颈内动脉串联病变是指颅内大血管闭塞合并同侧颈内动脉颅外段重度狭窄或闭塞病变,此类患者占急性缺血性脑卒中的10%~15%[1]。与单纯的急性颅内大血管闭塞相比,颈内动脉串联病变患者的预后更差、致残率和死亡率更高,若闭塞血管不能及时、有效再通,总死亡率可达55%[2]。颈内动脉串联病变的手术策略根据病变处理的先后次序分为优先远端取栓和优先颈动脉支架植入2种,采用哪种治疗方式的患者临床预后更优存在一定争议[3]。先处理颅内动脉闭塞病变能最大限度地缩短血管再通时间,但是在治疗颈内动脉颅外段病变的时候有可能发生颅内动脉再次闭塞;若优先处理颈内动脉颅外段病变则延长了血管再通时间。本研究回顾性分析接受颅内动脉机械取栓同期颈动脉支架植入治疗的颈内动脉串联病变所致急性缺血性脑卒中患者资料,观察其治疗效果。
1 资料和方法 1.1 研究对象回顾性选择2019年1月至2020年12月在聊城市人民医院脑科医院神经外科就诊的前循环急性缺血性脑卒中患者376例。纳入标准:(1)急性缺血性脑卒中的诊断符合《中国急性缺血性脑卒中诊治指南2018》[4]中诊断标准,且术中全脑血管造影检查证实前循环颅内动脉闭塞合并同侧颈内动脉起始部重度狭窄或闭塞;(2)年龄≥18岁;(3)发病至股动脉穿刺时间 < 6 h;(4)入院时美国国立卫生研究院卒中量表(National Institutes of Health stroke scale,NIHSS)评分≥6分;(5)发病前改良Rankin量表(modified Rankin scale,mRS)评分 < 2分;(6)患者或其家属对手术方案及治疗风险充分知情并签署手术知情同意书。
1.2 研究方法将入组患者根据血管内治疗处理策略分为由远及近组和由近及远组。
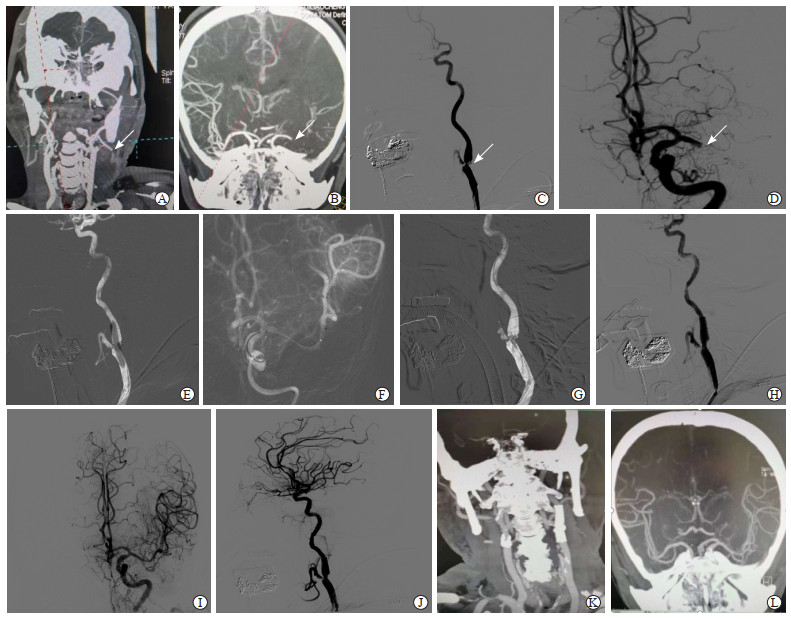
1.2.1 血管内治疗(1) 由远及近组:患者取仰卧位,予经口气管插管全身麻醉。经股动脉置入8 F短动脉鞘(日本Terumo公司),泥鳅导丝导引8 F导引导管(美国Boston Scientific公司)、5 F中间导管(美国EV3公司)到达患侧颈总动脉分叉附近。首先尝试将中间导管通过颈内动脉起始部重度狭窄或闭塞段,若未成功,则在路图下由微导管辅助微导丝通过颈内动脉起始段重度狭窄或闭塞段,然后沿微导丝送入球囊扩张导管,扩张颈内动脉起始段狭窄或闭塞段。球囊扩张后将中间导管通过颈内动脉起始段到达颈内动脉颅内段,由Traxcess 14微导丝(美国MicroVention公司)辅助Rebar-18微导管(美国EV3公司)通过颅内动脉闭塞段到达远端正常管腔。释放Solitaire FR取栓支架(美国EV3公司)覆盖闭塞病变处,停留5 min后,在支架锚定装置协助下操作Navien导管继续前进并保持负压抽吸,缓慢回撤取栓支架及中间导管至导引导管内。机械取栓操作结束后立即行患侧颈内动脉造影,若血管未开通则重复上述取栓操作。确认远端血管通畅后,将Navien导管置于颈内动脉岩段垂直部分,沿Navien导管释放Spider FX 5.0远端栓塞保护装置(美国EV3公司),根据颈内动脉起始部狭窄程度决定是否需要行球囊预扩张。然后置入Protege RX颈动脉支架(美国EV3公司),根据支架形态及支架植入术后颈内动脉起始部残余狭窄的严重程度决定是否予球囊再扩张。最后进行造影检查,采用改良脑梗死溶栓(modified thrombolysis in cerebral infarction,mTICI)分级评估血管再通情况,结束手术(图 1)。
|
图 1 1例采用由远及近行机械取栓+支架植入术的左侧颈内动脉串联病变患者的影像学资料 Fig 1 Imaging data of a patient with tandem lesions of left internal carotid artery undergoing mechanical thrombectomy+stent implantation from distal to proximal A 62-year-old male patient suffered from a sudden aphasia and was unable to move his right limbs for 2 h. The pre-onset modified Rankin scale score was 0, and the baseline National