进行颈动脉常规超声和PWV检测,探头型号为SL10-2,频率6~9 MHz。常规超声及PWV检测均由2名副主任医师操作完成。颈动脉常规超声检查:叮嘱受检者头部放松,取仰卧位,颈部略转向被检查侧的对侧。动态扫查颈总动脉起始段和中段、颈动脉球部、颈内和颈外动脉起始段至远端,检测并记录颈总动脉远心段及颈总动脉球部后壁内中膜厚度(intima-media thickness,IMT)。颈动脉内中膜广泛性增厚,内中膜融合,肌层低回声暗带消失,以1.0 mm≤IMT<1.5 mm判断内膜增厚[11]。如有斑块,尽量避开斑块,测量斑块的肩部远心端。
PWV检测:将探头置于颈总动脉长轴最大切面,清晰显示颈总动脉内中膜,尽量保持探头与血管壁平行,调节增益,避开斑块处。待图像稳定后启动PWV键,图像采集需2 s,在此过程中探头保持稳定,不可晃动加压,直到图像处理完成。将取样线尽量调至与血管壁重合,按下select键,检测颈总动脉收缩期开始时脉搏波传导速度(pulse wave velocity in beginning of systole,PWV-BS)和颈总动脉收缩期结束时脉搏波传导速度(pulse wave velocity in ending of systole,PWV-ES),以标准差Δ不超过PWV-BS、PWV-ES的20%视为数值有效。重复3次测量取平均数。
1.3 超声心动图检查采用日本东芝Aplio900彩色多普勒超声诊断仪,探头频率3.4 MHz,收集受检者的左心室射血分数。受检者于检查前休息5 min,用双平面辛普森法获取数值。
1.4 斑块稳定性指标检测采集受检者空腹肘静脉血5 mL,采用ELISA检测斑块稳定性指标血清基质金属蛋白酶3(matrix metalloproteinase 3,MMP-3)、蛋白酶K水平。
1.5 统计学处理应用SPSS 26.0软件进行统计学分析。符合正态分布及方差齐的计量资料以x±s表示,多组间比较采用单因素方差分析,两组间比较采用独立样本t检验;计数资料以例数和百分数表示,组间比较采用χ2检验。检验水准(α)为0.05。
2 结果 2.1 一般资料比较稳定组34例患者中男21例、女13例,年龄40~73(53.80±6.71)岁;不稳定组30例患者中男20例、女10例,年龄42~74(54.20±6.52)岁;30例健康对照组中男19名、女11名,年龄41~72(54.10±7.26)岁。稳定组和不稳定组患者的BMI、收缩压、颈总动脉IMT及有吸烟史(吸烟≥1年)患者占比均高于健康对照组,差异均有统计学意义(P均<0.05)。稳定型组和不稳定型组患者的年龄、性别、吸烟史、BMI、收缩压、舒张压、左心室射血分数、颈总动脉IMT等一般资料差异均无统计学意义(P均>0.05)。见表 1。
|
|
表 1 各组一般资料比较 |
2.2 动脉硬化指标比较
如表 2所示,心绞痛患者的颈总动脉IMT、PWV-BS、PWV-ES均高于健康对照,差异均有统计学意义(P均<0.001)。
|
|
表 2 心绞痛患者和健康对照颈总动脉硬化指标比较 |
如表 3所示,不稳定组患者颈总动脉PWV-ES高于稳定组,差异有统计学意义(P<0.001);不稳定组患者颈总动脉PWV-BS、IMT与稳定组相比,差异均无统计学意义(P均>0.05)。
|
|
表 3 稳定型和不稳定型心绞痛患者的颈总动脉硬化指标比较 |
2.3 稳定组和不稳定组患者的斑块稳定性指标比较
不稳定组患者血清MMP-3水平[(145.28±15.36)ng/mL vs(97.61±9.08)ng/mL]、蛋白酶K水平[(25.09±2.82)pg/mL vs(15.85±1.76)pg/mL]均高于稳定组,差异均有统计学意义(P均<0.05)。
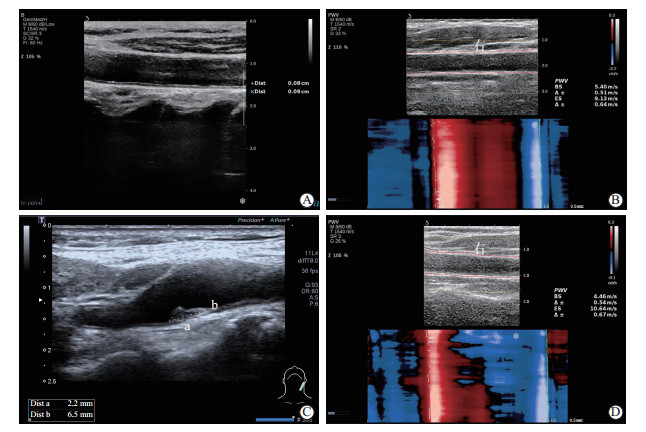
2.4 不同PWV-ES水平患者的斑块稳定性指标比较以PWV-ES中位数为分界值[12],PWV-ES高、低水平患者各32例。PWV-ES高水平患者的血清MMP-3水平[(151.96±17.48)ng/mL vs(88.93±8.52)ng/mL]和蛋白酶K水平[(27.15±3.12)pg/mL vs(14.06±1.78)pg/mL]均高于PWV-ES低水平患者,差异均有统计学意义(P均<0.01)。典型的冠心病心绞痛患者颈总动脉PWV检测图像见图 1。
|
图 1 冠心病心绞痛患者颈动脉UFPWV检测 A,B:稳定型心绞痛患者;C,D:不稳定型心绞痛患者.A:纵切面测量颈总动脉IMT;B:在颈总动脉体部测量PWV-BS、PWV-ES(PWV-BS=5.40 m/s,PWV-ES=9.13 m/s;标准差Δ分别小于PWV-BS、PWV-ES的20%,数值有效);C:颈总动脉球部后壁可见斑块;D:在颈总动脉体部测量PWV-BS、PWV-ES(PWV-BS=4.46 m/s,PWV-ES=10.64 m/s;标准差Δ分别小于PWV-BS、PWV-ES的20%,数值有效).UFPWV:极速脉搏波传导速度;IMT:内中膜厚度;PWV-BS:收缩期开始时脉搏波传导速度;PWV-ES:收缩期结束时脉搏波传导速度;Dist:距离. |
