2. 海军军医大学(第二军医大学)第一附属医院输血科,上海 200433
2. Department of Blood Transfusion, The First Affiliated Hospital of Naval Medical University (Second Military Medical University), Shanghai 200433, China
岛礁远离祖国大陆,地处边防一线,自然环境恶劣,守礁官兵不仅要承担繁重的战备任务,更要接受高温、高湿、高盐、强辐射、多台风等恶劣环境的挑战,这些都将对他们的身心健康产生一定的影响。提升卫勤保障能力、保障守礁官兵的身心健康对于提高部队战斗力具有重要的战略意义。本研究调查了2018年6月至2020年6月某岛礁医院耳鼻咽喉头颈外科门诊所有官兵的就诊信息,分析守礁官兵耳鼻咽喉头颈部疾病的构成情况和流行病学特征,探讨岛礁复杂环境下耳鼻咽喉头颈部疾病的发生规律,为制订针对性的卫勤保障方案、提高守礁官兵健康水平提供依据。
1 资料和方法 1.1 调查对象和方法调查对象为2018年6月至2020年6月在某岛礁医院耳鼻咽喉头颈外科门诊就诊的所有官兵,排除因非耳鼻咽喉头颈疾病而就诊者。收集信息包括性别、年龄、主诉、病情概要、就诊时间和诊断结果。参照国际疾病分类第十一次修订本(International Classification of Diseases 11th revision,ICD-11)[1]进行疾病编码分类,按耳部、鼻部、咽部、喉部及头颈部疾病进行分类,并统计各个部位所见疾病及构成比。
1.2 统计学处理采用Excel软件对原始数据进行登记录入、整理及分类统计,采用GraphPad Prism 8软件绘图。计量资料以x±s表示,计数资料以例次和百分数表示。
2 结果 2.1 病种特征分析2018年6月至2020年6月某岛礁医院耳鼻咽喉头颈外科门诊共有1 748例次官兵就诊,占岛礁医院总就诊例次的3.79%(1 748/46 121)。就诊官兵中男1 724例次、女24例次,年龄18~60(26.77±5.69)岁。由表 1可见,在1 748例次就诊记录中,耳部疾病共487例次(27.86%),诊断疾病24种,最常见的为急性外耳道炎(20.53%),其次为慢性外耳道炎(14.37%)、耵聍栓塞(11.50%)、耳鸣(9.03%)、真菌性外耳道炎(6.98%)、急性中耳炎(6.57%)、外耳道湿疹(5.95%)、耳聋(4.11%)、眩晕(3.70%)、耳部皮脂腺囊肿(3.29%)等;鼻部疾病共459例次(26.26%),诊断疾病14种,最常见的为慢性鼻炎(31.59%),其次为变应性鼻炎(29.63%)、鼻中隔偏曲(7.84%)、鼻出血(7.41%)、慢性鼻窦炎(7.19%)、急性鼻炎(5.45%)、急性鼻窦炎(4.14%)、急性鼻前庭炎(3.49%)、鼻骨骨折(1.31%)等;咽部疾病共565例次(32.32%),诊断疾病12种,最常见的为慢性咽炎(53.45%),其次为急性咽炎(29.91%)、急性扁桃体炎(8.50%)、慢性扁桃体炎(4.42%)、咽部异物(1.24%)等;喉部疾病共167例次(9.55%),诊断疾病5种,最常见的为慢性喉炎(56.89%),其次为急性喉炎(40.72%)、急性会厌炎(1.20%)等;头颈部疾病共39例次(2.23%),诊断疾病8种,最常见的为颈部淋巴结炎(46.15%),其次为颌面创伤(12.82%)、颞下颌关节紊乱综合征(12.82%)、急性腮腺炎(7.69%)、颈部创伤(7.69%)等;其他部位疾病3种,包括急性上呼吸道感染、口腔溃疡、睡眠相关呼吸障碍,累计31例次(1.77%)。
|
|
表 1 耳鼻咽喉头颈外科门诊就诊官兵各部位常见疾病 |
