重复肾输尿管畸形为较罕见的泌尿系先天性疾病,发病率约为0.8%[1],该病可伴发输尿管开口异位、输尿管口囊肿、膀胱输尿管反流、肾盂输尿管连接处狭窄等畸形并引起相应的临床症状。既往在治疗重复肾畸形时,对无功能的半肾主要采用半肾切除术; 对有功能的半肾,则通常采用输尿管膀胱再植术或经尿道输尿管口囊肿电切术[2]。我院2013年1月至2021年6月收治了9例重复肾输尿管畸形合并半肾输尿管口囊肿所致的肾、输尿管积水病例,采用经尿道输尿管口囊肿电切术取得了较好的治疗效果,现总结如下。
1 资料和方法 1.1 临床资料9例患者中女8例、男1例,年龄13~50岁,平均年龄(29.6±14.0)岁。6例因腰部酸痛、排尿困难、尿路感染等症状就诊(其中腰部酸痛3例,排尿中断、排尿困难1例,长期反复尿路感染2例); 3例无明显症状,于健康体检时发现。9例患者术前均行泌尿系超声、静脉尿路造影(intravenous urography,IVU)、泌尿系增强CT尿路成像(CT urography,CTU)及膀胱镜检查,确诊为伴有输尿管口囊肿的重复肾、输尿管畸形及上半肾、下半肾或输尿管积水。囊肿最大为6.0 cm×4.8 cm,最小为1.0 cm×1.2 cm。9例患者中有8例为上半肾病变,1例为下半肾病变。3例患者病变半肾积水程度为3~5 cm,5例患者积水为2~3 cm,1例患者积水为1.5 cm; 左侧6例,右侧3例。2例异位输尿管口囊肿开口于三角区,3例开口于患侧正常输尿管口处偏中间,2例开口于膀胱颈口,2例开口于尿道。
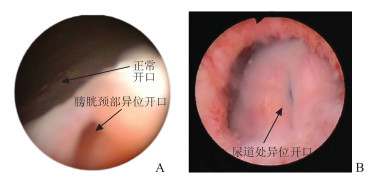
1.2 手术方法9例患者均接受全身麻醉下经尿道输尿管口囊肿切除术治疗。术者使用F24和F26奥林巴斯电切镜,电切功率120~150 W,电凝功率80~120 W。术中进镜后首先观察尿道及三角区是否有异常开口,然后在三角区明确健侧输尿管开口位置,仔细观察尿道、膀胱颈口及膀胱壁各个部位,找到异常输尿管开口(图 1)及囊肿位置,用电切环切除远侧隆起囊壁,完全暴露输尿管口,头侧囊壁予以保留,以形成半覆盖瓣膜。其中3例予以膀胱镜下留置双J管,彻底止血,留置F24三腔气囊导尿管,术后持续膀胱冲洗。
|
图 1 术中膀胱镜下图片 A:术中见输尿管口囊肿异位开口于膀胱颈; B:术中见输尿管口囊肿异常开口于尿道. |
2 结果
9例患者手术均一次成功,手术时间20~40 min,平均(28.3±7.5)min; 术中出血均少于20 mL; 术后膀胱冲洗,引流液颜色清亮,所有患者均于术后24 h内停止膀胱冲洗。术后第2天行腹部X线片检查,3例患者的双J管均留置在位。所有患者均于术后2~3 d拔除导尿管,术后住院(2.4±1.6)d。术后6~8周拔除双J管。随访1~24个月,复查超声,所有患者肾积水均减轻,仅有3例患者仍有轻度积水,未出现腰酸、腰痛、排尿困难等症状,尿路感染未见复发。其中1例半肾无功能(患侧半肾积水5.0 cm)且伴发复杂尿路感染的患者术后症状完全消失。见表 1。
|
|
表 1 9例重复肾输尿管畸形合并半肾输尿管口囊肿患者一般资料及围手术期情况 |
3 讨论
重复肾畸形是一种少见的先天性泌尿系疾病[3],患肾由于胚胎发育异常存在两套肾盂输尿管系统,通过一条浅沟分为上半肾及下半肾,但有共同的被膜。重复肾畸形可分为完全性重复肾和不完全性重复肾,前者绝大多数符合Weigert-Meyer定律,下输尿管口靠头侧及外侧,而上输尿管口靠内侧及下方,多表现为上位肾发育不良或积水。完全性重复肾畸形常同时伴有输尿管口囊肿、输尿管异位开口及膀胱输尿管反流等畸形。
输尿管口囊肿又称输尿管膨出,是输尿管末端的囊性扩张,分为正位输尿管口囊肿及异位输尿管口囊肿,异位输尿管口囊肿多伴重复肾输尿管畸形,80%的输尿管口囊肿并发于重复肾畸形的上肾部[4],多异位于膀胱颈部或尿道。发生原因多由于先天胚胎发育异常导致输尿管口闭塞或狭窄所引起的继发性改变[5],并可由囊肿的大小及伴或不伴有周围膀胱壁的薄弱或局部炎症情况出现膀胱输尿管反流[4]。