3 讨论
冠心病是常见的心血管系统疾病,心绞痛是冠心病最常见的临床表现之一,是主要不良心脑血管事件(major adverse cardiac and cerebrovascular event,MACCE)的预测因素。心绞痛会给患者带来较严重的心理困扰,使患者的生活质量下降、生存时间缩短[13]。近年冠心病心绞痛的患病率、死亡率呈逐年上升趋势且趋于年轻化,严重威胁着人类生命健康[14]。
冠心病心绞痛通常是由心肌缺血引起的症状,动脉粥样硬化增加了心外膜冠状动脉的阻力,当心外膜冠状动脉狭窄>70%时,即使在休息时也可能供血不足,导致缺血和心绞痛[4]。因此,预测冠状动脉的硬化程度对于冠心病及心绞痛的判断意义重大[15],对患者的治疗和预后有重大影响[16]。
冠状动脉造影是诊断冠心病、心绞痛及评估病情的金标准,但此类检查属于有创性检查,且需注射造影剂,因此临床应用有一定局限性。而冠心病患者颈动脉可存在与其冠状动脉相似的病理改变,可通过评价颈动脉的硬化间接评估冠状动脉的硬化程度[2]。颈动脉IMT和风险评分对冠状动脉病变具有较好的预测价值[17]。既往研究多采用颈动脉IMT作为超声评价早期动脉粥样硬化的标志物[18-20]。IMT是临床实践中早期评估血管硬化风险的一种常用、无创超声指标[16],但也有研究显示,在普通人群中,颈动脉IMT与心血管风险之间并无明确关系[21]。本研究结果显示,心绞痛患者的颈总动脉IMT高于健康对照组(P<0.001)。既往研究表明吸烟对冠状动脉的影响很大[22],本研究结果证实了这一结论,稳定型和不稳定型心绞痛患者中有吸烟史的患者比例高于健康对照组(P<0.05)。许多一级和二级预防试验表明,对可改变的危险因素(如戒烟)的管理,可以降低死亡率及心肌梗死、脑卒中和其他心血管事件的发生率[23-24]。由此可见,吸烟对心血管危害十分严重。但本研究中颈总动脉IMT、有吸烟史患者占比在稳定组与不稳定组之间的差异无统计学意义(P均>0.05)。
动脉弹性是心脑血管疾病早期的重要评估指标[3],但动脉弹性一般不易直接测得。而脉搏波是左心室收缩后主动脉瓣打开和心脏搏动沿动脉血管传播形成的,PWV能够反映血液的功能变化和容器壁的弹性与硬度[25-26]。以往检测血管弹性的技术有多层螺旋CT血管造影、速度向量成像技术,血管回声跟踪技术等。而颈-股动脉PWV和肱-踝动脉PWV是传统的PWV技术,使用这些方法获得的PWV值可能受到图像质量、测量距离、心率和计算方法的影响[27-29]。UFPWV技术无创、易操作、无辐射,能够超高速地自动抓拍,使用组织多普勒成像原理记录颈动脉壁的脉搏波,精准显示和测量颈动脉壁的运动过程[30]。在单次心动周期中测量径向速度,估测2个加速度峰值对应于2个传播波:收缩期开始时的第1波(主动脉瓣开放)测得速度即为PWV-BS,收缩期结束时第2个波(主动脉瓣关闭)测得速度即为PWV-ES[31]。动脉的扩张性越差、僵硬度越高、弹性越差,PWV-ES就越快,因此PWV作为评估动脉僵硬度的一个指标在临床中被广泛应用。临床诊断心绞痛多从症状考虑,以疼痛发作的时间和严重程度定诊。本研究中,心绞痛患者的颈总动脉PWV-BS、PWV-ES均高于健康对照(P均<0.001),不稳定组患者颈总动脉PWV-ES高于稳定组(P<0.001)。由此说明不稳定型心绞痛患者的冠状动脉硬化程度高于稳定型心绞痛患者,PWV-ES值更灵敏。
中心动脉僵硬度是心血管疾病的独立预测因素[32]。它的特点是动脉壁细胞外基质(extracellular matrix,ECM)的弹性蛋白/胶原蛋白含量比值显著降低,这主要是各种ECM成分降解的结果。MMP-3可能通过参与ECM稳态和重塑而导致中心动脉僵硬。血清MMP-3水平与中心动脉僵硬度之间关联的研究显示,MMP-3是颈-股动脉PWV的独立预测因子[33]。组织蛋白酶K是一种溶酶体半胱氨酸蛋白酶,可影响血管钙化。在慢性肾脏病患者中较高的蛋白酶K水平对其MACCE有影响。在非糖尿病慢性肾脏病患者中发现蛋白酶K水平、冠状动脉钙化和MACCE之间存在显著关联[34]。蛋白酶K不仅影响粥样斑块的ECM,也影响泡沫细胞的形成。蛋白酶K高表达在动脉粥样硬化的发生、发展中增加了动脉粥样硬化病变的易损性,促进其发生、发展[32, 35]。在血清斑块稳定性指标MMP-3和蛋白酶K水平比较方面,本研究得出PWV-ES高水平者的MMP-3和蛋白酶K高于PWV-ES低水平者(P均<0.01)。
综上所述,常规超声测量颈总动脉IMT用于心血管疾病危险分层存在争议,而检测PWV可以发现IMT尚未明显增厚的早期颈动脉硬化[36],为评价心绞痛患者的血管僵硬度提供了客观指标。这种新方法快速、方便、安全,能够定量反映动脉弹性的变化。由此可见,利用UFPWV技术测得的PWV-ES能够用来评估冠心病心绞痛患者的颈动脉粥样硬化风险,值得推广应用。