Institutes of Health stroke scale score was 19. A: Preoperative CTA confirming the left internal carotid artery occlusion (arrow); B: Preoperative CTA showing occlusion of the M1 segment of left middle cerebral artery (arrow); C: Intraoperative angiography showing extremely severe stenosis of the left internal carotid artery (arrow); D: Intraoperative angiography showing occlusion of the left middle cerebral artery (arrow); E: Balloon dilation of the carotid bulb; F: Stent thrombus removal in the left middle cerebral artery; G: Balloon dilation of the start of internal carotid artery under the distal protection device; H: Carotid stent implantation; I: Angiography showed that the left middle cerebral artery was unobstructed; J: Angiography showed that the left internal carotid artery was unobstructed; K: Postoperative CTA showed that the left internal carotid artery was unobstructed; L: CTA after operation showed that the left middle cerebral artery was unobstructed. CTA: Computed tomography angiography. |
(2) 由近及远组:患者先在颈内动脉起始部重度狭窄或闭塞段植入支架,然后应用取栓支架在颅内动脉闭塞处行机械取栓操作,支架植入和取栓具体操作同由远及近组。
1.2.2 围手术期药物治疗(1) 静脉溶栓:对于发病4.5 h内的患者,由术者决定是否予阿替普酶静脉溶栓治疗,剂量为0.9 mg/kg;发病4.5~6 h的患者直接行血管内治疗。(2)术后用药情况:对于术中Dyna-CT检查未见明显造影剂渗出或渗出较少的患者,术后予替罗非班0.25~0.3 mg/L静脉泵入,停用替罗非班4 h前口服负荷剂量双联抗血小板聚集药物(阿司匹林300 mg+硫酸氢氯吡格雷300 mg),之后予阿司匹林100 mg+硫酸氢氯吡格雷75 mg口服,每天1次,3个月后根据血栓弹力图结果调整为单药终身服用。术后24 h复查头颅CT,如发生症状性颅内出血则立即停用抗血小板聚集药物。
1.2.3 疗效、评价指标及随访主要评价指标为术中1次取栓成功率、术后90 d预后良好(mRS评分≤2分)率,次要评价指标包括血管成功再通(mTICI分级≥2b级)率、术后24 h NIHSS评分、术后7 d NIHSS评分、发病至股动脉穿刺时间、股动脉穿刺至血管再通时间、术后症状性颅内出血发生率、术后90 d死亡率等。除住院期间临床死亡患者外,其余均完成术后90 d随访。
1.3 统计学处理应用SPSS 22.0软件进行统计学分析。符合正态分布的计量资料以x±s表示,两组间比较采用独立样本t检验;计数资料以例数和百分数表示,两组间比较采用χ2检验或Fisher确切概率法。检验水准(α)为0.05。
2 结果 2.1 两组患者基线资料比较共55例颈内动脉串联病变所致急性缺血性脑卒中患者入组,其中男35例、女20例,年龄为35~82岁,平均年龄为(63.17±10.40)岁。合并糖尿病患者11例,合并高血压患者17例,合并高脂血症患者28例,有吸烟史患者23例。55例患者发病前mRS评分均 < 2分。31例接受静脉溶栓桥接血管内治疗,24例直接行血管内治疗。由远及近组43例,由近及远组12例,两组患者性别、年龄、脑卒中危险因素、入院时NIHSS评分、行静脉溶栓患者占比、血管闭塞部位、发病至股动脉穿刺时间差异均无统计学意义(P均>0.05)。见表 1。