在耳鼻咽喉头颈外科门诊1 748例次就诊记录中,诊断疾病占前20位的分别为慢性咽炎(302例次,17.28%)、急性咽炎(169例次,9.67%)、慢性鼻炎(145例次,8.30%)、变应性鼻炎(136例次,7.78%)、急性外耳道炎(100例次,5.72%)、慢性喉炎(95例次,5.43%)、慢性外耳道炎(70例次,4.00%)、急性喉炎(68例次,3.89%)、耵聍栓塞(56例次,3.20%)、急性扁桃体炎(48例次,2.75%)、耳鸣(44例次,2.52%)、鼻中隔偏曲(36例次,2.06%)、真菌性外耳道炎(34例次,1.95%)、鼻出血(34例次,1.95%)、慢性鼻窦炎(33例次,1.89%)、急性中耳炎(32例次,1.83%)、外耳道湿疹(29例次,1.66%)、急性鼻炎(25例次,1.43%)、慢性扁桃体炎(25例次,1.43%)和耳聋(20例次,1.14%)。
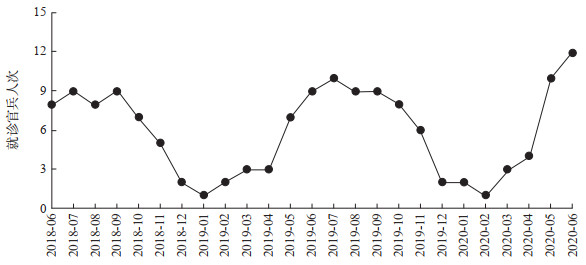
2.2 变应性鼻炎流行病学特征岛礁气候依据降水量大小可划分为雨季与旱季,雨季为每年的5月至11月,旱季为每年的12月至次年4月,变应性鼻炎就诊例次呈明显的雨季、旱季波动起伏规律(图 1)。
|
图 1 变应性鼻炎月就诊官兵例次变化趋势图 |
3 讨论
岛礁地处热带海洋季风气候,高温、高湿、高盐、强辐射、多台风,自然环境恶劣,年均气温22~28 ℃,年均湿度在80%以上,守礁官兵处于边防一线,条件较为艰苦[2-3]。本研究通过调查发现,岛礁官兵耳鼻咽喉头颈部疾病存在独有的流行病学特征,分析如下。
耳部疾病占耳鼻咽喉头颈外科门诊就诊例次的27.86%,以外耳道疾病(急慢性外耳道炎、耵聍栓塞等)最为多见。耵聍分布于外耳道软骨部,由耵聍腺和皮脂腺分泌的物质组成,含有多种抗菌蛋白及多肽,如溶菌酶、乳铁蛋白、β-防御素等[4-5]。耵聍作为保护屏障有防水、抗真菌、抗细菌的特性,在防止机械损伤和微生物入侵方面发挥重要作用[6-7]。耳部疾病高发原因主要有以下几个:(1)高温、高湿的岛礁环境抑制外耳道耵聍的分泌,降低了外耳道局部的抵抗力。(2)高温、高湿刺激外耳道,引起耳痒等不适感,岛礁官兵可能通过挖耳缓解不适,但挖耳方式不正确会造成外耳道皮肤损伤,继发感染。(3)岛礁官兵游泳训练较多,水进入外耳道并浸泡皮肤、破坏角质层,改变了局部微环境,如不洁的水进入耳内易诱发感染。(4)高湿的环境易使耵聍凝聚成块,贴覆于外耳道壁不易排出;有的官兵习惯性在出汗、洗澡后使用棉签清理耳朵内水分,将耵聍机械性内推向鼓膜,久之即形成耵聍栓塞。(5)耳鸣大多发生在打靶后,由强烈的噪声引起,多为自限性,一般1周内缓解。以上因素造成了岛礁耳部疾患发病率高,据此提出以下建议:(1)改变不良的挖耳习惯,避免使用锐利器械、棉签挖耳,减少挖耳次数。(2)游泳训练前注意泳池的消毒,训练中注意佩戴防水耳塞,训练结束后注意及时排空外耳道内水分。排空外耳道内水分的正确方法为一侧耳朵朝下,蹦跳几下,棉签置于外耳道口并吸出残余水分,保持外耳道干畅。(3)参加射击训练及处于噪声环境(如场站、电站)下的官兵注意佩戴防噪声耳塞,尽量避免久处噪声环境。
鼻部疾病占耳鼻咽喉头颈外科门诊就诊例次的26.26%,其中慢性鼻炎、变应性鼻炎占多数。其原因主要有以下几个:(1)岛礁补给困难,新鲜蔬菜水果匮乏,官兵无法从食物中获取足够维生素。维生素在维持鼻黏膜上皮的完整、腺体的分泌、特异性和非特异性免疫防御功能上发挥重要作用,维生素缺乏时鼻黏膜腺体分泌减少,纤毛脱落,局部防御功能下降,易发生感染[8]。(2)岛礁战备压力大,官兵执勤之余缺乏娱乐活动,大部分官兵抽烟。烟雾影响鼻黏膜上皮纤毛的摆动,导致血管舒缩障碍,同时腺体的分泌功能也受到影响,促进鼻腔炎症的发生、发展[9-10]。(3)鼻腔黏膜和鼻腔生理功能的维持主要依靠自主神经系统调控,需要特定的温度、湿度;当环境温度、湿度突然改变,如执勤官兵由高温、高湿的室外返回低温、低湿的空调间,温度和湿度变化幅度超出血管、腺体、神经的调节范围,将导致鼻腔黏膜和鼻腔功能紊乱,出现一系列鼻部炎症症状,如鼻塞、流清涕、打喷嚏等。长期处于这种环境将导致炎症迁延不愈,演变为慢性鼻炎[11]。(4)过敏性疾病如变应性鼻炎具有明显的发病规律,即旱季就诊例次较少,雨季就诊例次明显升高。岛礁上雨季空气湿度加大,雨量增多,蟑螂、恙螨等大量繁殖,植物花粉颗粒、真菌孢子增多,过敏原数量大量增加,使季节变应性鼻炎发病率升高[12-13]。基于上述分析,提出以下建议:(1)勤洗衣被,经常晾晒,室内保持干爽,除螨、剿灭蟑螂,杀灭动物性过敏原;雨季非执勤时患有变应性鼻炎的官兵尽量减少室外活动。(2)避免周围环境温度和湿度的骤然波动,执勤后返回室内,空调温度不宜调至过低,可逐步低幅调节室温。(3)增加维生素摄入,可口服维生素类制剂。(4)戒烟,增加业余活动,加强体育锻炼,增强抵抗力,以减少炎症性疾病的发生。