本研究存在一定的局限性,研究结果对结论的支持程度尚需深层次的论证:(1)本研究样本量较小,今后将开展大样本、多中心的研究;(2)尚需进一步随访不稳定型心绞痛与稳定型心绞痛患者的3年发病情况,以获得更可靠的证据。
| [1] |
PREJEAN S P, DIN M, REYES E, HAGE F G. Guidelines in review: comparison of the 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes and the 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation[J]. J Nucl Cardiol, 2018, 25: 769-776. DOI:10.1007/s12350-017-1137-z |
| [2] |
MALAKAR A K, CHOUDHURY D, HALDER B, PAUL P, UDDIN A, CHAKRABORTY S. A review on coronary artery disease, its risk factors, and therapeutics[J]. J Cell Physiol, 2019, 234: 16812-16823. DOI:10.1002/jcp.28350 |
| [3] |
VALLÉE A, ZHANG Y, PROTOGEROU A, SAFAR M E, BLACHER J. Added value of aortic pulse wave velocity index for the detection of coronary heart disease by elective coronary angiography[J]. Blood Press, 2019, 28: 375-384. DOI:10.1080/08037051.2019.1641400 |
| [4] |
BEN-SHLOMO Y, SPEARS M, BOUSTRED C, MAY M, ANDERSON S G, BENJAMIN E J, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17, 635 subjects[J]. J Am Coll Cardiol, 2014, 63: 636-646. DOI:10.1016/j.jacc.2013.09.063 |
| [5] |
YAMASA T, IKEDA S, KOGA S, KAWANO H, KAIBARA S, MAEMURA K. Comparison of the brachial-ankle pulse wave velocity between patients with acute coronary syndrome and effort angina pectoris[J]. Intern Med, 2018, 57: 1371-1374. DOI:10.2169/internalmedicine.9367-17 |
| [6] |
ZHU Z Q, CHEN L S, WANG H, LIU F M, LUAN Y, WU L L, et al. Carotid stiffness and atherosclerotic risk: non-invasive quantification with ultrafast ultrasound pulse wave velocity[J]. Eur Radiol, 2019, 29: 1507-1517. DOI:10.1007/s00330-018-5705-7 |
| [7] |
MEMBERS T F, MONTALESCOT G, SECHTEM U, ACHENBACH S, ANDREOTTI F, ARDEN C, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European Society of Cardiology[J]. Eur Heart J, 2013, 34: 2949-3003. DOI:10.1093/eurheartj/eht296 |
| [8] |
FIHN S D, GARDIN J M, ABRAMS J, BERRA K, BLANKENSHIP J C, DALLAS A P, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons[J]. Circulation, 2012, 126: 3097-3137. DOI:10.1161/CIR.0b013e3182776f83 |
| [9] |