重复肾输尿管畸形多发于女性,患者常因出现腰背酸痛、反复尿路感染、排尿异常甚至尿失禁等症状就诊。目前,对于输尿管口囊肿导致的重复肾输尿管梗阻及肾积水的诊断主要依据超声、IVU、CTU或磁共振尿路成像(magnetic resonance urography,MRU)及膀胱镜检查。超声可显示积水程度,IVU可显示整个尿路系统形态,有助于了解输尿管口的位置、囊肿大小及分肾功能。当梗阻及发育不良导致病变半肾不显影时,可行CTU及MRU检查,从而准确诊断及进行尿路系统重建。膀胱镜检查可以明确囊肿的位置、大小、正常及异位输尿管开口位置,有助于协助术前手术方案的制定。此外,放射性核素肾图检查可评估双肾功能,为手术方式的选择提供依据。
对无临床症状的重复肾畸形,可暂不行手术治疗,采取动态观察; 但对重复肾输尿管畸形伴输尿管口囊肿引起肾积水及出现反复发作的泌尿系感染等其他症状的患者,常需行外科手术治疗。手术方式主要有输尿管膀胱再植术、半肾切除术、经尿道输尿管口囊肿电切术等。开放或腹腔镜下切除病变半肾及相应的肾盂输尿管等传统治疗重复肾畸形的方法主要存在以下不足:(1)创伤较大; (2)部分患者由于长期炎症、积水导致局部粘连,手术视野小,且术中组织分离困难,容易损伤、误扎健侧半肾血管和输尿管,导致术中、术后出血,术后输尿管狭窄; (3)术中由于缝扎正常的半肾过多,导致剩余肾实质供血不良、缺血; (4)部分患者因切除不完全出现尿瘘、尿性囊肿等。
目前对无功能的上肾单位是否保留仍有争议。重复肾畸形的症状主要来源于输尿管口囊肿、异位开口所致的梗阻、反流、结石、尿路感染,而畸形的上半肾本身并不会导致功能性紊乱,肾积水是梗阻、反流所导致的继发性改变。Le等[6]认为无功能的上肾单位可以保留,因为它并不会导致并发症的发生; 但Dönmez等[7]认为上位肾无功能,反复尿路感染或同侧腹痛即为切除指征。本研究对9例伴有输尿管口囊肿的重复肾输尿管畸形及上半肾或输尿管积水的患者行经尿道输尿管口囊肿电切术,术后积水情况均得到明显改善,且1例半肾无功能且伴发复杂尿路感染的患者术后症状完全消失。这提示经尿道输尿管口囊肿电切术不仅对有功能半肾的积水有效,而且对无功能半肾积水的反复感染同样有效。因此,术者认为对于大部分患者尤其是患肾仍存在有功能肾皮质的患者可优先考虑该术式。同样,Sander等[8]和Jesus等[9]也认为内镜下输尿管口囊肿电切术能够有效控制泌尿系感染,降低膀胱出口梗阻的发生率。
经尿道输尿管口囊肿电切术能够对输尿管口囊肿进行结构整复达到良好的治疗效果,且具有术式简单、损伤小、无明显并发症、住院时间短、患者接受度好、术后患者恢复良好等优点,若术后病情未得到有效控制,仍有进一步手术的机会。但经该术式治疗后,还可能有一定的复发率,且囊肿壁越厚复发率越高。一部分原因是囊壁切开不足导致的重新愈合[10],当然也可因为切开范围过大而引起膀胱输尿管反流,导致肾积水复发。尽管如此,经尿道输尿管口囊肿电切术可去除输尿管口囊肿这一直接病因对上尿路所致的进一步损伤,解除梗阻,并为后续进一步治疗提供条件,尤其是对感染导致脓毒血症的患者。因此,经尿道输尿管口囊肿电切术是治疗伴有输尿管口囊肿的重复肾输尿管畸形及上半肾或输尿管积水患者的优先术式。
对此术式总结如下:(1)术前明确诊断,根据术前影像学资料,区分完全性或不完全性重复肾畸形,明确输尿管口囊肿及异位开口,对输尿管开口于尿道括约肌内的囊肿且患肾存在有功能肾皮质的患者,电切可列为优先选择的手术方式。(2)术中保持膀胱适当充盈,避免过度充盈影响对输尿管口囊肿的定位,找出正常输尿管开口及异位输尿管开口,后者多位于膀胱颈部、三角区、尿道,部分患者异位开口位于囊肿内基底部,易被忽略。手术过程中必须有足够的耐心,观察正常及异常输尿管开口的喷尿情况。术中需切开囊壁全层,充分暴露输尿管口,避免囊壁的愈合导致复发,同时应避免损伤正常输尿管开口。(3)术中电切时注意对较大的囊肿可切除部分远端低位囊壁,保留近侧高位囊壁使之形成抗反流活瓣,保护好输尿管抗反流机制,而对于较小的囊肿甚至可切除全部囊壁以避免术后瘢痕愈合导致输尿管口狭窄。(4)对内镜治疗后效果欠佳、上位肾无功能、积脓或反复感染的患者,可行半肾输尿管切除术。
| [1] |