|
|
表 1 两组颈内动脉串联病变所致急性缺血性脑卒中患者的基线资料比较 Tab 1 Comparison of baseline data of patients with acute ischemic stroke caused by internal carotid artery tandem lesions between 2 groups |
2.2 两组患者治疗效果比较
所有患者均顺利完成颅内动脉闭塞处机械取栓及颈内动脉起始部重度狭窄或闭塞段支架植入术。由远及近组患者1次取栓成功率高于由近及远组,股动脉穿刺至血管再通时间短于由近及远组,差异均有统计学意义(P均 < 0.05)。而两组患者术后即刻血管成功再通率、术后症状性颅内出血发生率、术后24 h NIHSS评分、术后7 d NIHSS评分、术后90 d预后良好率和死亡率差异均无统计学意义(P均>0.05)。见表 2。
|
|
表 2 两组颈内动脉串联病变所致急性缺血性脑卒中患者的治疗效果比较 Tab 2 Comparison of therapeutic effects of patients with acute ischemic stroke caused by internal carotid artery tandem lesions between 2 groups |
3 讨论
急性颈内动脉串联病变患者同时存在近端颈内动脉病变和远端颅内动脉病变,是急性缺血性脑卒中的一个较为复杂的类型,此类患者行单纯静脉溶栓治疗的血管成功再通率仅为9%,预后良好率仅为20%,而死亡率高达55%[5],可能是因为血栓负荷较大、顺行血流量较少,使溶栓药物难以到达颅内血栓处。HERMES研究表明颈内动脉串联病变导致的急性缺血性脑卒中行静脉溶栓联合机械取栓术的治疗效果优于单纯静脉溶栓[6],还有多项研究详细分析了血管内治疗串联病变的有效性和安全性,但对于串联病变血管内治疗的手术策略尚无统一意见[7-9]。
目前针对颈内动脉串联病变的手术策略分为优先处理近端病变(由近及远)和优先处理远端病变(由远及近),2种方式各有优缺点。由近及远的手术策略先行颈内动脉起始部支架植入使颈内动脉血流恢复后,再行颅内动脉闭塞机械取栓术,该术式的优点是可以建立良好的血管通路,能避免在颅内动脉取栓后进行颈内动脉手术操作时出现颅内血管再次闭塞的可能,但是也存在近端血流恢复后远端栓子逃逸的风险,并且近端病变优先处理使远端血管再通时间延长,可能会引起更大面积的梗死灶。而优先处理远端病变即先开通颅内动脉闭塞段,如果颈内动脉起始部闭塞或重度狭窄,中间导管无法通过时,可先予球囊扩张,待颅内动脉血流恢复后再行颈内动脉支架植入,这一方式能使远端血管快速再通,但是手术难度相对较高,在建立血管通路时可能会导致血液进入血管壁甚至发生动脉夹层和血管穿孔。一篇meta分析显示2种手术方案在血管成功再通率、术后症状性颅内出血发生率、术后90 d预后良好率方面差异均无统计学意义[10];也有研究表明先处理颅内动脉病变再处理颈内动脉颅外段病变的手术方案在血管成功再通率、并发症发生率方面优于先处理颈内动脉颅外段病变再处理颅内动脉病变[11]。针对颈内动脉串联病变的手术策略,有学者总结提出了PEARS(protect-expand-aspiration-revascularization-stent)技术[12]和Double PT(pass-thrombectomy-protective thrombectomy)技术[13],但是针对串联病变的最佳手术方案仍未达成共识[14]。本研究中多数患者采取先远后近的逆向开通策略,即采用球囊扩张颈内动脉起始部闭塞或重度狭窄段后推送导引导管通过狭窄或闭塞段,此时颈内动脉无正向血流,起到了防止远端栓子逃逸的作用,且Navien导管跟进后予负压抽吸能有效地清除颈内动脉起始部脱落的栓子和血栓组织;然后予颅内动脉机械取栓操作,取栓后撤除微导丝微导管级取栓支架、保留Navien导管,沿Navien导管输送保护伞到达颈内动脉岩段垂直部分保护伞到位后撤除Navien导管,再沿保护伞推送杆送入球囊,予狭窄处预扩张;最后释放颈动脉支架,若支架打开不良、残余狭窄较严重,可再次予球囊扩张。