咽部疾病和喉部疾病分别占耳鼻咽喉头颈外科门诊就诊例次的32.32%和9.55%,以急慢性咽喉炎为主。原因主要有如下几个:(1)岛礁终年高温,雨后及晚上气温下降快,官兵未及时增加衣物致受凉;一些官兵执勤后喜吹冷空调、洗凉水澡而引发急性上呼吸道感染,这是造成急性咽喉炎常见原因[14]。(2)岛礁官兵普遍抽烟,是引发急慢性咽喉炎最常见的原因[15-16]。(3)官兵日常训练中,用声频繁,发音响度大、音调高,未掌握正确的发音技巧,同时训练中体内水分流失较严重,未及时补充充足的水分而导致咽喉部干燥、疼痛,这些都是导致咽喉部急慢性炎症出现的常见原因[17-18]。据此提出以下建议:(1)关注天气变化,适量增减衣物,避免上呼吸道感染的发生。(2)训练结束后不宜立即洗凉水澡,休息时空调温度不可调至过低。(3)戒烟。(4)训练中及时补充水分,养成正确的发声习惯,注意声带休息。
头颈部疾病及其他类型疾病较为少见。其中颌面创伤5例次、颈部创伤3例次,均于作业中出现,应加强相关的防护措施,提高防范意识。颞下颌关节紊乱综合征5例次,均为大量嚼食槟榔后出现。经调查发现,有的官兵有大量嚼食槟榔的习惯,大多就诊于口腔科,相关的数据仍需进一步统计调查。长期嚼食槟榔会增加患口腔癌、下咽癌、食管癌的风险[19-21],应在官兵中普及嚼食槟榔的危害相关知识,教育广大官兵摒弃陋习。
本次流行病学调查结果提示,岛礁官兵耳鼻咽喉头颈部疾病种类繁多,表现各异,病情多较复杂。根据流行病学调查结果针对性制订科学合理的卫勤保障方案,对维护守礁官兵的身心健康水平、提高部队战斗力具有重要意义。
| [1] |
World Health Organization. ICD-11: International Classification of Diseases 11th revision. The global standard for diagnostic health information[S/OL]. [2020-06-23]. https://icd.who.int/en.
|
| [2] |
刘威, 薛晨, 吕奕鹏, 葛阳, 张鹭鹭. 南海方向部分岛礁官兵卫生服务需求调查分析[J]. 第二军医大学学报, 2016, 37: 1415-1417. LIU W, XUE C, Lü Y P, GE Y, ZHANG L L. Investigation of healthcare demands of PLA soldiers in the islands of the South China Sea[J]. Acad J Sec Mil Med Univ, 2016, 37: 1415-1417. |
| [3] |
王汇, 陆小英, 王梦可. 南沙某岛礁官兵卫生服务需求调查[J]. 解放军医院管理杂志, 2019, 26: 1111-1113. |
| [4] |
YOON Y J, YOON J, LEE E J, KIM J S. Substance Pand calcitonin gene-related peptide in the glands of external auditory canal skin[J]. Clin Exp Otorhinolaryngol, 2017, 10: 321-324. DOI:10.21053/ceo.2017.00129 |
| [5] |
YOON Y J, LEE E J. Spatial distribution of antimicrobial peptides and mast cells in the skin of the external auditory canal[J/OL]. J Laryngol Otol, 2011, 125: e6. DOI: 10.1017/s0022215111002271.