HAGBERG S M, WOITALLA F, CRAWFORD P, American College of Cardiology, American Heart Association. 2002 ACC/AHA guideline versus clinician judgment as diagnostic tests for chest pain[J]. J Am Board Fam Med, 2008, 21: 101-107. DOI:10.3122/jabfm.2008.02.070146 |
| [10] |
BRAUNWALD E, ANTMAN E M, BEASLEY J W, CALIFF R M, CHEITLIN M D, HOCHMAN J S, et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction-summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina)[J]. J Am Coll Cardiol, 2002, 40: 1366-1374. DOI:10.1016/S0735-1097(02)02336-7 |
| [11] |
TOUBOUL P J, HENNERICI M G, MEAIRS S, ADAMS H, AMARENCO P, BORNSTEIN N, et al. Mannheim carotid intima-media thickness consensus (2004-2006). An update on behalf of the Advisory Board of the 3rd and 4th Watching the Risk Symposium, 13th and 15th European Stroke Conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006[J]. Cerebrovasc Dis, 2007, 23: 75-80. DOI:10.1159/000097034 |
| [12] |
YIN L X, MA C Y, WANG S, WANG Y H, MENG P P, PAN X F, et al. Reference values of carotid ultrafast pulse-wave velocity: a prospective, multicenter, population-based study[J]. J Am Soc Echocardiogr, 2021, 34: 629-641. DOI:10.1016/j.echo.2021.01.003 |
| [13] |
KLONER R A, CHAITMAN B. Angina and its management[J]. J Cardiovasc Pharmacol Ther, 2017, 22: 199-209. DOI:10.1177/1074248416679733 |
| [14] |
FERREIRA-GONZÁLEZ I. The epidemiology of coronary heart disease[J]. Rev Esp Cardiol (Engl Ed), 2014, 67: 139-144. DOI:10.1016/j.recesp.2013.10.003 |
| [15] |
VALLÉE A, PETRUESCU L, KRETZ S, SAFAR M E, BLACHER J. Added value of aortic pulse wave velocity index in a predictive diagnosis decision tree of coronary heart disease[J]. Am J Hypertens, 2019, 32: 375-383. DOI:10.1093/ajh/hpz004 |
| [16] |
LORENZ M W, MARKUS H S, BOTS M L, ROSVALL M, SITZER M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis[J]. Circulation, 2007, 115: 459-467. DOI:10.1161/CIRCULATIONAHA.106.628875 |
| [17] |
ZHU Y, YOU J, XU C, GU X. Predictive value of carotid artery ultrasonography for the risk of coronary artery disease[J]. J Clin Ultrasound, 2021, 49: 218-226. DOI:10.1002/jcu.22932 |
| [18] |