颈内动脉串联病变所致急性缺血性脑卒中患者行血管内治疗时,无论由远及近开通还是由近及远开通,缺血再灌注时间都是影响预后的主要因素,越短的再灌注时间意味着更好的预后。在一项纳入25例颈内动脉串联闭塞患者的研究中,优先处理颅内病变组血管再通时间较优先处理颅外病变组短[(43±31)min vs (111±43)min,P < 0.001],但是两组患者的预后差异无统计学意义,这可能和样本量较小、存在抽样误差有关[15]。本研究中两组患者术中均未发生远端血管开通后再闭塞,但与由近及远组相比,由远及近组患者的1次取栓成功率更高、股动脉穿刺至血管再通时间更短,能更快地达到血管再通。
远端血管机械取栓成功后否需要同期植入颈动脉支架存在争议,因为急性期支架植入后,为避免支架内血栓形成需立即给予负荷剂量抗血小板聚集药物治疗,这可能会增加颅内出血的风险,尤其当患者在接受静脉溶栓治疗后。Heck和Brown[16]研究报道急诊颈内动脉支架植入术后患者应用抗血小板聚集药物治疗,其症状性颅内出血发生率高达22%。然而有研究提示,对于急性缺血性脑卒中患者动脉内溶栓后行急诊支架植入术是安全、有效的[17]。Broeg-Morvay等[18]研究表明,急诊支架植入术治疗颈内动脉串联闭塞并未增加症状性颅内出血的发生率。也有研究显示同期植入颈动脉支架的患者预后良好率较分期植入者更高,但是在术后死亡率和症状性颅内出血发生率方面无明显差异[19]。中国ACTUAL注册研究中症状性颅内出血发生率为16.0%[20]。白永杰等[21]回顾性分析了124例颈内动脉串联闭塞患者资料,机械取栓术后症状性颅内出血发生率为15.3%。本研究中由远及近组术后症状性颅内出血发生率为14.0%(6/43),由近及远组为16.7%(2/12),总体病例症状性颅内出血发生率为14.5%(8/55),与上述研究结果相近,提示前循环颈内动脉串联病变患者行机械取栓同期颈动脉支架植入不会增加术后出血风险。
颈内动脉串联病变患者行血管内治疗围手术期的药物治疗方案目前也存在争议,TITAN研究纳入369例行机械取栓术的颈内动脉串联闭塞患者,发现接受抗血小板药物治疗的患者术后90 d死亡率更低,血管成功再通率更高,但术后脑出血发生率并未增加[1],Pop等[22]研究发现联合应用阿司匹林和硫酸氢氯吡格雷双重抗血小板药物能显著降低支架植入术后支架内血栓形成的发生率,且对于颈动脉支架植入术后患者,大部分临床中心均给予双联抗血小板药物治疗。本研究入组患者术后24 h均行头颅CT检查,无颅内出血给予双联抗血小板药物治疗(阿司匹林100 mg+硫酸氢氯吡格雷75 mg每天1次口服),发生非症状性颅内出血的患者的一般情况下采取单一抗血小板药物,术后若发生症状性颅内出血则立即停用抗血小板药物。
同期在我院行机械取栓治疗的非串联闭塞患者共321例,218例行静脉溶栓桥接机械取栓治疗,1次取栓成功率为75%,发病至股动脉穿刺时间为(231.26±60.20)min,股动脉穿刺至血管再通时间为(52.34±20.60)min,术后即刻血管成功再通率为93%,术后90 d预后良好率为56%、死亡率为12%,症状性颅内出血发生率为15%(未发表资料),与本研究中串联病变病例的治疗效果相当。本研究中血管成功再通率、症状性颅内出血发生率、术后90 d预后良好率也与文献[23-24]报道相近,但术后死亡率更低,这可能和入组病例数少、取栓评估剔除了一部分症状严重的病例有关。
综上所述,颅内动脉机械取栓联合颈动脉支架植入治疗颈内动脉串联病变所致急性缺血性脑卒中时,不论采取由近及远还是由远及近手术策略都是安全、有效的,但采取由远及近的手术策略能获得更高的1次取栓成功率且能更快地实现血管再通。但本研究采取回顾性分析,病例数较少且缺少随机化对照,结果有一定局限性,对急性颈内动脉串联病变患者的最佳治疗方案仍需进一步探索。
| [1] |
ZHU F, BRACARD S, ANXIONNAT R, DERELLE A L, TONNELET R, LIAO L, et al. Impact of emergent cervical carotid stenting in tandem occlusion strokes treated by thrombectomy: a review of the TITAN collaboration[J/OL]. Front Neurol, 2019, 10: 206. DOI: 10.3389/fneur.2019.00206.