|
| [6] |
KATZENELL U, HALPERIN D, DAHAN T, BARTOV N. A novel device for the evacuation of cerumen[J]. Ann Otol Rhinol Laryngol, 2019, 128: 704-707. DOI:10.1177/0003489419838545 |
| [7] |
STOECKELHUBER M, MATTHIAS C, ANDRATSCHKE M, STOECKELHUBER B M, KOEHLER C, HERZMANN S, et al. Human ceruminous gland: ultrastructure and histochemical analysis of antimicrobial and cytoskeletal components[J]. Anat Rec A Discov Mol Cell Evol Biol, 2006, 288: 877-884. |
| [8] |
ABUZEID W M, AKBAR N A, ZACHAREK M A. Vitamin D and chronic rhinitis[J]. Curr Opin Allergy Clin Immunol, 2012, 12: 13-17. DOI:10.1097/ACI.0b013e32834eccdb |
| [9] |
HISINGER-MÖLKÄNEN H, PIIRILÄ P, HAAHTELA T, SOVIJÄRVI A, PALLASAHO P. Smoking, environmental tobacco smoke and occupational irritants increase the risk of chronic rhinitis[J/OL]. World Allergy Organ J, 2018, 11: 6. DOI: 10.1186/s40413-018-0184-5.
|
| [10] |
OTTAVIANO G, MARIONI G, GIACOMELLI L, LA TORRE F B, STAFFIERI C, MARCHESE-RAGONA R, et al. Smoking and chronic rhinitis: effects of nasal irrigations with sulfurous-arsenical-ferruginous thermal water: a prospective, randomized, double-blind study[J]. Am J Otolaryngol, 2012, 33: 657-662. DOI:10.1016/j.amjoto.2012.03.002 |
| [11] |
JACOBS R, LIEBERMAN P, KENT E, SILVEY M, LOCANTORE N, PHILPOT E E. Weather/temperature-sensitive vasomotor rhinitis may be refractory to intranasal corticosteroid treatment[J]. Allergy Asthma Proc, 2009, 30: 120-127. DOI:10.2500/aap.2009.30.3206 |
| [12] |
ZIEGLMAYER P, SCHMUTZ R, LEMELL P, UNGER-MANHART N, NAKOWITSCH S, GOESSL A, et al. Fast effectiveness of a solubilized low-dose budesonide nasal spray in allergic rhinitis[J]. Clin Exp Allergy, 2020, 50: 1065-1077. |
| [13] |
SEEDAT R Y, CLAASSEN J, CLAASSEN A J, JOUBERT G. Mite and cockroach sensitisation in patients with allergic rhinitis in the free state[J]. S Afr Med J, 2010, 100: 160-163. DOI:10.7196/SAMJ.3669 |
| [14] |
GRIEF S N. Upper respiratory infections[J]. Prim Care, 2013, 40: 757-770. DOI:10.1016/j.pop.2013.06.004 |
| [15] |
ŞANLI A, BEKMEZ E, YILDIZ G, ERDOǦAN B A, YILMAZ H B, ALTIN G. Relationship between smoking and otorhinolaryngological symptoms[J]. Kulak Burun Bogaz Ihtis Derg, 2016, 26: 28-33. DOI:10.5606/kbbihtisas.2016.87059 |
| [16] |
RENNER B, MUELLER C A, SHEPHARD A. Environmental and non-infectious factors in the aetiology of pharyngitis (sore throat)[J]. Inflamm Res, 2012, 61: 1041-1052. DOI:10.1007/s00011-012-0540-9 |
| [17] |
MAHATO N B, REGMI D, BISTA M, SHERPA P. Acoustic analysis of voice in school teachers[J]. JNMA J Nepal Med Assoc, 2018, 56: 658-661. DOI:10.31729/jnma.3626 |
| [18] |
SUNDARRAJAN A, FUJIKI R B, LOERCH S E, VENKATRAMAN A, SIVASANKAR M P. Vocal loading and environmental humidity effects in older adults[J]. J Voice, 2017, 31: 707-713. DOI:10.1016/j.jvoice.2017.02.002 |
| [19] |
RIMAL J, SHRESTHA A, MAHARJAN I K, SHRESTHA S, SHAH P. Risk assessment of smokeless tobacco among oral precancer and cancer patients in eastern developmental region of Nepal[J]. Asian Pac J Cancer Prev, 2019, 20: 411-415. DOI:10.31557/APJCP.2019.20.2.411 |
| [20] |
AKHTAR S. Areca nut chewing and esophageal squamous-cell carcinoma risk in Asians: a meta-analysis of case-control studies[J]. Cancer Causes Control, 2013, 24: 257-265. DOI:10.1007/s10552-012-0113-9 |
| [21] |
BRADLEY P J. Epidemiology of hypopharyngeal cancer[J]. Adv Otorhinolaryngol, 2019, 83: 1-14. |
 2022, Vol. 43
2022, Vol. 43