JEEVARETHINAM A, VENURAJU S, DUMO A, RUANO S, ROSENTHAL M, NAIR D, et al. Usefulness of carotid plaques as predictors of obstructive coronary artery disease and cardiovascular events in asymptomatic individuals with diabetes mellitus[J]. Am J Cardiol, 2018, 121: 910-916. DOI:10.1016/j.amjcard.2018.01.001 |
| [19] |
NEZU T, HOSOMI N, AOKI S, MATSUMOTO M. Carotid intima-media thickness for atherosclerosis[J]. J Atheroscler Thromb, 2016, 23: 18-31. DOI:10.5551/jat.31989 |
| [20] |
RAVANI A, WERBA J P, FRIGERIO B, SANSARO D, AMATO M, TREMOLI E, et al. Assessment and relevance of carotid intima-media thickness (C-IMT) in primary and secondary cardiovascular prevention[J]. Curr Pharm Des, 2015, 21: 1164-1171. DOI:10.2174/1381612820666141013121545 |
| [21] |
NAQVI T Z, LEE M S. Carotid intima-media thickness and plaque in cardiovascular risk assessment[J]. JACC Cardiovasc Imaging, 2014, 7: 1025-1038. DOI:10.1016/j.jcmg.2013.11.014 |
| [22] |
KONDO T, NAKANO Y, ADACHI S, MUROHARA T. Effects of tobacco smoking on cardiovascular disease[J]. Circ J, 2019, 83: 1980-1985. DOI:10.1253/circj.CJ-19-0323 |
| [23] |
KANTARIA M, BULEISHVILI M, KIPIANI N V, ORMOTSADZE G, SANIKIDZE T. Risk-factors of coronary artery disease (review)[J]. Georgian Med News, 2020(299): 78-82. |
| [24] |
BOUABDALLAOUI N, MESSAS N, GREENLAW N, FERRARI R, FORD I, FOX K M, et al. Impact of smoking on cardiovascular outcomes in patients with stable coronary artery disease[J]. Eur J Prev Cardiol, 2021, 28: 1460-1466. DOI:10.1177/2047487320918728 |
| [25] |
IKONOMIDIS I, MAKAVOS G, LEKAKIS J. Arterial stiffness and coronary artery disease[J]. Curr Opin Cardiol, 2015, 30: 422-431. DOI:10.1097/HCO.0000000000000179 |
| [26] |
PERALTA C A, ADENEY K L, SHLIPAK M G, JACOBS D Jr, DUPREZ D, BLUEMKE D, et al. Structural and functional vascular alterations and incident hypertension in normotensive adults: the Multi-Ethnic Study of Atherosclerosis[J]. Am J Epidemiol, 2010, 171: 63-71. DOI:10.1093/aje/kwp319 |
| [27] |
VAN BORTEL L M, LAURENT S, BOUTOUYRIE P, CHOWIENCZYK P, CRUICKSHANK J K, DE BACKER T, et al. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity[J]. J Hypertens, 2012, 30: 445-448. DOI:10.1097/HJH.0b013e32834fa8b0 |