|
| [2] |
RUBIERA M, RIBO M, DELGADO-MEDEROS R, SANTAMARINA E, DELGADO P, MONTANER J, et al. Tandem internal carotid artery/middle cerebral artery occlusion: an independent predictor of poor outcome after systemic thrombolysis[J]. Stroke, 2006, 37: 2301-2305. DOI:10.1161/01.STR.0000237070.80133.1d |
| [3] |
BERKHEMER O A, BORST J, KAPPELHOF M, YOO A J, VAN DEN BERG L A, FRANSEN P S S, et al. Extracranial carotid disease and effect of intra-arterial treatment in patients with proximal anterior circulation stroke in MR CLEAN[J]. Ann Intern Med, 2017, 166: 867-875. DOI:10.7326/M16-1536 |
| [4] |
中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国急性缺血性脑卒中诊治指南2018[J]. 中华神经科杂志, 2018, 51: 666-682. DOI:10.3760/cma.j.issn.1006-7876.2018.09.004 |
| [5] |
POWERS W J, DERDEYN C P, BILLER J, COFFEY C S, HOH B L, JAUCH E C, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association[J]. Stroke, 2015, 46: 3020-3035. DOI:10.1161/STR.0000000000000074 |
| [6] |
GOYAL M, MENON B K, VAN ZWAM W H, DIPPEL D W, MITCHELL P J, DEMCHUK A M, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials[J]. Lancet, 2016, 387: 1723-1731. DOI:10.1016/S0140-6736(16)00163-X |
| [7] |
BERKHEMER O A, FRANSEN P S S, BEUMER D, VAN DEN BERG L A, LINGSMA H F, YOO A J, et al. A randomized trial of intraarterial treatment for acute ischemic stroke[J]. N Engl J Med, 2015, 372: 11-20. DOI:10.1056/NEJMoa1411587 |
| [8] |
SAVER J L, GOYAL M, BONAFE A, DIENER H C, LEVY E I, PEREIRA V M, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke[J]. N Engl J Med, 2015, 372: 2285-2295. DOI:10.1056/NEJMoa1415061 |
| [9] |
HAUSSEN D C, TURJMAN F, PIOTIN M, LABREUCHE J, STEGLICH-ARNHOLM H, HOLTMANNSPÖTTER M, et al. Head or neck first? Speed and rates of reperfusion in thrombectomy for tandem large vessel occlusion strokes[J]. Interv Neurol, 2020, 8: 92-100. |
| [10] |
WILSON M P, MURAD M H, KRINGS T, PEREIRA V M, O'KELLY C, REMPEL J, et al. Management of tandem occlusions in acute ischemic stroke-intracranial versus extracranial first and extracranial stenting versus angioplasty alone: a systematic review and meta-analysis[J]. J Neurointerv Surg, 2018, 10: 721-728. DOI:10.1136/neurintsurg-2017-013707 |
| [11] |
BEHME D, MOLINA C A, SELIM M H, RIBO M. Emergent carotid stenting after thrombectomy in patients with tandem lesions[J]. Stroke, 2017, 48: 1126-1128. DOI:10.1161/STROKEAHA.117.016182 |
| [12] |
YI T Y, CHEN W H, WU Y M, ZHANG M F, LIN D L, LIN X H. Another endovascular therapy strategy for acute tandem occlusion: protect-expand-aspiration-revascularization-stent (PEARS) technique[J/OL]. World Neurosurg, 2018, 113: e431-e438. DOI: 10.1016/j.wneu.2018.02.052.