DE CALUWE D, CHERTIN B, PURI P. Fate of the retained ureteral stump after upper pole heminephrectomy in duplex kidneys[J]. J Urol, 2002, 168: 679-680. DOI:10.1016/S0022-5347(05)64722-2 |
| [2] |
DIDIER R A, CHOW J S, KWATRA N S, RETIK A B, LEBOWITZ R L. The duplicated collecting system of the urinary tract: embryology, imaging appearances and clinical considerations[J]. Pediatr Radiol, 2017, 47: 1526-1538. DOI:10.1007/s00247-017-3904-z |
| [3] |
杨宏伟, 易发现. 重复肾输尿管合并输尿管囊肿的诊疗进展[J]. 临床外科杂志, 2019, 27: 1007-1010. DOI:10.3969/j.issn.1005-6483.2019.11.027 |
| [4] |
吴阶平. 吴阶平泌尿外科学[M]. 济南: 山东科学技术出版社, 2019: 959.
|
| [5] |
FARROKH D. Early diagnosis of congenital ureterocele[J]. J Belge Radiol, 1992, 75: 25-28. |
| [6] |
LE H K, CHIANG G. Long-term management of ureterocele in duplex collecting systems: reconstruction implications[J/OL]. Curr Urol Rep, 2018, 19: 14. DOI: 10.1007/s11934-018-0758-3.
|
| [7] |
DÖNMEZ M I, YAZICI M S, ABAT D, KARA Ö, BAYAZIT Y, BILEN C Y. Laparoscopic upper pole heminephrectomy in adults for treatment of duplex kidneys[J]. Urol J, 2015, 12: 2074-2077. |
| [8] |
SANDER J C, BILGUTAY A N, STANASEL I, KOH C J, JANZEN N, GONZALES E T, et al. Outcomes of endoscopic incision for the treatment of ureterocele in children at a single institution[J]. J Urol, 2015, 193: 662-666. DOI:10.1016/j.juro.2014.08.095 |
| [9] |
JESUS L E, FARHAT W A, AMARANTE A C M, DINI R B, LESLIE B, BÄGLI D J, et al. Clinical evolution of vesicoureteral reflux following endoscopic puncture in children with duplex system ureteroceles[J]. J Urol, 2011, 186: 1455-1458. DOI:10.1016/j.juro.2011.05.057 |
| [10] |
ADORISIO O, ELIA A, LANDI L C, TAVERNA M, MALVASIO V, DANTI A D. Effectiveness of primary endoscopic incision in treatment of ectopic ureterocele associated with duplex system[J]. Urology, 2011, 77: 191-194. DOI:10.1016/j.urology.2010.02.061 |
 2022, Vol. 43
2022, Vol. 43