| [28] |
NÉMETH Z K, STUDINGER P, KISS I, OTHMANE T E H, NEMCSIK J, FEKETE B C, et al. The method of distance measurement and torso length influences the relationship of pulse wave velocity to cardiovascular mortality[J]. Am J Hypertens, 2011, 24: 155-161. DOI:10.1038/ajh.2010.220 |
| [29] |
CALABIA J, TORGUET P, GARCIA M, GARCIA I, MARTIN N, GUASCH B, et al. Doppler ultrasound in the measurement of pulse wave velocity: agreement with the Complior method[J/OL]. Cardiovasc Ultrasound, 2011, 9: 13. DOI: 10.1186/1476-7120-9-13.
|
| [30] |
BAI X, LIU W, HUANG H, YOU H. Ultrafast pulse wave velocity and ensemble learning to predict atherosclerosis risk[J/OL]. Int J Cardiovasc Imaging, 2022. DOI: 10.1007/s10554-022-02574-3.
|
| [31] |
HUANG C W, SU Y, ZHANG H, QIAN L X, LUO J W. Comparison of different pulse waveforms for local pulse wave velocity measurement in healthy and hypertensive common carotid arteries in vivo[J]. Ultrasound Med Biol, 2016, 42: 1111-1123. DOI:10.1016/j.ultrasmedbio.2015.12.021 |
| [32] |
BOUTOUYRIE P, CHOWIENCZYK P, HUMPHREY J D, MITCHELL G F. Arterial stiffness and cardiovascular risk in hypertension[J]. Circ Res, 2021, 128: 864-886. DOI:10.1161/CIRCRESAHA.121.318061 |
| [33] |
IANNARELLI N J, MACNEIL A J, DEMPSTER K S, WADE T J, O'LEARY D D. Serum MMP-3 and its association with central arterial stiffness among young adults is moderated by smoking and BMI[J/OL]. Physiol Rep, 2021, 9: e14920. DOI: 10.14814/phy2.14920.
|
| [34] |
IZUMI Y, HAYASHI M, MORIMOTO R, CHENG X W, WU H X, ISHII H, et al. Impact of circulating cathepsin K on the coronary calcification and the clinical outcome in chronic kidney disease patients[J]. Heart Vessels, 2016, 31: 6-14. DOI:10.1007/s00380-014-0570-z |
| [35] |
LI X, LI Y, JIN J, JIN D, CUI L, LI X, et al. Increased serum cathepsin K in patients with coronary artery disease[J]. Yonsei Med J, 2014, 55: 912-919. DOI:10.3349/ymj.2014.55.4.912 |
| [36] |
黄辉, 朱正球, 栾云, 王晗, 张玫玫, 刘牛, 等. 超极速超声成像脉搏波技术在早期颈动脉粥样硬化风险动态评估中的应用价值[J]. 东南大学学报(医学版), 2017, 36: 9-13. DOI:10.3969/j.issn.1671-6264.2017.01.003 |
 2022, Vol. 43
2022, Vol. 43