|
| [13] |
CHEN W H, YI T Y, WU Y M, ZHANG M F, LIN D L, LIN X H. Endovascular therapy strategy for acute embolic tandem occlusion: the pass-thrombectomy-protective thrombectomy (double PT) technique[J/OL]. World Neurosurg, 2018, 120: e421-e427. DOI: 10.1016/j.wneu.2018.08.096.
|
| [14] |
JACQUIN G, POPPE A Y, LABRIE M, DANEAULT N, DESCHAINTRE Y, GIOIA L C, et al. Lack of consensus among stroke experts on the optimal management of patients with acute tandem occlusion[J]. Stroke, 2019, 50: 1254-1256. DOI:10.1161/STROKEAHA.118.023758 |
| [15] |
LOCKAU H, LIEBIG T, HENNING T, NEUSCHMELTING V, STETEFELD H, KABBASCH C, et al. Mechanical thrombectomy in tandem occlusion: procedural considerations and clinical results[J]. Neuroradiology, 2015, 57: 589-598. DOI:10.1007/s00234-014-1465-5 |
| [16] |
HECK D V, BROWN M D. Carotid stenting and intracranial thrombectomy for treatment of acute stroke due to tandem occlusions with aggressive antiplatelet therapy may be associated with a high incidence of intracranial hemorrhage[J]. J Neurointerv Surg, 2015, 7: 170-175. DOI:10.1136/neurintsurg-2014-011224 |
| [17] |
王斌, 王亚冰, 李慎茂, 朱凤水, 吉训明, 焦力群, 等. 动脉溶栓联合血管成形术治疗急性缺血性卒中的单中心研究[J]. 中国脑血管病杂志, 2011, 8: 65-69. DOI:10.3969/j.issn.1672-5921.2011.02.003 |
| [18] |
BROEG-MORVAY A, MORDASINI P, SLEZAK A, LIESIROVA K, MEISTERERNST J, SCHROTH G, et al. Does antiplatelet therapy during bridging thrombolysis increase rates of intracerebral hemorrhage in stroke patients?[J/OL]. PLoS One, 2017, 12: e0170045. DOI: 10.1371/journal.pone.0170045.
|
| [19] |
GORY B, PIOTIN M, HAUSSEN D C, STEGLICH-ARNHOLM H, HOLTMANNSPÖTTER M, LABREUCHE J, et al. Thrombectomy in acute stroke with tandem occlusions from dissection versus atherosclerotic cause[J]. Stroke, 2017, 48: 3145-3148. DOI:10.1161/STROKEAHA.117.018264 |
| [20] |
HAO Y, YANG D, WANG H, ZI W, ZHANG M, GENG Y, et al. Predictors for symptomatic intracranial hemorrhage after endovascular treatment of acute ischemic stroke[J]. Stroke, 2017, 48: 1203-1209. DOI:10.1161/STROKEAHA.116.016368 |
| [21] |
白永杰, 张帅, 李顺, 尚贤金, 资文杰, 段佩养, 等. 前循环串联性闭塞所致急性缺血性卒中患者血管内机械血栓切除术后的有症状颅内出血: 预测因素和对转归的影响[J]. 国际脑血管病杂志, 2019, 27: 401-407. DOI:10.3760/cma.j.issn.1673-4165.2019.06.001 |
| [22] |
POP R, ZINCHENKO I, QUENARDELLE V, MIHOC D, MANISOR M, RICHTER J S, et al. Predictors and clinical impact of delayed stent thrombosis after thrombectomy for acute stroke with tandem lesions[J]. AJNR Am J Neuroradiol, 2019, 40: 533-539. |
| [23] |
SALLUSTIO F, MOTTA C, KOCH G, PIZZUTO S, CAMPBELL B C, DIOMEDI M, et al. Endovascular stroke treatment of acute tandem occlusion: a single-center experience[J]. J Vasc Interv Radiol, 2017, 28: 543-549. DOI:10.1016/j.jvir.2017.01.007 |
| [24] |
GRIGORYAN M, HAUSSEN D C, HASSAN A E, LIMA A, GROSSBERG J, REBELLO L C, et al. Endovascular treatment of acute ischemic stroke due to tandem occlusions: large multicenter series and systematic review[J]. Cerebrovasc Dis, 2016, 41: 306-312. DOI:10.1159/000444069 |
 2022, Vol. 43
2022, Vol. 43


